J.ophthalmol.(Ukraine).2018;2:34-39.
|
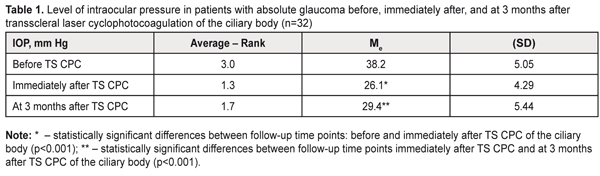
https://doi.org/10.31288/oftalmolzh/2018/2/34-39 Efficacy of transscleral Nd:YAG laser cyclophotocoagulation and changes in blood circulation in the eye of patients with absolute glaucoma P. P. Chechin, Cand. Sc. (Med.); O.V. Guzun, Cand. Sc. (Med.); N. I. Khramenko, Cand. Sc. (Med.); O. A. Peretyagin, Cand. Sc. (Med.) SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”; Odessa (Ukraine) E-mail: olga.v.guzun@gmail.com TO CITE THIS ARTICLE: Chechin PP, Guzun OV, Khramenko NI, Peretyagin OA. Efficacy of transscleral Nd:YAG laser cyclophotocoagulation and changes in blood circulation in the eye of patients with absolute glaucoma. J.ophthalmol.(Ukraine).2018;2:34-9. https://doi.org/10.31288/oftalmolzh/2018/2/34-39 Background. Absolute glaucoma is a disease which is caused by a range of different factors and which refers to a most severe ophthalmic pathology. Treatment of absolute glaucoma is often insufficient to manage pain and to decrease intraocular pressure. The purpose. To study changes in ocular hemodinamics and efficacy of transscleral (TS) Nd-YAG laser cyclophotocoagulation (CPC) in patients with absolute glaucoma. Material and Methods. We followed-up 30 patients (32 eyes) with absolute glaucoma; patients' age averaged 62.5 (SD, 2.09); 19 males (63%) and 11 females (37%). Baseline best corrected visual acuity (BCVA) averaged 0.011 (SD 0.018): BCVA=0.001-0.06 in 15 eyes (47%); BCVA=light perception (correct) in 5 eyes; BCVA=no light perception (incorrect) in 2 eyes; BCVA=0 in 12 eyes. A baseline IOP level averaged 38.2 (SD 5.05) mmHg ranging from 29.0 to 47.0 mmHg. A treatment course included three TS CPC sessions performed by Nd:YAG laser (λ=1.06 μm, I=0.8 J) every other day. TS CPC was performed concentrically in full circle (360°) in two rows, at 1.5-2.0 mm from the surgical limbus. A schedule of antihypertensive instillations was not changed. Additionally, a course of anti-inflammatory therapy was prescribed (indometacin, 0.1%, 4 times a day for a month). Results and Discussion. TS CPC of the ciliary body resulted in pain management in all patients (100%). The IOP level was significantly decreased compared to baseline: by 32%, immediately after TS CPC of the ciliary body and by 23% at 3 months after TS CPC, to 26 (SD 2.85) mmHg and 29.4 (SD 5.44) mmHg, respectively. Visual function remained the same after a treatment course. RQ blood circulation decreased after a treatment course at average by 34%, or to 2.3 (1.46) ‰ (р=0.00002). Vascular tone improved after TS CPC in 11%, 25.0 (SD 1.29)‰. The correlation analysis revealed a direct relationship between: the number of applications performed and a decrease of IOP (r=0.45), (р<0.05) as well as postoperative blood circulation (r=0.36), (р<0.05). There was also noted a significant correlation relationship (r=0.42), (р<0.05) between a decrease of an IOP level and a decrease of volume blood circulation of the eye after TS CPC of the ciliary body. Age and gender had no significant correlation relationship with IOP changes. TS CPC of the ciliary body did not achieve a desired effect in 8 patients (25%), which required a repeat course after three months. Conclusions. TS CPC of the ciliary body in patients with absolute glaucoma decreases IOP at average by 32% immediately after surgery and by 23% at 3 months after TS CPC. TS CPC of the ciliary body in patients with absolute glaucoma decreases volume blood circulation in the vascular pool of the ciliary body by 34% and reduces tonic properties of ciliary vessels by 11 %. TS CPC of the ciliary body is a successful organ-sparing treatment for patients with absolute glaucoma and has an apparent analgesic endpoint. Key-words: absolute glaucoma, transscleral laser cyclophotocoagulation of the ciliary body, blood circulation in the eye Background Absolute glaucoma is a disease which is caused by a range of different factors and which refers to a most severe ophthalmic pathology. Treatment of absolute glaucoma is of certain problems since conservative treatment is ineffective and surgery is dangerous with no chance to success. Instillations of various antihypertensive agents are insufficient to manage pain and to decrease intraocular pressure. Modern literature analysis has shown that surgical or combined (with intravitreal ranibizumab) methods are not always able to achieve a longstanding antihypertensive effect (treatment is successful within a 6 month period in 66.7-73.7% of patients) with occurrence of different complications in 5.6-31.6% of patients according to different authors. In addition, pain syndrome remains in most patients [6, 7, 15, 21, 27]. Today, there are several therapeutic methods of treatment for diseased eyes with zero vision, among which retrobulbar injection of chlorpromazine, 96° ethanol, and phenol are stood out [23, 24]. Cyclodestructive operations have taken the leading place in treatment of patients with painful absolute glaucoma. With experience and in result of experimental and clinical studies, the surgical techniques are being improved. Currently, the most prospective one is contact transscleral laser cyclophotocoagulation due to its simple technique, efficacy, compact equipment, and noninvasive impact [13]. Laser cyclodestructive interventions are widely practiced and performed even after multiple surgeries when intraocular pressure (IOP) stabilization and pain management have not been achieved [14]. Diode laser cyclophotocoagulation has been reported to be successful in 51-58.5% [25, 26]. Micropulse transscleral cyclophotocoagulation after endoscopic cyclophotocoagulation for refractive glaucoma has also been reported to have good results [20]. In pathogenesis of impact of contact transscleral laser cyclophotocoagulation of the ciliary body, the main role goes to partial atrophy of the ciliary body and its processes which results in lowering intraocular fluid production [3, 5]. Literature analysis has demonstrated a wide variety of success rates of laser cyclophotocoagulation in absolute glaucoma. One of mechanisms in glaucoma progression is vascular dysfunction [18]. Single papers have reported on disorders of regional circulation [1, 2, 4, 10, 16]. These papers demonstrate that, in open-angle glaucoma, a decrease in blood circulation of the uveal tract correlates with a level of IOP. A direct relationship was revealed between blood circulation in the ciliary body and a rate of aqueous humor secretion. Blood circulation disorders were noted in different vascular pools in the eye; however, a wide fluctuations range of regional blood circulation keeps from systemizing these data in regards to absolute glaucoma [8]. Rheoophthalmography (ROG) studies changes in blood circulation in the choroid. ROG gives an account of pulse volume changes and blood velocity. Rheogram calculates a rheographic quotient (RQ). In norm, RQ is 4.84‰, 4.22‰, and 3.74‰ for the ages of 10-20, 20-40, and 40-60, respectively. Studying ocular hemodynamics in glaucoma is an informative method providing a clear orientation to fine prescribing a particular additional medication. Studies on regional blood flow in the eye of patients with early and advanced stages of glaucoma have shown the improvement of blood content (RQ) by 25% after treatment using quercetin and polyvinylpyrrolidone [11]. Longstanding investigations and observations on blood circulations in the eye and brain, performed by N.G. Zavgorodnyaya and N.V. Pasyechnikova, have made it possible to determine regularities of these disorders, their relationship with clinical manifestations of glaucoma [9]. Based on the literature analysis, it became necessary to study changes in blood circulation and IOP in patients with absolute glaucoma before and after contact transscleral laser photocoagulation of the ciliary body with scleral compression. The purpose of the present paper was to study changes in ocular hemodinamics and efficacy of transscleral (TS) neodymium: yttrium-aluminum-garnet (Nd: YAG) laser cyclophotocoagulation (CPC) in patients with absolute glaucoma. Material and Methods We followed-up 30 patients (32 eyes) with absolute glaucoma; patients' age averaged 62.5 (SD, 2.09); there were 19 males (63%) and 11 females (37%). There were eight eyes with the end stage of primary glaucoma; four eyes with posttraumatic glaucoma; 12 eyes with secondary neovascular glaucoma caused by diabetes mellitus; eight eyes with outcome of central retinal vein occlusion. Baseline best corrected visual acuity (BCVA) averaged 0.011 (SD 0.018): BCVA=0.001-0.06 in 15 eyes (47%); BCVA=light perception (correct) in 5 eyes; BCVA=no light perception (incorrect) in 2 eyes; BCVA=0 in 12 eyes. A baseline IOP level averaged 38.2 (SD 5.05) mmHg ranging from 29.0 to 47.0 mmHg. To perform TS CPC of the ciliary body, we used a Neodymium: yttrium-aluminum-garnet (Nd: YAG) laser with λ=1.06 µm and with a 600 µm quartz fiberoptic polymer contact probe which had been developed in Laser Department of the Filatov Institute in collaboration with the Institute of Physics on NAS of Belarus. The laser was used for dosed compression of the sclera with a power of 2.4-4•105 dyn/cm2 with exposure time of 5-7 sec. Monofilament output energy was 0.8 J, which had been worked out in our experiment as optimal energy [12]. A treatment course included three TS CPC sessions every other day. TS CPC was performed concentrically in full circle (360°) in two rows, at 1.5-2.0 mm from the surgical limbus. In a part of patients, infrared diaphanoscopy was used to visualize ciliary processes, the width of which averaged 2.0 mm. Pre-operatively, the patients underwent epibulbar anesthesia with proxymetacaine hydrochloride (0,5%). A schedule of antihypertensive instillations was not changed. Additionally, a course of non-steroidal anti-inflammatory drugs including indometacin (4 times a day for a month) was prescribed since the latter decreases the activity of cyclooxygenase, an enzyme which participates in prostaglandin (inflammatory mediator) formation. All patients (60 eyes) underwent visual acuity test, IOP measurements, and rheoophthalmography at baseline and after treatment. Since major vessels were located similarly in the eyes with absolute glaucoma and in the fellow intact eyes (without clinically diagnosed glaucoma), it made it possible to use the latter as a control group to demonstrate in a full degree a specific character of changes in regional blood circulation in the eyes with painful absolute glaucoma. Rheoophthalmography was performed using a computer Rheography complex (Reocom, Ukraine, Karkiv). The complex is designed to measure electrical impedance of human body areas and time parameters of electrocardiography (ECG) and to process the data, to calculate parameters of regional hemodynamics, and to printout measurement and calculation result data. The study was performed in a patient placed in the prone position. Under epibulbar anesthesia with proxymetacaine hydrochloride (05%), a contact lens sensor was placed on patient’s eyeball and short-term recording (up to 60 s) with parallel ECG recording (Lead II) was made. In the present paper, we used parameters of blood volume pulse (BVP) defined by the rheographic quotient (RQ, ‰) and tonic properties of vessels defined by a ratio of the ascending rheowave duration to the whole rheowave duration (α/Т, %). Calculations were made using a software program (STATISTICA 10.0, StatSoftInc). Changes in IOP were assessed using the Friedman rank analysis of variance followed by the Wilcoxon signed-rank test to specify paired differences. To demonstrate the differences of changes, median (Ме) and standard deviation (SD) are given. Spearman's rho (r) was calculated for correlation analysis. Results and Discussion Immediately after TS CPC, dark round areas with a size corresponding to a wave-guide diameter were noted in the application sites. A number of the applications varied from 15 to 40 with an average of 28.8 (SD 6.53). Afterwards, in a part of the patients, we observed a development of combined injection which decreased after 4-times-a-day non-steroidal anti-inflammatory instillations of indometacin, eye tolerance of which was optimal. After the first TS CPC session, most patients noted a decrease of pain in the eye, and the pain syndrome was managed after three TS CPC sessions. The IOP level significantly decreased after a treatment course to 26.1 (SD 4.29) mmHg from the baseline level, i.e. by 32% (Table 1). As it can be seen in Table 1 a decrease of an average rank was noted immidiately after TS CPC. 3 months later, however, the average rank increased with the IOP level increased by 13% to 29.4 (SD 5.44) mmHg but remained significantly lower (by 23%) than that at baseline (χF2=57.3; p=0.0001).
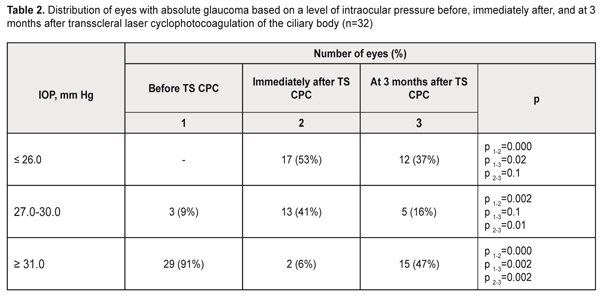
Distribution of the eyes based on an IOP level at different follow-up time points is given in Table 2.
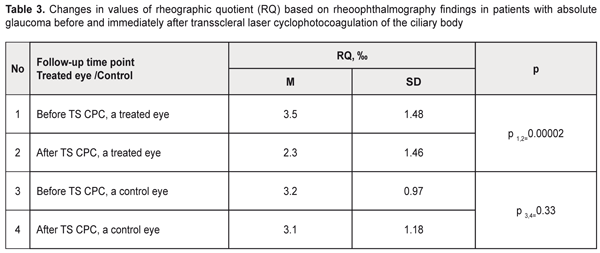
Table 2 shows that most patients (91%) had a baseline IOP level greater than 31.0 mmHg. The IOP level decreased and was within normal ranges (lower than 26 mmHg) in 53 % of the eyes immediately after TS CPC and in 37% of the eyes at 3 months after TS CPC. Our findings agree with those of E.Y. Wong et al. (1997), А. Mistlberger (2001), Р. Frezzotti et al. (2010) who have reported a decrease of the IOP level by 30% after diode laser contact transscleral cyclophotocoagulation in 56-73.2% of patients with refractive glaucoma with a mean follow-up period of 9 months [17, 22, 28]. It can be assumed that lowering IOP is conditioned by decreased production of aqueous humor against the background of decreased trophism of the ciliary body and ciliary processes associated with cell atrophy after laser radiation [8]. Visual function changed insignificantly after a treatment course. Improvement of visual acuity was noted in 4 eyes (13%), in which decreased IOP resulted in improvement of corneal transparency. ROG data of 30 patients (30 eyes) before and after TS CPC are displayed in Tables 3, 4, and 5.
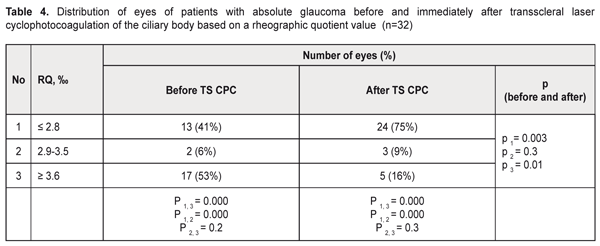
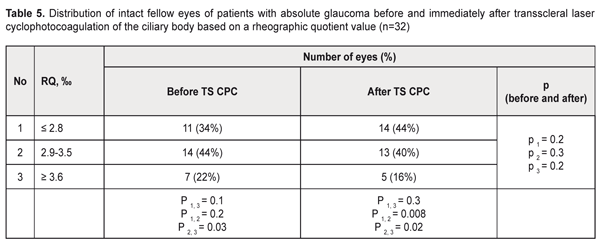
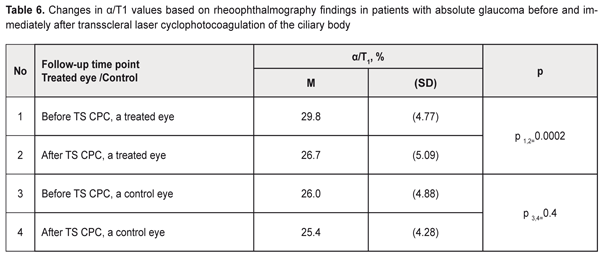
After treatment, volume blood circulation decreased significantly (by 34%) in the ciliary body vessels compared to baseline RQ (р=0.00002), 3.5 (1.48)‰ vs. 2.3 (1.46)‰, respectively. Distribution of the eyes with absolute glaucoma before and after TS CPC of the ciliary body based on RQ values are given in Table 4. As it can be seen in Table 4, at baseline, blood circulation was decreased in 41% of the eyes while 53 % of the eyes had increased blood circulation with congestive phenomena. After TS CPC, blood circulation was increased in 16 % of the patients and decreased in the 75% of the patients (р<0.05). Our findings are consistent with those of authors reporting that the effect of laser cyclolaserphotocoagulation is positive in non-ischemic glaucoma which has a high level of hemodynamic processes and, consequently, a high rate of intraocular fluid production [9]. Distribution of the intact fellow eyes is given in Table 5. After TS CPC of the ciliary body, volume blood circulation tended to be decreased in the intact fellow eyes as well. We believe that decreased RQ blood circulation in a TS CPC operated on eye is associated with reduced congestive processes and decreased inflammatory response which occurs in absolute glaucoma. Changes in intraocular vascular tone ROG values (α/Т1) in the patients with absolute glaucoma before and after TS CPC of the ciliary body are given in Table 6.
Table 6 demonstrates that TS CPC of the ciliary body resulted in a decrease in tone of large vessels by 10% (p=0.01) compared to baseline, 26.7 (SD, 5.09)% vs. 29.8 (SD, 4.77)%, respectively. Clear positive dynamics of IOP and pain syndrome management was noted after TS CPC of the ciliary body. The correlation analysis revealed a direct relationship between: the number of applications performed and a decrease in IOP (r=0.45), (р<0.05) as well as postoperative blood circulation (r=0.36), (р<0.05). There was also noted a significant correlation relationship (r=0.42), (р<0.05) between a decrease of an IOP level and a decrease of volume blood circulation of the eye after TS CPC of the ciliary body. Age and gender had no significant correlation relationship with IOP changes. During TS CPC of the ciliary body, hyphema occurred in two eyes (6%), which is consistent with data of other authors [19]. At 3 months of follow-up, 8 eyes (25%) referred with unpleasant sensations and discomfort in the eye; however, pain syndrome was not so pronounced as it was at presentation. Such patients required a repeat course of TS CPC of the ciliary body. Conclusions TS CPC of the ciliary body in patients with absolute glaucoma decreases IOP at average by 32% immediately after surgery and by 23% at 3 months after TS CPC. TS CPC of the ciliary body in patients with absolute glaucoma decreases volume blood circulation in the vascular pool of the ciliary body by 34% and reduces tonic properties of ciliary vessels by 11 %. TS CPC of the ciliary body is a successful organ-sparing treatment for patients with absolute glaucoma and has an apparent analgesic endpoint. References
|