J.ophthalmol.(Ukraine).2018;2:23-28.
|
https://doi.org/10.31288/oftalmolzh/2018/2/2328 Infrared thermography of external ocular surface in patients with absolute glaucoma in transscleral cyclophotocoagulation: a pilot study O. S. Zadorozhnyy, Cand Sc (Med), O. V. Guzun, Cand Sc (Med), A. Iu. Bratishko, T. B. Kustryn, I. O. Nasinnyk, A. R. Korol, Dr Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine; Odessa (Ukraine) E-mail: laserfilatova@gmail.com TO CITE THIS ARTICLE: Zadorozhnyy OS, Guzun OV, Bratishko AIu, Kustryn TB, Nasinnyk IO, Korol AR. Infrared thermography of external ocular surface in patients with absolute glaucoma in transscleral cyclophotocoagulation: a pilot study. J.ophthalmol.(Ukraine).2018;2:23-8. https://doi.org/10.31288/oftalmolzh/2018/2/2328
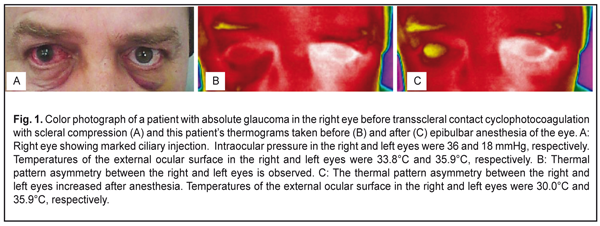
Background: Changes in the temperature of external ocular surface in patients with absolute neovascular glaucoma (including the changes after transscleral contact cyclophotocoagulation with scleral compression (TCCSC)) are still to be investigated. Purpose: To use infrared thermography (1) to investigate thermal patterns and to estimate the temperature of the external ocular surface in healthy individuals and (2) to compare these characteristics in the glaucomatous eyes versus intact fellow eyes of patients with absolute glaucoma undergoing treatment with 1064-nm TCCSC. Materials and Methods: Twenty healthy volunteers (40 eyes) and 45 patients (90 eyes) with absolute glaucoma were under observation. All 130 eyes underwent visual acuity assessment, anterior eye photography, and infrared thermography of the external corneal surface. Each patient underwent three sessions of 1 064-nm TCCSC. Results: In healthy subjects, mean external ocular surface temperature was 34.5 ± 0.7°C. For patients with absolute glaucoma, external corneal surface temperature at baseline was higher in intact fellow eyes than in glaucomatous eyes (34.3 ± 0.9°C versus 33.1 ± 0.8°С, P = 0.0008). In addition, increases in the temperature of external ocular surface were observed in the course of decrease in IOP after 1 064-nm TCCSC. Conclusion: In patients with absolute glaucoma, infrared thermography found a marked thermal pattern asymmety between glaucomatous eyes and intact fellow eyes. In addition, increases in the temperature of external ocular surface in the course of decrease in IOP after 1064-nm TCCSC may be apparently attributed to improved ocular blood flow and inflammatory response of the ciliary body to laser photocoagulation. Keywords: infrared thermography, temperature of external ocular surface, absolute glaucoma Introduction Infrared thermography is a well known diagnostic method with application in medicine for use in cardiac surgery, dermatology, oncology, ophthalmology, etc. which enables non-invasive real-time imaging of temperature distribution in superficial body tissues. It has undergone technological changes in recent years, an infrared thermography systems have become more available and easy to use, with their characteristics enabling fast and accurate assessment of surface temperature distribution of the object under investigation (e.g., external ocular surface) [1]. Temperature of the external corneal surface is influenced by environmental factors. Experimental studies demonstrated that reduced air temperatures and increased air velocity reduced external corneal surface temperature [2, 3]. In addition, an experimental study in monkeys demonstrated that decreasing choroidal blood flow by elevating intraocular pressure produced a decrease in ocular tissue temperature [4]. Moreover, in experimental animals, no significant difference in temperature was found between right and left eyes under various environmental conditions [2]. Neovascular glaucoma is a severe form of secondary glaucoma resulting from a myriad of ocular and systemic conditions with retinal ischemia as a mediator. In addition, it is characterized by a release of angiogenic factors, and new vessels formed on the iris and in the anterior chamber drainage angle, thus leading to sustained increased IOP [5]. Absolute glaucoma can develop if the disease is diagnosed and treated too late, and is characterized by sharp asymmetry in aqueous humor dynamics and ocular blood flow between the affected and intact eyes. Therefore, it is reasonable to believe that, in these conditions, infrared thermography will provide valuable data on the severity and course of disease as well as efficacy of provided treatment. However, changes in the temperature of external ocular surface in the course of decrease of IOP and restoration of ocular blood flow in patients with absolute neovascular glaucoma (including those that have undergone transscleral cyclophotocoagulation) are still to be investigated. The purpose of this study was to use thermography to (1) investigate thermal patterns and to estimate the temperature of the external ocular surface in healthy individuals and (2) to compare these characteristics in the glaucomatous eyes versus intact fellow eyes of patients with absolute glaucoma in the course of treatment with 1 064-nm transscleral contact cyclophotocoagulation with scleral compression (TCCSC). Materials and Methods This open-label comparative prospective pilot study followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee of the Filatov Institute. Written informed consent was obtained from all individual participants included in the study. Twenty healthy volunteers (40 eyes; age, 37 years to 65 years) and 45 patients (90 eyes; age, 41 years to 61 years) with absolute glaucoma were under observation. Each patient had an intact fellow eye. The cause of absolute neovascular glaucoma was thrombotic central or branch retinal vein occlusion (20 patients, 20 eyes) or diabetic retinopathy (25 patients, 25 eyes). All affected eyes received brimonidine and timolol 0.5%, a beta-blocker, both twice daily, before the study and over the course of laser therapy, whereas their fellow eyes received no eye drops for at least 2 weeks before initiation of study treatment. All 130 eyes underwent visual acuity assessment, anterior eye photography, and infrared thermography of the external corneal surface. A smartphone attached infrared thermography system, FLIR ONE, (FLIR® Systems, Inc., USA; spectral range, 8-14 μm; temperature range, 20°С to +120°С; accuracy, ± 0.1°С; resolution, 160×120 pixels) was used to measure external corneal surface temperatures in a room kept at constant temperature and relative humidity (20.1±0.6°C and 44.5±1.5%, respectively). A built-in digital video camera enabled taking visible range photos of the structures under investigation along with obtaining infrared images. Examination of participants and treatment of glaucoma patients were performed under stable environmental conditions (air temperature and humidity control and minimal indoor air velocity). Before thermography, participants spent 20 minutes indoors with their eyes closed for adaptation to the indoor environment. Healthy subjects underwent infrared thermography only once throughout the study. In patients with glaucoma, thermography was performed during each laser treatment session (before epibulbar anesthesia, after epibulbar anesthesia (immediately before laser), immediately after laser, and 30 minutes after laser) and at 1-month follow up. External ocular surface temperatures were recorded for both eyes in all participants. Laser interventions were conducted under epibulbar anesthesia. To this end, a drop of proxymethocaine (0.5%) was instilled thrice with an interval of 10 minutes. In each affected eye, three sessions of TCCSC were performed every other day (i.e., at days 1, 3 and 5 of the treatment course) using a 1 064-nm infrared laser to reduce IOP [6]. To position a laser probe accurately within the course of TCCSC, pars plicata was visualized in all quadrants using infrared diaphanoscopy [7]. Statistical analysis Means and standard deviations (SD) were calculated. Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. The level of significance p ≤ 0.05 was assumed. Results In healthy subjects, mean IOP and mean external ocular surface temperature were 19.0 ± 2.0 mmHg and 34.5 ± 0.7°C, respectively, and there were no significant differences in these characteristics between right and left eyes (P = 0.3 and P = 0.6, respectively). In patients with glaucoma, at the first session of TCCSC, before anesthesia (i.e., at baseline), visual acuity was perception of light with inaccurate projection of rays in the affected eye, and mean IOP in affected eyes and intact fellow eyes was 37.7±3.2 mmHg and 18.9±1.8 Hg, respectively. Thermography showed marked asymmetry between the thermal patterns of affected and intact eyes (Fig. 1B). For all patients, external corneal surface temperature at baseline was higher in intact fellow eyes than in glaucomatous eyes (34.3 ± 0.9°C versus 33.1 ± 0.8°С, P = 0.0008). In patients with glaucoma associated with diabetes mellitus, mean external corneal surface temperature in the affected eye was 33.3 ± 0.7°С. In patients with glaucoma associated with thrombotic occlusion of the central retinal vein, mean external corneal surface temperature in the affected eye was 32.8 ± 0.8°С and was not significantly different from glaucoma associated with diabetes mellitus (P = 0.6).
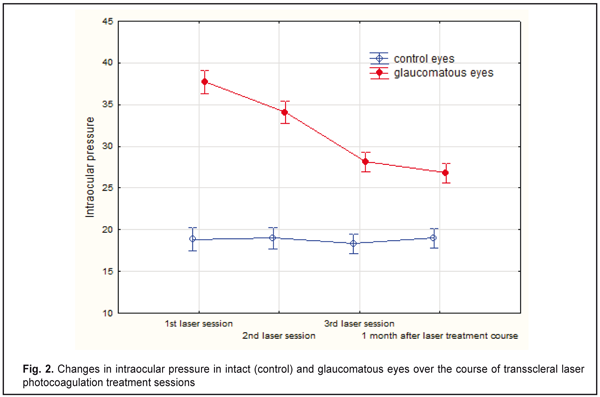
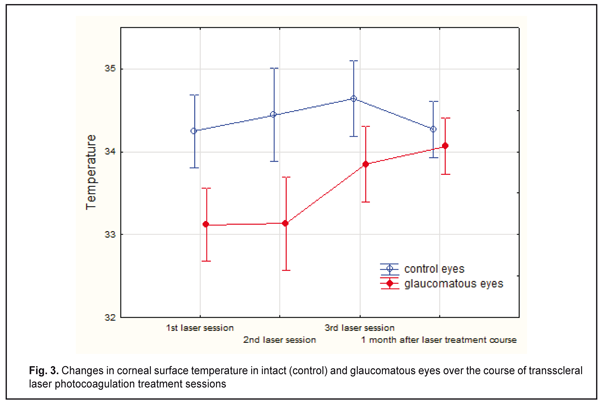
In all patients, at the first session of TCCSC, the asymmetry between the thermal patterns of affected and intact eyes increased with anesthesia (Fig. 1C). For all patients, mean external corneal surface temperature in the affected eyes decreased to 31.9 ± 0.9°С (and this decrease was statistically significant, P = 0.0001), and that in the intact fellow eyes was 34.1 ± 0.9°С and did not change significantly compared to baseline (P = 0.7) immediately after anesthesia. In addition, by 10 minutes after anesthesia, mean external corneal surface temperature in the affected eyes restored to baseline, and that in the intact fellow eyes was 34.2 ± 0.9°С and did not change significantly compared to baseline (P = 0.8). Furthermore, by 30 minutes after TCCSC procedure, mean external corneal surface temperature in the affected eyes increased to 33.5 ± 0.7°С and was somewhat increased over baseline (P = 0.15). By the second session of TCCSC, IOP in the affected eyes decreased to 34.1 ± 2.9 mmHg, while that in the intact eyes was 19 ± 2.0 mmHg (and did not change significantly compared to baseline, P = 0.8). In addition, mean IOP in the glaucomatous eyes was still significantly different from that in the intact fellow eyes (P = 0.000), and mean external corneal surface temperature in the former was still significantly lower than that in the latter (P = 0.000). Furthermore, mean external corneal surface temperature in the glaucomatous eyes and intact fellow eyes was 33.1 ± 1.1°С and 34.4 ± 1.0°С, respectively, and did not change significantly compared to baseline (P = 0.96 and P = 0.44, respectively). By the third session of TCCSC, IOP in the affected eyes decreased to 28 ± 2.3 mmHg (compared to that immediately before the second session, P = 0.000), while that in the intact eyes was 18 ± 2.1 mmHg (and did not change significantly compared to that immediately before the second session, P = 0.9). In addition, mean IOP in the glaucomatous eyes was still significantly different from that in the intact fellow eyes (P = 0.000). Furthermore, mean external corneal surface temperature in the former increased to 33.9 ± 0.8°С (P = 0.008), while that in the latter still did not change significantly and was 34.6 ± 0.9°С (P = 0.46). Moreover, at that time point, no significant difference in mean external corneal surface temperature was observed between the glaucomatous eyes and intact fellow eyes (P = 0.1). At month 1, mean IOP in the glaucomatous eyes was 26.8 ± 2.7 mmHg and somewhat decreased compared to that immediately before the third session (P = 0.2), and in the intact fellow eyes, was 19 ± 1.7 mmHg and did not change significantly (P = 0.16, Fig. 2). In addition, mean IOP in the former eyes was still significantly different from that in the latter eyes (P = 0.000). Furthermore, mean external corneal surface temperature in the glaucomatous eyes increased to 34.1 ± 0.8°С (P = 0.5), while that in the latter was 34.3 ± 0.4°С (P = 0.25). Moreover, at that time point, there was still no significant difference in mean external corneal surface temperature between the glaucomatous eyes and intact fellow eyes (P = 0.4).
No complications were observed during or after TCCSC treatment course. Discussion In this study, infrared thermography showed a pronounced asymmetry between the thermal patterns of glaucomatous and intact eyes, which can be attributed mainly to abnormal ocular blood flow in eyes with elevated IOP. We found that, in eyes with absolute glaucoma and elevated IOP, external corneal surface temperature was lower than in fellow eyes with normal IOP. A number of authors also demonstrated the effect of elevated IOP on ocular blood flow and external corneal surface temperature. Thus, Auker and co-authors [4] found decreased ocular perfusion pressure and external ocular surface temperature in monkey eyes with increased IOP. Galassi and colleagues [8] suggested that ocular surface temperature could be a marker of impaired retrobulbar hemodynamics in patients with primary open-angle glaucoma. Several studies demonstrated a relationship between external corneal surface temperature and ocular blood flow. Thus, in the study of Sodi and co-authors [9], ischemic CRVO eyes showed lower ocular surface temperatures than nonischemic ones. Morgan and colleagues [10] investigated ocular surface temperatures in patients with carotid artery stenosis and found that the affected side showed lower ocular surface temperatures than unaffected. In addition, the results of their study indicated that anastomoses within the brain were unable to compensate fully for the reduction in blood flow on the affected side. In our current work, in patients with absolute glaucoma, increases in the temperature of external ocular surface were observed in the course of decrease in IOP after 1064-nm TCCSC. Thus, mean IOP in the glaucomatous eyes was significantly reduced as early as day 3 of the laser treatment course. In addition, in these eyes, temperature of the external ocular surface increased and was not significantly different from intact fellow eyes only by the third laser session (i.e., day 5). Furthermore, at month 1 after laser treatment, in the glaucomatous eyes, mean external corneal surface temperature was still not significantly different from intact fellow eyes. In the study of Galassi and colleagues [11], an increase in corneal surface temperature was observed in the eyes that underwent glaucoma surgery. In the study of Fujishima and co-workers [12], corneal temperature was found to be increased compared to baseline even on days 1 and 30 after cataract surgery due to postoperative inflammation. Therefore, apparently, in eyes with absolute glaucoma, an increase in external corneal surface temperature after TCCSC should be attributed to improved ocular blood flow in the presence of not only reduced IOP, but also inflammatory response of the ciliary body to transscleral photocoagulation. The use of some types of IOP-reducing eye drops may result in a reduction of external corneal surface temperature. Thus, Brimonidine, an α2-adrenergic agonist, decreases production of the aqueous humor by vasoconstriction of ciliary body blood vessels [13]. Conclusion First, infrared thermography is an easy-to-use and safe method for documenting the thermal pattern asymmetry between right and left eyes, and enables high accuracy measurements of external ocular surface temperature. Second, in healthy subjects, infrared thermography found no thermal pattern asymmetry between right and left eyes, with a mean external corneal surface temperature of 34.5°С. Third, in patients with absolute glaucoma, infrared thermography demonstrated a marked thermal pattern asymmety between glaucomatous eyes and intact fellow eyes, and the mean external corneal surface temperature was lower in the former than in the latter (33.1°С vs 34.3°С). Finally, in eyes with absolute glaucoma, an increase in external corneal surface temperature after TCCSC may be apparently attributed to improved ocular blood flow in the presence of inflammatory response of the ciliary body to laser photocoagulation.
Acknowledgements: The authors would like to thank professor A.S. Buiko for his methodological assistance in conducting the study. References
|