J.ophthalmol.(Ukraine).2018;1:78-80.
|
https://doi.org/10.31288/oftalmolzh201817880 Characteristics of measles keratoconjunctivitis in adults O.N. Ivanova, Cand. Sc. (Med.), T.B. Gaydamaka, Dr. Sc. (Med.), G.I. Drozhzhyna, Dr. Sc. (Med.), T.A. Veliksar, Postgraduate Student Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine; Odessa (Ukraine) E-mail: tveliksar@gmail.com TO CITE THIS ARTICLE: Ivanova ON, Gaydamaka TB, Drozhzhyna GI, Veliksar TA. Characteristics of measles keratoconjunctivitis in adults. J.ophthalmol.(Ukraine).2018;1:78-80. https://doi.org/10.31288/oftalmolzh201817880 Introduction. Measles (lat. morbilli) is an acute anthroponotic infectious virus disease with a high contagion level. In general, measles is common for children. However, there are a good number of the diseased among adults. A clinical picture of measles in adults is characterized by more intensive symptoms and by more likely development of complications. Purpose. To analyze the clinical course of measles keratoconjunctivitis in adults. Materials and Methods. In 2017, we followed up two patients (aged 34 and 42) having had measles with an atypical disease course. Both patients were diagnosed bilateral conjunctivitis and superficial punctate keratitis. Dry eye syndrome was moderate. The patients were performed anti-inflammatory, antiviral, desensitizing and substitutional therapy. 3 days after treatment onset, the patients' complaints decreased and biomicroscopy findings were improved. At Day 7, the subjective complaints and clinical signs almost disappeared. Conclusion. The course of measles in adults is of particular severity. Measles keratoconjunctivitis is characterized by punctuate eruption in the cornea and pronounced dry eye syndrome. Early therapy enabled to regress the process and to recover the vision within a short period of time. Key-words: keratitis, measles, keratoconjunctivitis, epitheliopathy Introduction Measles (lat. morbilli) is an acute anthroponotic infectious virus disease with a high contagion level (a contagiosity index is near 100%). It is caused by an RNA virus of the genus Morbillivirus within the family Paramyxoviridae. The virus is spread by airborne transmission and is characterized by a cycling course of the disease, development of intoxication and signs of catarrhal inflammation of mucous membranes, occurence of enanthema, Belsky - Filatov - Koplik spots, and specific gradual changes of spotted papulose exanthema [1, 4, 6, 11]. In 2017 there was an epidemic growth of measles incidence in Europe. Data published by European Center for Disease Prevention and Control (ECDC) demonstrate that within the period between January 2016 and October 2017 in Europe (EU) there were registered almost 19 000 cases of measles including 44 cases followed by death. The most 2017 cases were registered in 14 European countries including Romania (7 570), Italy (4 617), Ukraine (1 627), and Germany (894) [2]. The Ministry of Health of Ukraine has reported that 1 627 cases of measles were registered in Ukraine in 2017 at the beginning of September (two fatal cases in Odessa region). Most of the cases were noted in Ivano-Frankovsk (747) and Odessa (589) regions. In general, measles is common for children. However, there are a good number of the diseased among adults. Thus, this year in Odessa region there have been registered 200 cases of disease among the adult population (33.9% of total). The spread of measles throughout Europe is associated with a low level of measles vaccine coverage. Last year, fewer than half of Ukrainian children were measles vaccinated according to the schedule [3, 5, 10]. A clinical picture of measles in adults is characterized by more intensive symptoms with pronounced intoxication of the body and by more likely development of complications (hearing and vision disorders develop in 30% of patients over 20 y/o). Conjunctivitis can develop in pre-onset period of the disease. According to foreign authors, keratitis occurs in 3.3% to 10.6% of cases [7, 8, 9, 12]. Over the years, measles patients have not applied to the hospital of the Filatov Institute. In 2017, two patients were treated for measles keratoconjunctivitis during the measles epidemic. Purpose. To analyze the clinical course of measles keratoconjunctivitis in adults. Materials and Methods In 2017, we followed up two patients (aged 34 and 42) having had measles with an atypical disease course. While being treated at infectious diseases hospital for measles, both patients were diagnosed keratoconjunctivitis. Measles developed with extensive cutaneous eruption (Figure 1).
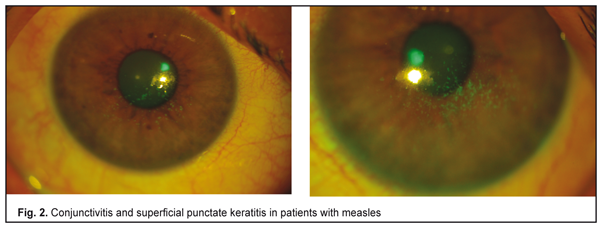
Results Upon discharge from infectious diseases hospital, on the same day, both patients were admitted to Corneal Pathology Department of the Filatov Institute of Eye Diseases and Tissue Therapy with complaints of photophobia and foreign body sensation in both eyes. As told by the patients, the complaints were gradually increasing since enanthesis appeared on the face. Beginning from the second day at infectious diseases hospital, both patients were prescribed okoferon instillations four times a day. At admission to Corneal Pathology Department, both patients were diagnosed bilateral conjunctivitis and superficial punctate keratitis (Figures 2, a, b). Dry eye syndrome was moderate.
Biomicroscopy revealed the changes as follow: conjunctival hyperemia, single hemorrhages; the corneal surface was rough and fluorescein penetrated in the form of epitheliopathy; in the optic zone, the cornea at subepithelial levels was fluorescein stained as numerous punctuate (0.1mm) infiltrates; a smooth swelling was noted in the stroma. The patients were performed anti-inflammatory, antiviral, desensitizing and substitutional therapy which included: 0.02% chlorhexidine instillation, okoferon (іnterferon alfa-2b), 2% ectoin, thiotriazolinum, hylo care four times a day; ganciclovir gel five times a day; at later terms, dexamethasone; parabulbar injections: heparin, thiotriazolinum, and dexamethasone; intramuscular injections: 1 mln laferobion (іnterferon alfa-2b), non-steroidal anti-inflammatory agents, desensitizing agents, vitamins. At 3 days after treatment onset, the patients noticed state improvement and significantly reduced photophobia. Biomicroscopy revealed a reduction of conjunctival hyperemia, corneal epitheliopathy with the poorly fluorescein penetrated corneal surface, as well as a resolution of subepithelial punctuate infiltrates. The stromal swelling was resorbed. At Day 7, the subjective complaint disappeared (photophobia, foreign body sensation). Biomicroscopy showed mild conjunctival hyperemia; subconjunctival hemorrhages were resolved; the corneal surface was smooth and epithelized. Subepithelial punctuate infiltrates were resorbed. The stroma was transparent. Visual acuity increased to 1.0. The recommendations as follow were given: antiseptic agent instillations four times a day (boric acid solution, chlorhexidine solution, miramistin solution); іnterferon alfa-2b (okoferon) 4-6 times a day; tear substitutes 4-6 times a day (hylo-care, hylo-comod, 0.21 % optinol, Thealoz Duo); nutritional vitamin drops four times a day (sensivit, lacrisek, thiotriazolinum); overnight repairing agents (corneregel, solcoseryl). Conclusion The course of measles in adults is of particular severity. Measles keratoconjunctivitis is characterized by punctuate eruption in the cornea and pronounced dry eye syndrome. Early therapy enabled to regress the process and to recover the vision within a short period of time. References
|