J.ophthalmol.(Ukraine).2018;1:74-77.
|
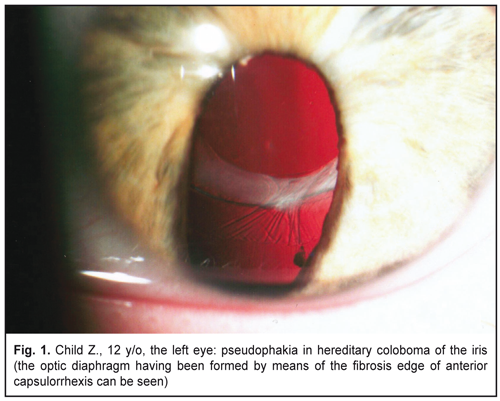
https://doi.org/10.31288/oftalmolzh201817477 Surgical management of bilateral congenital coloboma of the iris and congenital cataract N.F. Bobrova , Dr Sc (Med), Prof.; D.V. Smaglii, internship doctor SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”; Odessa (Ukraine) E-mail: filatovbobrova@gmail.com TO CITE THIS ARTICLE: Bobrova NF, Smaglii DV. Surgical management of bilateral congenital coloboma of the iris and congenital cataract. J.ophthalmol.(Ukraine).2018;1:74-7. https://doi.org/10.31288/oftalmolzh201817477 Background. A combined character of a defect, which is congenital coloboma in the presence of congenital cataract, brings up an issue of choosing optimal management to achieve the maximum possible optical functions, provided that the risk of development of operational and postoperative complications is reduced. Purpose. To analyze a character, features, and complications and to develop the optimal surgical management of bilateral congenital iris coloboma and cataract. Material and Methods. Visual acuity testing, standard ophthalmic examination, distance ultrasound biometry, keratometry, ultrasound scanning were performed. Results and Conclusions. We performed minimally invasive surgery including phacoemulsification of congenital cataract with IOL endocapsule implantation and formation of optic diaphragm without interventions in the iris. Visual acuity in the pseudophakic left eye increased to 1.0 within 3 months, additional diaphragming was not able to correct visual acuity. High visual acuity, 1.0, remained in the right eye in the presence of coloboma of the iris and partial cataract. Binocular vision was achieved. The autoplasty method using the proper lens capsule for coloboma of the iris made it possible to maximally improve visual acuity in the eyes with double congenital abnormality of the iris and the lens. The reasonable attitude to corepraxy, considering the bilateral damage, enabled to achieve binocular vision within the shortest possible period of time after surgery. Key-words: congenital coloboma of the iris, congenital cataract, childhood, cataract phacoemulsificаtion, IOL implantation, autoplasty Introduction Coloboma is a disease caused by a range of different factors and characterized by an isolated or combined hole of the iris, retina, vitreous, optic nerve, or eyelid. Missing pieces in the eyeball structures are caused by the failure of the choroid fissure to close up at weeks 4-5 of prenatal development [7]. One of the causes of the defect can be cytomegalovirus infection in the mother at early stages of gestation [4]. A term of coloboma was introduced by Walther, meaning “a lacking part” from the Greek. The frequency of coloboma is approximately 4.89 per 100 000 newborns [6]. Based on statistic data, the most common among all described types is coloboma of the iris (1:6 000). The pathology occurs among males and females with the same frequency. A typical coloboma of the iris is observed in the lower quadrant. This can be explained by the fact that the choroid fissure closes in the lower part of the eye glass [4]. A typical coloboma is shaped like a pear or an inverted drop. A congenital coloboma can be isolated in one eye but more often, in 60% of cases, it occurs in both eyes [1]. A combined character of a defect, which is congenital coloboma in he presence of congenital cataract, brings up an issue of choosing surgical managements to achieve the maximum possible optical functions provided that the risk of development of operational and postoperative complications is reduced. The purpose. To analyze a character, features, and complications and to develop the optimal surgical management of bilateral congenital coloboma of the iris and congenital cataract Material and Methods A 12-year-old child’s parents applied to Pediatric Ophthalmology Department of the Filatov Institute with complaints about a decrease in visual acuity of the left eye within the last few years. Best corrected visual acuity of the right eye was 1.0; best uncorrected visual acuity of the left eye was 0.05; monocular vision; color perception was not disturbed. Physical examination showed quiet eyes, transparent cornea, the anterior chamber of average depth, and typical full congenital colobomata of the iris in both eyes. The pupils were slightly decentrated downwards. The right eye had lens opacities in layers in the periphery; in the left eye, the lens was unevenly cloudy. The posterior segment of the right eye had no changes; the left eye fundus could not be ophthalmoscopically examined. Distance ultrasound biometry: OD – 23.11 mm; OS – 23.86 mm, which allows considering myopization of the vision worst eye. Keratometry: OD, 42.0 D; OS, 42.25 D. Ultrasound scanning (sine-scan) of the eyes: the anterior chamber of the mid depth, 3.2 mm; the iris had a missing part at the lower quadrant at 5-7 o’clock; in the rest of directions, the angle of the anterior chamber was about 40 degrees. The lenses were acoustically anechogenic with a thickness of 3.51 mm and 4.20 mm in the right and left eyes, respectively, which evidenced about a certain swelling of the lens substance. IOL was calculated according to the formula CRKII: OD= 23.1D, OS= 21.0D. Results and Discussion Considering the presence of the combined congenital defect of both eyes, colobomata of the iris and cataract, as well as the apparently decreased visual acuity in the left eye with high visual acuity in the right eye, we recommended surgical treatment for the left eye, s.s. phaco-aspiration of congenital cataract with endocapsular IOL implantation. Surgery performed was characterized by the presence of week subluxation of the lens upwards: the ciliary zonules within the coloboma area were stretched, thinned, and missing in the certain parts. Viscoelastic addition to this area made it possible to prevent vitreous prolapse. In consequence of the iris congenital defect, the pupil was insufficiently dilated upwards; however no additional measures were used to dilate it. In the center, we managed to form capsulorrhexis, 5.0 mm in diameter. Phaco-aspiration, irrigation of the lens nucleus and mass, was without abnormalities; however, removal of the lens mass from the upper area of the capsular bag, which was covered with the pupil edge of the iris, required using an angle handpiece and a phacoemulsification system. The IOL optic power was increased by 1.0D' as compared to the calculated one to achieve mild myopia and to improve near vision. An Acrysof SN60WF IOL, +22.0D, was implanted using a cartridge into the capsular bag without complications. At first, the IOL was placed in a position of 6-12 o’clock for a lower haptic element to pull down the edge of the capsular bag. However, it was not possible to achieve the dislocation of the capsular bag downwards so the IOL was rotated in a position of 3-9 o’clock. Therefore, the IOL center, dislocated a little upwards, and the optic center of the pupil were in line. Postoperative period was unremarkable. On discharge, the eye was quiet, the fundus eye was without pathological findings, and best uncorrected visual acuity increased to 0.7. 3 months after surgery, visual acuity in the operated left eye increased to 1.0; additional diaphragming and correction did not improve the vision. High visual acuity, 1.0, remained in the right eye. For near vision, the operated eye required additional correction +2.0D, font #5 could be read. Binocular vision was achieved. Since the frequency of congenital coloboma changes is extremely low, there are few researches on the character of cataract surgery in the presence of this defect. As a rule, they have been presented as single observations, excluding the paper of Stashevich S.V. with colleagues [5] on outcomes of surgeries performed in 27 eyes (16 patients). It should be noted that the age of patients with iris coloboma and cataract, based on the literature data, ranged from 38 to 72 years, which allows considering secondary lens opacity with age-related cataract development when congenital colobomata have existed so far. Only Nordlund [10] has reported that among seven operated patients, there was one 18-year-old patient with microphthalm, the rest aged 42-50. Thus, our case of surgery in the 12-year-old child is kind of unique. In the literatute, we have met different surgical techniques for cataract extraction in the presence of congenital coloboma of the iris. Thus, there is an interesting case of intracapsular extraction of cataract through a wide congenital coloboma using forceps in 59 year-old patient [9]. Jaffe and Clayman [8] have described in details a character of the congenital defect and surgery in six eyes (4 patients, aged 48-72 years). The authors noted that defective changes in congenital colobomata of the iris were observed both in the iris itself and in the ciliary zonules, ciliary body, inferior pole of the lens, and even in the sclera which was thinned in the inferior pole. For cataract extraction, the authors used an intracapsular technique in one case and phacoemulsification with posterior-capsular IOL implantation in the rest, including one case with endocapsular fixation. These authors are first to have achieved the surgical success in this pathology. Nordlund and colleagues [10] have operated within twelve years seven eyes (5 patients) with typical congenital coloboma and cataract with a follow-up period not less than two months. When performing surgery, the authors noticed frequent myosis (3 cases), for reversal of which they used both iris retractors and multiple sphincterotomy production; difficulties with capsulorrhexis were explained by the weakness of the ciliary zonule in the coloboma area, high density of the anterior capsules in one case where they needed to use scissors; in two cases there was vitreous prolapse through both the congenital coloboma area and spontaneous rupture of the posterior capsule. One eye was performed close iridoplasty of coloboma, one eye was left aphakic, four eyes were IOL implanted (endocapsularly and in the ciliary sulcus, in 3 and 1 cases, respectively). Among postoperative complications the authors pointed at retinal detachment development in the aphakic eye and monocular diplopia associated, in their opinion, with an ectopic pupil of the operated pseudophakic eye. Wide clinical observations of 27 eyes (16 patients) have allowed Stashkevich S.V. and colleagues [5] to execute digital systemization of anterior eye defects. Herewith, the authors determined that there was brunescent cataract in 80% of patients, dysplasia of ciliary zonules fibers in 76%, the ectopic pupil of varying degrees in 74.5%. Their results enabled to develop the classification of pupil ectopia in congenital colobomata of the iris, which practically resulted in indications for achieving both optimal mydriasis (using iris retractors, as a rule) and pupilloplasty variants to eliminate coloboma and the pupil’s centration (sphincterotomy and wedge resection of the pupillary border of the iris in the meridian opposite to coloboma). For cataract extraction, the authors recommended to use a capsule supporting ring and a phaco-chop/stop&chop combination. For IOL implantation, soft models were preferable with haptic to be located perpendicular to the coloboma projection. The authors also noted such operation complications as vitreous prolapse (7.4%), rupture of the posterior capsule (3.7%), and hemorrhages during iridoplasty (11.1%); postoperative compications were: transitory hypertension and hyphema (11.1% each); variously expressed swelling of the cornea (3.7%). As we pointed, our case is a unique one because of the simultaneous presence of two congenital defects, differently expressed congenital cataracts and bilateral congenital colobomata, equal in size and location, in a 12-year-old child. High visual acuity of the right eye (1.0) in the presence of partial cataract and coloboma of the iris required a well-reasoned approach to iridoplasty performance, also considering mild but present ectopia of the both pupils. Alongside this, a wish to perform diaphragming in the coloboma area would undoubtedly improve the vision of an operated eye with total cataract of the uncertain term and possible amblyopia development. Based on the existing situation, we used an autoplasty method we had developed before and used in surgery for traumatic cataracts: a usage of self-tissues of the eye in order to cover a defect of the iris. In this case, it was a flap from the anterior capsule of the lens which was a bit wider in the coloboma area because of little lens subluxation upwards. The further fibrosis of the anterior capsulorrhexis boder formed a certain diaphragm (Fig. 1), which made it possible to achieve the highest visual acuity (1.0). Herewith, additional artificial diaphragming did not increase visual acuity.
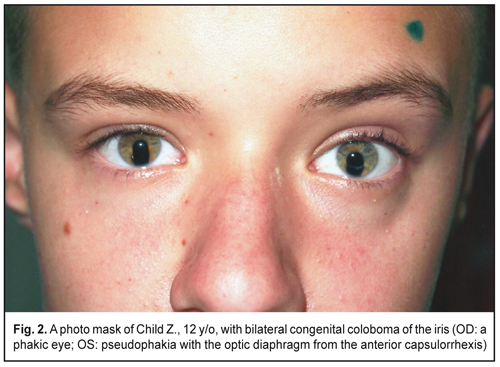
Our observation confirmed the presence of abnormal changes of ciliary zonules in the coloboma area and vitreous prolapse was prevented through the constant additional administration of vascoelastic for tamponing the defect [3]. It is important to pay careful attention to maintaining the symmetry of the ectopic pupils with a bilateral defect, which enables to achieve in the postoperative period the formation of binocular vision, avoiding the monocular diplopia development which has been described by previous authors. Also, we should point at the sparing character of this surgery (iris retractors, capsule rings, or iridoplasty were used) which made it possible to out complications and achieve the best result in the eyes with double abnormality. At the present time, the teenager is comfortable with existing bilateral colobomata of the iris (Fig. 2), his parents do not strain after cosmetic operations.
Conclusions Minimally invasive surgical methods in ophthalmology give the possibility to restore the sight with high visual acuity and, along with that, the quality of life, to minimize the number/volume of surgical interventions and complication development in the presence of bilateral congenital cataract and coloboma of the iris. The autoplasty method using the proper lens capsule for coloboma of the iris made it possible to maximally improve the vision in the eye with double congenital abnormality of the iris and the lens.
The reasonable attitude to corepraxy, considering the bilateral damage, enabled to achieve binocular vision within the shortest possible period of time after surgery. References
|