J.ophthalmol.(Ukraine).2016;6:50-56.
|
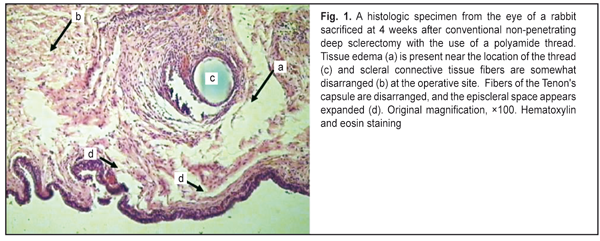
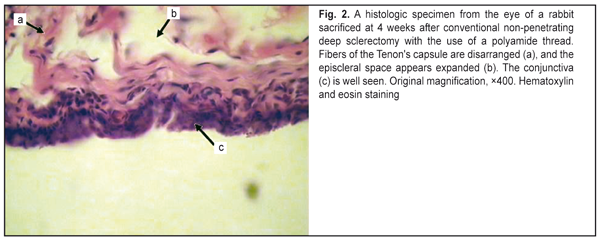
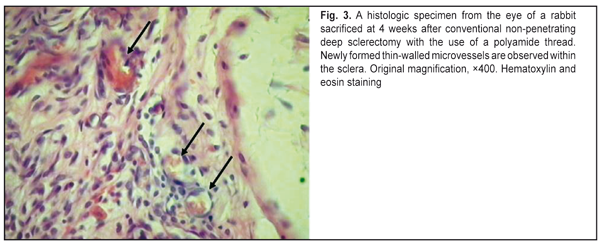
https://doi.org/10.31288/oftalmolzh201765056 Experimental substantiation of modified non-penetrating deep sclerectomy for primary open-angle glaucoma E.A. Ivachev, Ophthalmologist Railroad Clinical Hospital at the Penza station, Russian Railways JSC E-mail: eivachov1@yandex.ru Background: Excessive bleb scarring is the main cause of reduced hypotensive effect after conventional non-penetrating deep sclerectomy (NPDS). We have developed a modification of NPDS with implantation of a drainage device to reduce this scarring. Purpose: To investigate morphologically the inflammatory response and scarring at the operative site after conventional NPDS and modified NPDS (MNPDS) with implantation of different drainage devices in rabbits. Materials and Methods: The animals of Groups I and 3 underwent manipulations similar to conventional NPDS (with implantation of either a 5-0 polyamide thread or Xenoplast drainage device, respectively), whereas those of Groups 2 and 4 underwent manipulations similar to MNPDS (with implantation of either a 5-0 polyamide thread or Xenoplast drainage device, respectively). Results: At week 4, the reparative process in the animals of Group 1 was not yet complete (with insubstantial inflammatory changes still present, mostly around a foreign body), whereas that in the animals of Group 2 was practically complete. In addition, in the animals of Group 3, the process was significantly hindered by active exudative inflammation, whereas in the animals of Group 4, the inflammatory changes were less pronounced. Conclusion: The technique of MNPDS reduces postoperative bleb scarring and results in a shorter reparative process at the filtering site compared to that in conventional NPDS. Extensive dissection of the conjunctiva from the episclera and episcleral diathermocoagulation result in a longer reparative process at the operative site. Incorporation of either type of drainage device (polyamide thread or Xenoplast) into the intrascleral space results in a stable dilatation of the space and prevents the adhesion between the roof and the bed of the scleral tunnel. Keywords: glaucoma, surgical treatment, non-penetrating deep sclerectomy, morphologic changes at the operative site Introduction Non-penetrating glaucoma surgery is a popular approach to lowering intraocular pressure. Although conventional non-penetrating deep sclerectomy (NPDS) has a number of advantages (like microinvasiveness, low complication rate, and controlled intraoperative IOP reduction), ocular hypertension is common after this procedure. Aqueous humor passes through the intrascleral channel into the subconjunctival space, thus forming a bleb. Some studies have demonstrated that the subconjunctival pathway is a leading aqueous outflow pathway [1, 2] after conventional NPDS. Excessive bleb scarring is the main cause of reduced hypotensive effect after NPDS. Inflammatory response to surgical intervention in the presence of glaucomatous changes in the ocular tissues leads to accelerated scarring of the newly formed aqueous outflow pathways, thus resulting in recurrent IOP elevation. Bakunina et al [3] proposed to excise the episcleral and conjunctival connective tissue as a source of proliferating fibroblasts during NPDS in order to reduce scarring at the site of aqueous humor filtration. They have reported that the hypotensive effect of their approach has been maintained for up to 3 years. The techniques with the reduced surgical area have been described as an approach for combating excessive scarring at the surgical site [4, 5]. We have obtained a patent for the modified non-penetrating deep sclerectomy (MNPDS) with implantation of a drainage device (Pat. of Russia №2,539,554 issued 10.07.2013) for patients with primary open-angle glaucoma. The method consists in isolating the filtering site from the operative site without the use of coagulation in the absence of a free scleral flap [6]. The purpose of this study was to investigate morphologically the inflammatory response and scarring at the operative site after conventional NPDS and MNPDS with implantation of different drainage devices in rabbits. Materials and Methods Animal studies were conducted at the vivarium of the Penza State Agricultural Academy. All animal experiments, care and handling were performed in compliance with Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the Protection of Animals Used for Scientific Purposes, and Order No. 267 of the Russian Ministry for Health of 19 June 2003 on Approval of Regulations for Laboratory Practice. Twenty Chinchilla adult male rabbits, divided into four groups of five animals each, were used in this experimental study. The animals of Groups I and 3 underwent manipulations similar to conventional NPDS (with implantation of either a 5-0 polyamide thread or Xenoplast drainage device, respectively), whereas those of Groups 2 and 4 underwent manipulations similar to MNPDS (with implantation of either a 5-0 polyamide thread or Xenoplast drainage device, respectively). Polyamide thread is a synthetic nonabsorbable suture material that measures 0.100-0.149 mm in diameter, with no reaction in the adjacent tissue. Xenoplast drainage device is made of porous collagen derived from bone tissues of agricultural animals. It measures 4.0?1.5?0.5–0.8 mm, and is nonabsorbable, non-toxic and immunogenic. In both eyes of Group 1 rabbits, the conjunctiva was dissected from the episclera, and a high-frequency electrosurgical unit Fotek E80 was used in bipolar coagulation mode (exposure duration, 0.5 s; power setting, 3 W) to produce 20 coagulation lesions at the episcleral surface. A 5x5 mm scleral flap including one-third of scleral thickness, was separated from the sclera, and a 5-0 polyamide thread was placed underneath it. Thereafter, this area was covered with the bulbar conjunctiva that was secured with a running suture. Both eyes of Group 3 rabbits were subjected to the same manipulations as those of Group 1 rabbits; however, a Xenoplast collagen drainage device, and not polyamide thread, was implanted in the scleral bed. In both eyes of Group 2 rabbits, a 2.2-mm keratome was used to create a 3-mm-long intrascleral anterior–posterior tunnel. The keratome was introduced at the limbus and advanced through the sclera to the subconjunctival space. A 5-0 polyamide thread was placed in the created tunnel. Thereafter, the conjunctiva was secured with a running suture. In both eyes of Group 4 rabbits, the intrascleral tunnel was formed in a fashion similar to that of Group 2; however, a Xenoplast collagen drainage device, and not polyamide thread, was implanted in the tunnel. Postoperatively, all animals received conservative therapy (instillation of antibacterial agents) for 2 weeks. The animals were euthanized by air embolism at four weeks after surgery. Enucleated globes were fixed in 10 % neutral formalin. The operative area was removed, defatted and dehydrated in ascending grades (50, 80, 96, and 100%) of alcohol, and embedded in a 1:1 acetone and paraffin mixture and then in pure paraffin. A paraffin block was created from each sampling, and cut for 4-6-µm sections to obtain 5 slides stained with hematoxylin and eosin. Five photographs per slide were taken using a Zeiss Axioskop microscope equipped with a Zeiss Axiocam digital camera. Results and discussion Group 1 The animals of Group I underwent manipulations similar to conventional NPDS with implantation of a 5-0 polyamide thread. We found that, in the slides of the animals of this group, scleral connective tissue fibers were somewhat disarranged, with some fibers exhibiting an abnormal structure, and tissue edema was still present (Fig.1). Fibers of the Tenon's capsule were disarranged, and the episcleral space appeared expanded (Fig. 2). Three to four lymphocytes were occasionally observed in the field of vision with a high magnification. Fibroblasts were the most abundant immune cell type identified in the specimens. Numerous newly formed microvessels were observed (Fig. 3).
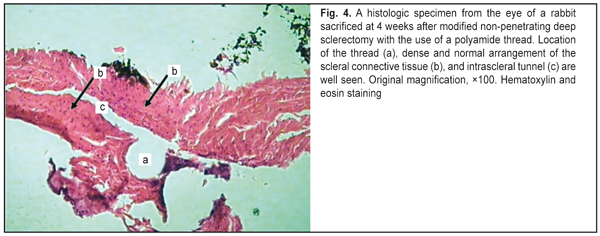
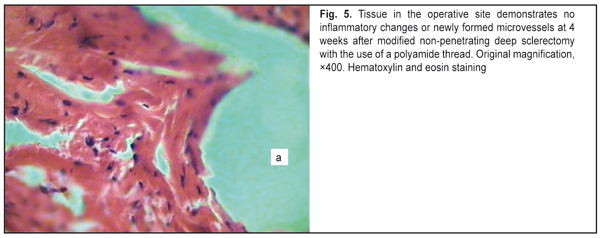
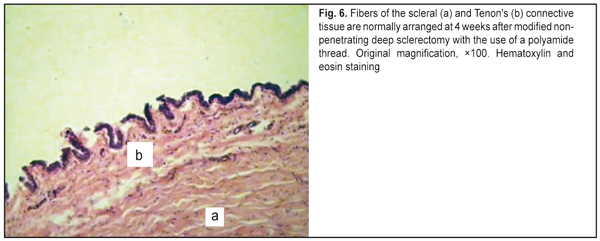
Therefore, these slides give evidence that, by week 4, the reparative process was not yet complete, and, moreover, insubstantial inflammatory changes were still present (mostly around a foreign body). This is attributable to the use of the dissection of the conjunctiva, episcleral diathermocoagulation, and cutting of a U-shaped scleral flap. Group 2 The animals of Groups 2 underwent manipulations similar to MNPDS with implantation of a 5-0 polyamide thread. In the slides of the animals of this group, no signs of inflammatory changes (like leukocyte lineage cells or edema of the fibrous tissue) were observed (Fig. 4). In addition, the numbers of fibroblasts (the cells that actively produce the fibrous component of the connective tissue) and fibrocytes (definitive, non-active forms) were practically equal (Fig. 5), and no newly formed microvessels were observed. Fibers of the scleral and Tenon's connective tissue were normally arranged (Fig. 6), and the episcleral space did not appear expanded.
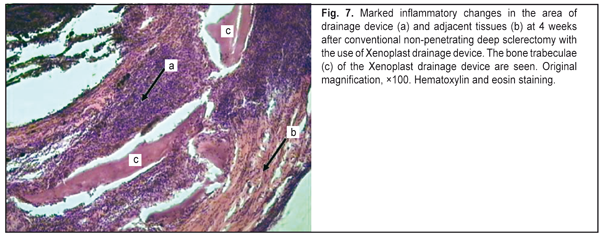
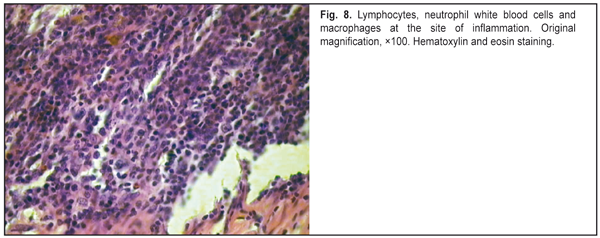
Therefore, these slides give evidence that, after MNPDS with the use of a polyamide thread, the reparative process in the rabbit’s eye were rather fast, and, by week 4, were practically complete. This is attributable to (a) the absence of the use of the dissection of the conjunctiva or episcleral diathermocoagulation, and (b) shaping of the intrascleral tunnel without cutting a superficial scleral flap. Group 3 The animals of Group 3 underwent manipulations similar to conventional NPDS with implantation of a Xenoplast drainage device. Marked inflammatory changes were found in the specimens from these animals. Leukocyte lineage cells were found to fill all the gaps in between the bone trabeculae of the draining device (Fig. 7) and to infiltrate a large connective tissue area surrounding the device (Fig. 8). There was separation of fibers of scleral and Tenon’s connective tissue that appeared acutely edematous, and the episcleral space appeared expanded.
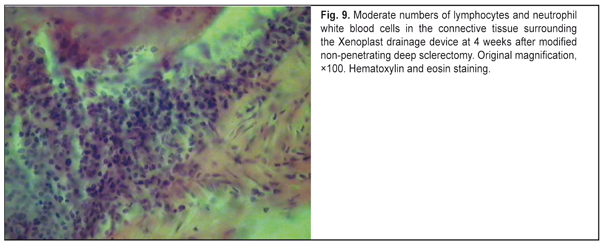
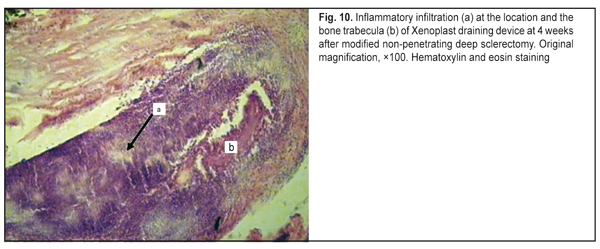
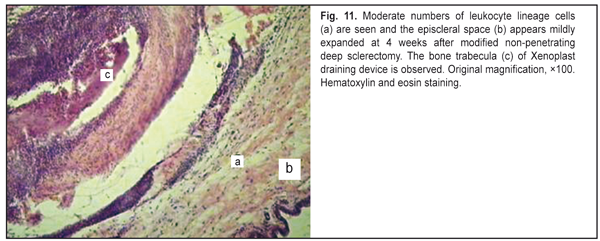
Therefore, in the animals of Group 3, the reparative process was significantly hindered by active exudative inflammation, that is attributable to the use of the dissection of the conjunctiva, episcleral diathermocoagulation, cutting of a U-shaped scleral flap, and the presence of Xenoplast. Group 4 The animals of Group 4 underwent manipulations similar to MNPDS with implantation of a Xenoplast drainage device. In the slides of the animals of this group, mild inflammatory changes were observed, with lymphocytes and neutrophil white blood cells but not macrophages seen in the operative site (Fig.9). Although leukocyte lineage cells were found to fill all the gaps in between the bone trabeculae of the draining device (Fig. 10), they were present in small numbers in adjacent tissues (Fig. 11). Numerous fibroblasts and moderate numbers of fibrocytes were seen in the connective tissue. Disorganisation of connective tissue fibers was less apparent than in Group III, and the episcleral space appeared mildly expanded.
Therefore, in the slides of the animals of Group 4, the inflammatory changes were less pronounced than those observed for the animals of Group 3, and were attributable to the use of the dissection of the conjunctiva, episcleral diathermocoagulation, and formation of the inrascleral tunnel without cutting a superficial scleral flap. We would like to highlight several points related to the glaucoma surgery technique which promote postoperative scarring, thus decreasing the hypotensive effect. In conventional non-penetrating deep sclerectomy, the bleb is formed at the operative site, i.e., it is located in the same area as the operative site. That means that bleb formation will be directly associated with the amount of intraoperative trauma. The amount of intraoperative trauma, in its turn, depends on the surface area of dissection of the conjunctiva from the episclera, amount and power of episcleral diathermocoagulation, and the size of the scleral flap. These manipulations are performed in the area of subsequent bleb formation, and thus influence scarring in the area [3, 7-10]. Intraoperative use of diathermocoagulation leads to marked local inflammatory response with massive cellular tissue infiltration, thus resulting in a longer reparative period for the operative area, and, consequently, in increased scarring of newly formed aqueous outflow pathways [11]. In addition, the surface area of separation of the conjunctiva from the episclera influences the subsequent size and shape of the bleb, as the velocity and amount of fluid resorbed through the conjunctival and episcleral vessels are higher in diffused blebs [12]. Studies on scarring at the operative site have demonstrated that, in conventional NPDS, the superficial scleral flap is involved in postoperative inflammation with subsequent cicatrization, thus resulting in deformation of the flap with obstruction of the intrascleral cavity [13]. We have developed the basic technological principles of modified non-penetrating deep sclerectomy (isolation of the filtering site from the operative site; no need for creating a superficial scleral flap or using diathermocoagulation at the filtering site; forming an intrascleral pocket; and the potential using of various drainage devices) in order to prevent excessive scarring at the filtering site. Conclusions First, the technique of modified non-penetrating deep sclerectomy reduces postoperative bleb scarring and results in a shorter reparative process at the filtering site compared to that in conventional non-penetrating deep sclerectomy. Second, extensive dissection of the conjunctiva from the episclera as well as episcleral diathermocoagulation results in a longer reparative process at the operative site. Finally, incorporation of either type of drainage device (polyamide thread or Xenoplast) into the intrascleral space results in a stable dilatation of the space and prevents the adhesion between the roof and the bed of the scleral tunnel. References
|