J.ophthalmol.(Ukraine).2018;1:3-6.
|
http://doi.org/10.31288/oftalmolzh2018136 Assessing the efficacy of surgical treatment for age-related cataract through risk factor analysis I.M. Bezkorovaina, Dr Sc (Med), Prof., I.S. Steblovska, Post-Grad Student Ukrainian Medical Stomatological Academy; Poltava (Ukraine) E-mail: irunasteblovska@gmail.com TO CITE THIS ARTICLE: Bezkorovaina IM, Steblovska IS. Assessing the efficacy of surgical treatment for age-related cataract through risk factor analysis. J.ophthalmol.(Ukraine).2018;1:3-6. http://doi.org/10.31288/oftalmolzh2018136
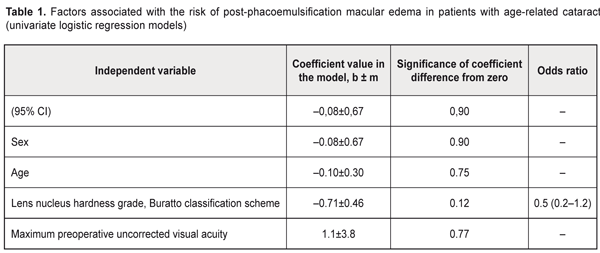
Background: Although conventional phaco and femtosecond laser-assisted cataract surgery are widely used treatment options, patients undergoing these approaches often experience peri- and post-operative complications that worsen functional outcomes. Cystic macular edema is one of these complications and occurs in 1-28% of patients. Purpose: To assess the efficacy of surgical treatment for age-related cataract through risk factor analysis using logistic regression models. Materials and Methods: Eighty-three eyes of 83 patients with age-related cataract (lens nuclei of grades 1 to 3, Buratto classification scheme) participated in the study. Aqueous humor samples were collected during phacoemulsification procedures and investigated for the presence of prostanoids, thromboxane B2 and prostacyclin 6-keto-PGF1α. A negative outcome of surgical treatment for cataract was defined as development of macular edema; any other outcome was considered positive. Results: 6-keto-PGF1α/ thromboxane B2 ratio can be used as a marker of the risk for developing macular edema 1 year after phacoemulsification for age-related cataract. Key-words: logistic regression models, age-related cataract, macular edema Introduction Although the advent of small incision cataract surgery and the development of phacoemulsification (phaco) have contributed to the reduction of postoperative complications, such vision-threatening complications as infectious endophthalmitis, toxic anterior segment syndrome, intraoperative suprachoroidal hemorrhage, cystic macular edema (CME), retinal detachment, persistent corneal edema and IOL dislocation can still occur during or after cataract surgery [1, 2]. CME, if persistent, leads to irreversible changes in the retinal pigment epithelium and retinal photoreceptors, with subsequent deterioration of visual function [3-6]. Conventional phaco and femtosecond laser-assisted cataract surgery are widely used treatment options. Unfortunately, patients undergoing these approaches often experience intra- and post-operative complications that worsen functional outcomes. CME is one of these complications and occurs in 1-28% of patients. Therefore, the need (1) to optimize surgical treatment of patients with age-related cataract based on studies on the features and mechanisms of postoperative macular edema, and (2) to develop a new technique for predicting this complication become clearly urgent. The purpose of the study was to assess the efficacy of surgical treatment of patients with age-related cataract through the risk factor analysis using logistic regression models. Materials and Methods Eighty-three patients (43 man and 40 women; age, 40 to 85 years; 83 eyes) with age-related cataract (soft lens nuclei of grades 1 to 3, Buratto classification scheme) participated in this retrospective study. All these patients underwent phacoemulsification with implantation of an Acrysof Natural IQ IOL (Alcon Laboratories, Inc., Fort Worth, TX) and were followed up for 12 months. Aqueous humor samples were collected during phacoemulsification procedures and investigated for the presence of prostanoids, thromboxane B2 and prostacyclin 6-keto-PGF1α. In addition, 6-keto-PGF1α/ thromboxane B2 ratios were calculated for samples collected. We used univariate logistic regression models to analyze the risk factors associated with (1) developing macular edema and (2) failing to attain maximum uncorrected visual acuity after phaco in patients with age-related cataract. Logistic regression models were built and analyzed to identify the risk factors associated with the failure to achieve positive outcomes following phacoemulsification. Statistical analyses were undertaken with MedStat software (developed by Lyakh and Gur’ianov, 2014-2012) and EZR software (version 1.35; Saitama Medical Center, Jichi Medical University, Saitama, Japan). We calculated risk ratio (RR), absolute risk reduction (ARR) and the 95% confidence intervals (CI) for the ARR. Spearmen correlation coefficients were calculated for each analysis. Binary logistic regression was used to investigate the relationship between a dichotomous variable and independent variables. Logistic regression models were developed to assess effects of independent variables on treatment outcomes. Receiver operator characteristic (ROC) curves were used to determine the ideal threshold values for individual parameters. Areas under the curve (AUC) values were calculated for the sensitivity and specificity, and 95% confidence intervals were calculated for each parameter. Odds ratios (OR) and 95% confidence intervals were calculated to assess effects of independent variables on treatment outcomes. Results and Discussion A negative outcome of surgical treatment for cataract was defined as development of macular edema during the follow-up; any other outcome was considered positive. In logistic regression analyses, the output variable (Y) was 0 if no macular edema (73 patients) or 1 if macular edema was present (10 patients) postoperatively, and sex, age, nucleus hardness grade and maximum preoperative uncorrected visual acuity were independent variables (risk factors). Table 1 presents the results of our risk factor analysis in univariate logistic regression models. There was no relationship between the risk of post-phacoemulsification macular edema and sex, age, and maximum preoperative uncorrected visual acuity in patients with age-related cataract (P > 0.05 for all; Table 1). The risk of post-phacoemulsification macular edema was, however, found to decrease with increasing hardness of the lens nucleus (P = 0.12). In addition, it was found that patients with low 6-keto-PGF1α/ thromboxane B2 ratios tended to develop post-phacoemulsification macular edema, and the mean ratio value was lower in patients with edema than in those without edema (0.577 ± 0.005 and 0.963 ± 0.008, respectively). In all former patients, the ratio value was less than 0.60, whereas in all latter patients, the ratio value was more than 0.80.
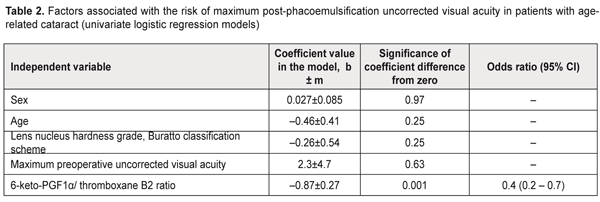
The efficacy of treatment (with regard to attaining maximum uncorrected visual acuity) was assessed 12 months after surgery. In logistic regression analyses, the output variable (Y) was 0 if the patient could achieve a visual acuity of 0.8–1.0 at 1 year after surgery (73 patients); otherwise the output variable was 1 (6 patients). In addition, sex, age, nucleus hardness grade, maximum preoperative uncorrected visual acuity and 6-keto-PGF1α/ thromboxane B2 ratio were independent variables (risk factors). Table 2 presents the results of our risk factor analysis in univariate logistic regression models. There was no relationship between the risk of failure to achieve a good maximum post-operative uncorrected visual acuity and sex, age, nucleus hardness grade, and maximum preoperative uncorrected visual acuity in patients with age-related cataract (Table 2; P > 0.05 for all). For every 0.1 point increase in 6-keto-PGF1α/ thromboxane B2 ratio, the risk of failure to achieve a good maximum post-operative uncorrected visual acuity was found to decrease (P = 0.001; OR, 0.4; 95% CI, 0.2–0.7). Therefore, 6-keto-PGF1α/ thromboxane B2 ratio can be used as a marker of the risk of failure to achieve a good maximum uncorrected visual acuity in cataract patients at 1 year after phacoemulsification.
Figure 1 demonstrates a ROC curve for 6-keto-PGF1α/ thromboxane B2 ratio in cataract patients at 1 year after phacoemulsification. The AUC for 6-keto-PGF1α/ thromboxane B2 ratio was 0.86 (95% CI, 0.77 – 0.93), thus demonstrating a strong relationship of 6-keto-PGF1α/ thromboxane B2 ratio with the risk of failure to achieve a good maximum uncorrected visual acuity in cataract patients at 1 year after phacoemulsification. The optimal cut-off value of 6-keto-PGF1α/ thromboxane B2 ratio of 0.86 (sensitivity, 83.3%, 95% CI, 35.9%–99.6%; specificity, 86.3%, 95% CI, 76.2% – 93.2%) was determined by maximizing the Youden index of the ROC curve. If the ratio value exceeds the cut-off point, one may predict that a visual acuity of 0.8-1.0 will be achieved by 12 months after phacoemulsification; otherwise the prognosis for achieving this visual acuity is unfavorable.
Conclusions First, 6-keto-PGF1α/ thromboxane B2 ratio can be used as a marker of the risk for developing macular edema 1 year after phacoemulsification for age-related cataract. Second, a direct correlation was found between 6-keto-PGF1α/ thromboxane B2 ratio and the risk of failure to achieve a good maximum uncorrected visual acuity in cataract patients at 1 year after phacoemulsification. Finally, the optimal cut-off value of 6-keto-PGF1α/ thromboxane B2 ratio was found to be 0.86 (sensitivity, 83.3%, 95% CI, 35.9%–99.6%; specificity, 86.3%; 95% CI, 76.2% – 93.2%).
References
|