J.ophthalmol.(Ukraine).2018;1:60-66.
|
https://doi.org/10.31288/oftalmolzh201816066 Effect of different modes of high-frequency electric current on structural changes in the optic nerve in rabbits N.F. Bobrova 1, Dr. Sc. (Med.), Prof.; V.V. Vit 1, Dr. Sc. (Med.), Prof.; T.A. Sorochinskaya 1, Cand. Sc. (Med.); N.I. Molchanyuk 1, Cand. Sc. (Med.); I.M. Levitsky 2, ophthalmologist 1 Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine; Odessa (Ukraine) 2 AILAZ Medical Center; Kiev (Ukraine) E-mail: filatovbobrova@gmail.com TO CITE THIS ARTICLE: Bobrova NF, Vit VV, Sorochinskaya TA, Molchanyuk NI, Levitsky IM. Effect of different modes of high-frequency electric current on structural changes in the optic nerve in rabbits. J.ophthalmol.(Ukraine).2018;1:60-6. https://doi.org/10.31288/oftalmolzh201816066
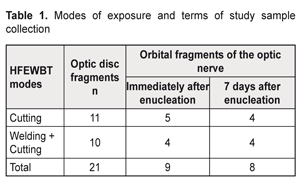
An original technique for enucleation of the eyeball with advanced retinoblastoma using high-frequency electric welding of biological tissues (HFEWBT) was developed in SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine” in 2013. Purpose. To study in experiment the effect of different modes of electric high-frequency current on structural changes of the rabbit’s optic nerve and the extension of the structural changes after eye enucleation. Material and Methods. 14 Chinchilla rabbits (21 eyes) were enucleated the eyeball using an EK-300M1 unit. We used two modes of the HF-current exposure for transection of the optic nerve: Group 1 (11 eyes), a cutting mode (current intensity, 1.5 A; voltage, 200 V; power, 350 W; frequency, 66 kHz; exposure, up to 3 sec); Group 2 (10 eyes), a welding (current intensity, up to 0.3 A; voltage, 40-60 V; frequency, 66 kHz; exposure, up to 3 sec) + cutting mode. Fragments of the optic nerve excised during the surgery were studied light-optically and ultrastructurally. Results. Using both cutting and welding+cutting modes of the HFEVBT method for the transection of the optic nerve caused the development of dry necrosis in the parenchyma and sheaths of the optic nerve not only in the site of exposure but also at the distance which depended on the mode used. Herewith, the welding+cutting mode caused necrosis, growing by the Day 7 up to 3-4 mm wide, which two times exceeded the necrosis extension when using the cutting mode. Degeneration and gliosis of the optic nerve in Group 2 (welding+cutting) occurred within the greater area than that in Group 1 (cutting), reaching the optic disc and sensory retina. Conclusions. We believe that the extension of the destructive changes when using the welding+cutting HFEWBT mode can increase the ablasticity of enucleation of the eyes with retinoblastoma at high risk of optic nerve invasion. Key-words: optic nerve, electric welding, high frequency current, experiment Background In 1991, Ukrainian academicians B.Ye. Paton and V.K. Lebedev developed a model of using high-frequency current (HF-current) to weld live soft tissues with preserving the viability of bordering tissues that was confirmed by a series of experiments in animals [1, 8, 9]. Today, this technology is successfully developing, the equipment is being improved, and new surgical techniques are emerging. In ophthalmology, high-frequency electric welding of biological tissues (HFEWBT) was first used in Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine for eyeball enucleation associated with uveal melanoma in order both to transect the external rectus muscles and the optic nerve and to connect the conjunctiva [5, 7]. We developed a new technique of enucleation using HFEWBT for advanced retinoblastoma [2, 3]. However, the possibility of using this technique for transecting the optic nerve in order to prevent the extension of neoplasm into the skull cavity in enucleation of the eyes with retinoblastoma at high risk of optic nerve invasion has not been studied. In this regard, we carried out an experimental study on changes in the optic nerve under different modes of electric HF-current after eyeball enuclation in rabbits. Purpose. To experimentally study the effect of different modes of electric HF-current on structural changes in the rabbit’s optic nerve and their extension after enucleation of the eyeball. Material and Methods Experimental studies were performed on the basis of vivarium at Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine, and followed regulations approved by the Act of Ukraine No1759-VI from 15 December 2009 On Protection of Animals from Cruelty. The studies involved 14 Chinchilla rabbits. The animals of the same age and weight, 5-6 months and 2.5-3 kg, respectively, were maintained in separate cages under standard conditions. All the animals were performed enucleation using two modes of the HF-current exposure for transecting the optic nerve: Group 1 (11 eyes), a cutting mode; Group 2 (10 eyes), a welding+cutting mode. In the experimental study we used an EK-300M1 unit and a set of electric welding tools designed in the E.O. Paton Electric Welding Institute [5, 6]. The unit provides such modes as welding, coagulation, overlap, and cutting. The main frequency of an original high-frequency signal is 66 kHz; the range of load is 10-1000 Ohm. The cutting mode is used for tissues with increased resistance (current intensity, 1.5 A; voltage, 200 V; power, 350 W; frequency, 66 kHz; exposure, up to 3 sec). The welding mode (current intensity, up to 0.3 A; voltage, 40-60 V; frequency, 66 kHz; exposure, up to 3 sec) is recommended for welding up vessels, connecting tissues and edges of a surgical incision. A level of optimal power is determined automatically depending on a tissue type. Using this mode, a real time of exposure is determined automatically within the selected range; the operate time of HF-current is maximal. The electrosurgical effect of cutting and coagulation is based on providing quite a high degree of heat of biological tissues by a narrow HF-current flow between the energy sources of bipolar welding instruments. The principle of the method is based on coagulative changes in the welded tissues under the influence of high frequency current. Operational Procedure: under general anesthesia (thiopental sodium), after preoperative showering with 0.5 chlorhexidine, the conjunctiva was separated from the limbus and the rectus muscles were cut; the eyeball was fixated to the medial rectus muscle tendon. In Group 1, the optic nerve was transected by specially developed forceps-scissors using HFEWBT in the cutting mode. In Group 2, the optic nerve was first exposed by forceps-scissors using HFEWBT in the welding mode and, afterwards, immediately transected using the cutting mode. The fragment of the optic nerve to be studied was excised using standard scissors immediately after operation and at 7 days after enucleation, in 9 eyes and 8 eyes, respectively. On operation completion, the orbit was injected antibiotic and plugged sterile goods. Follow-up examinations were performed on the following day, on Day 3 and 7 after operation. To prepare sections for light-optical morphometry, the optic disc (Group 1: 11 fragments; Group 2: 10 fragments; Total: 21 fragments); and the orbital fragment of the optic nerve (Group 1: 9 fragments; Group 2: 8 fragments; Total: 17 fragments) were excised. Data on the modes of exposure and the terms of sample collection are given in Table 1.
The collected samples were fixated in 10% formalin; the prepared sections were hematoxylin and eosin stained and light-optically studied. To perform the ultrastructural study, the optic disc fragments (4 fragments for each mode (cutting and welding+cutting)) and the orbital fragments of the optic nerve (4 fragments for each mode) were excised; the fragments were fixed in 2.5% glutaraldehyde in phosphate buffer (pH 7.4) and followed by 1% osmic acid postfixation in phosphate buffer (pH 7.4). Afterwards, the samples were dehydrated in graded alcohol solutions. Araldite/Epon mixture was used to infiltrate and embed the samples. We performed pathomorphological and ultrastructural studies of the following tissues obtained from the rabbits’ eyes immediately after enucleation using the different HFEWBT modes: the optic disc, sections of optic disc-surrounding sheaths of the eye, the optic nerve in the site of its transection, and 9 orbital fragments of the optic nerve; 8 orbital fragments of the optic nerve were obtained at Day 7 after enucleation. Results In all cases, surgical intervention proceeded without complications. HFEWBT for the optic nerve transection made it possible to perform practically bloodless enucleation since bleeding from the large ophthalmic artery was excluded. No complications (edema of orbital tissues, hemorrhages, pyoinflammatory processes) were observed during the postoperative period. The healing process was smooth. Effect of HFEWBT in the cutting mode on the optic nerve in rabbits (Group 1) Pathomorphological study of the optic nerve sections obtained immediately after enucleation using HFEWBT in the cutting mode revealed: pronounced edema of the optic nerve parenchyma just near the exposure site; homogenization of ganglion cell axons; focal necrosis of connective-tissue formations dividing axons into bundles; disappeared intermeningeal spaces and necrosis of meningothelial cells. The sheaths of the optic nerve were saturated with hemolyzed blood. A necrosis band of the optic nerve parenchyma corresponded to the size of the working surface of the instrument used for the optic nerve transection and spread out it approximately 1-2 mm on either side. Edema of the optic nerve parenchyma was noted outside the necrosis area. Attention was drawn to destruction in walls of the central artery and the retinal vein located centrally in the parenchyma of the optic nerve. Herewith, the blood was partially hemolyzed and around vessels we noted pronounced edema with voids filled with fluid (Fig. 1).
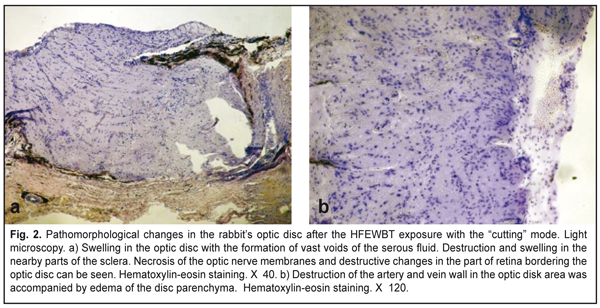
Similar changes were detected in the optic disc. First of all, there was a swelling with voids, different in form and size, filled with serous fluid. A swelling was also noted in a part of the sclera surrounding the optic nerve. Variously pronounced swellings and first signs of vacuole degeneration of glial elements and neurons were also noted in the retina, in sites immediately bordering the optic nerve (Fig. 2A). Destruction of the retinal arteries and veins located on the inner retinal surface in the area of the optic disc was also revealed (Fig. 2B). Herewith, the arteries and veins were filled with homogeneous mass of hemolyzed blood with a great amount of coagulated proteins.
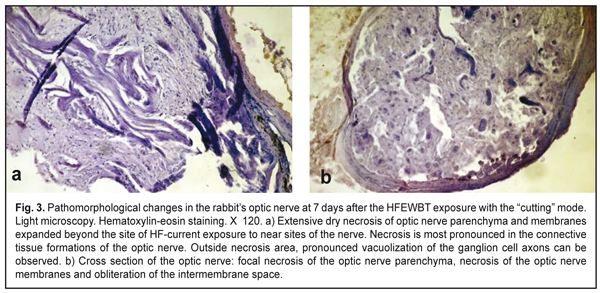
At Day 7 after the HFEWBT exposure to the optic nerve, we noted decreased edema in the optic nerve parenchyma, obliteration of the part of the optic nerve blood vessels; but, along with this, focal oval-shaped sites of basophilic degeneration of ganglion cell axons were revealed. The axon bundles were homogenized; the nuclei of the glial elements could not be detected. Small round aggregations of glial elements were merely noted, which evidenced of their proliferation and early gliosis of the optic nerve (Fig. 3A). Obliteration of the intermeningeal spaces and early signs of fibrosis in the sheaths were also noted (Fig. 3B). The necrosis band in the optic nerve parenchyma was approximately 1 mm wide.
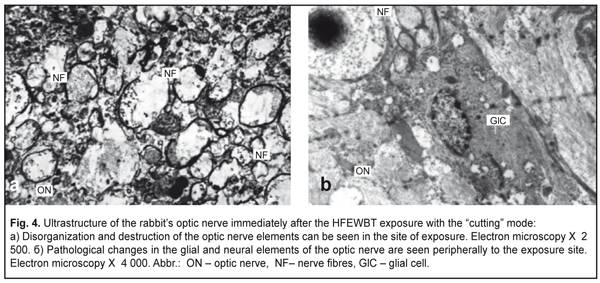
The ultrastuctural study of the Group 1 samples showed disorganization in the optic nerve structure in the exposure site as much as complete detritus and electron-transparent vesicles. Edematous changes were more pronounced than destructive ones (Fig. 4A). Peripherally to the HFEWBT exposure site, myelin sheathes were preserved but differed from the normal ones by separated fibers and homogenized sites. Axoplasm of the nerve fibers contained the destroyed remnants of intracellular structures and was swollen. The cells of the glia as well as their processes underwent destruction. Altered myelin sheathes, empty axoplasm, lysis of the glial cell processes were detected (Fig. 4B). Sites next to the HFEWBT exposure site had the similar pathological changes though they were less pronounced.
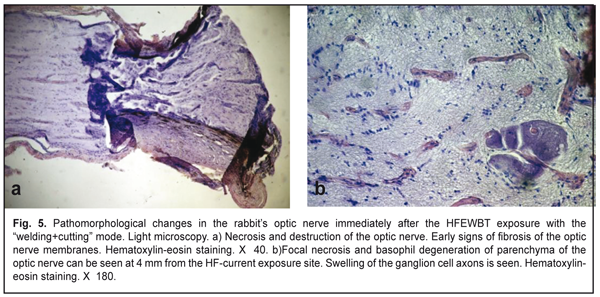
Effect of HFEWBT in the welding+cutting mode on the optic nerve in rabbits (Group 2) When using HF-current in the welding+cutting mode for the optic nerve transection, as early as the first day after the exposure we detected destructive changes which were more pronounced as compared to those when the cutting mode was used; the changes were in the optic nerve both directly in the exposure site and distantly as well as in the optic disc. The changes came down to the presence of coagulation necrosis in the optic nerve in the center of power; pyknosis of the nucleus in the ganglion cells; sites of complete tissue homogenization; and tissue basophilia. Herewith, there appeared numerous voids filled with the serous fluid (Fig. 5a). The optic nerve sheaths dissipated and were focally necrotized. A width of the necrosis band was significantly higher than that when the cutting mode was used and reached approximately 3-4 mm. In addition, secondary phenomena of degeneration of the ganglion cell axons were spread at a significantly greater distance: approximately 5 mm on either side from the center of power (Fig. 5b). At 7 days after the exposure, the swelling in the optic nerve tissues decreased. Meanwhile, the degenerative changes in the optic nerve parenchyma, microscopically manifested as focal sites of basophil degeneration of the ganglion cell axons, were preserved over the greater area.
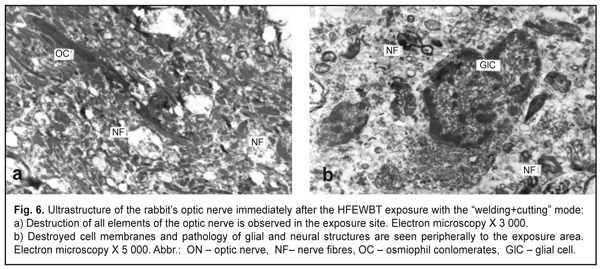
Ultrastructural studies focused on the HFEWBT exposure revealed disorganization in the optic nerve structure; destruction of almost all formations; cell debris; and structureless fragments. The samples were characterized by the presence of a great number of homogenized osmiophil elements which, apparantly, were formed as a result of adhesion of destroyed nerve fiber and glia cell fragments. Alteration and partial destruction involved both the nerve fibers and, especially, the glia cells (Fig. 6a). Destruction of the optic nerve elements were also expressed peripherally to the center of power. There were a less number of osmiophil conglomerates; however, myelin sheaths, preserved here, were homogenized and soldered together, or fragmented (Fig. 6b).
Discussion Pasyechnikova N.V. and colleagues [4, 6] have performed experimental studies on histomorphologic and ultrastructural changes in rabbit’s orbit tissues in standard practice enucleation using cutting instruments and in enucleation using HFEWBT with the cutting mode for the optic nerve transection and noted the absence of bleeding and 10 minute reduction of operating time in case of using HF-current as compared to the standard practice enucleation. Postoperative clinical signs of inflammation have been reported to be less pronounced and healing to be more promoted after using HFEWBT in the absence of any complications including thermal damage of surrounded tissues, deformation, necrosis, and increased scarring [10]. Pathohistological study of the optic nerve immediately after the optic nerve transection detected along the section line a dry necrosis band persisting even in a week’s time with the nearby development of focal edema of nerve tissues and obliteration of blood vessels [4, 10]. Ultrastructural study of optic nerve tissues under the cutting mode HF-current action showed the presence of an area of complete necrosis directly in the site of electrodes and, behind it, substance of denaturated proteins, destroyed optic nerve structures, myelin sheath coagulates, and damaged collagen fibrills of the optic nerve membranes [6,10]. Results of our experimental studies gave the evidence of a less traumatic course of surgery when using the HFEWBT method in both cutting and welding+cutting modes: the absence of bleeding from the ophthalmic artery; no need of the orbit tamponade; reduction of operating time and, subsequently, reduction of tissue edema; the absence of hematomas and other postop complications, which has been reported by other authors having used the HFEWBT method in the cutting mode for the optic nerve transection [2, 7, 10]. Our experimental studies of the two HFEWBT modes, cutting and welding+cutting, for transecting the optic nerve revealed, in both cases, dry necrosis in the optic nerve parenchyma and sheaths that developed not only in the site of the HFEWBT exposure, as pointed by Pasyechnikova and colleagues [4, 6], but also at the distance depending on the mode used. Herewith, HFEWBT in the “welding+cutting” mode caused 3-4 mm wide necrosis on either side from the exposure site, growing up by Day 7 after surgery, which two times exceeded the necrosis length after the cutting mode HFEWBT exposure (1-2 mm). Degeneration and gliosis of the optic nerve in Group 2 (welding+cutting) occurred within the greater area than that in Group 1 (cutting), reaching the optic disc and sensory retina. Ultrastructurally, we revealed the complete necrosis areas in the optic nerve tissues in using both HFEWBT modes. Behind the necrosis area, there was pathological substance of osmiophil conglomerates tightly bound with remnants of destroyed optic nerve ultrastructures, myelin sheath coagulates, and collagen fibrils of the optic nerve sheaths. Coagulative and homogenizing processes in biological tissues prevailed when using the welding+cutting mode compared to the cutting mode where edematic changes in the exposure site were mainly noted. Conclusions
Analysis of the light electron microscopy data showed that the HFEWBT method for transecting the optic nerve in eye enucleation in experimental animals, using both cutting and welding+cutting modes, led to the development of dry necrosis of the optic nerve parenchyma and sheaths, the length of which depended on the mode used. Herewith, the coagulative processes prevailed when using the welding+cutting mode and extended to a much greater distance as compared to the cutting mode, 4 mm vs. 1-2 mm, respectively. We believe that the increase of extension of the destructive changes when using the welding+cutting HFEVBT mode can increase the ablasticity of enucleation of the eyes with retinoblastoma at high risk of optic nerve invasion References
|