J.ophthalmol.(Ukraine).2017;5:45-49.
|
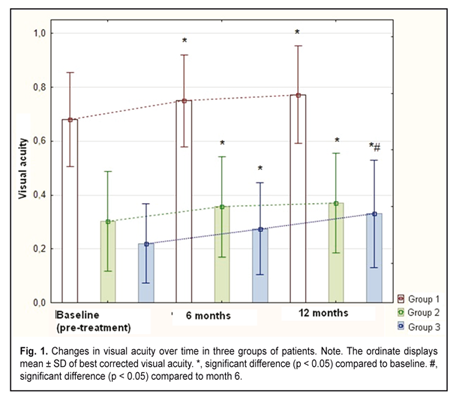
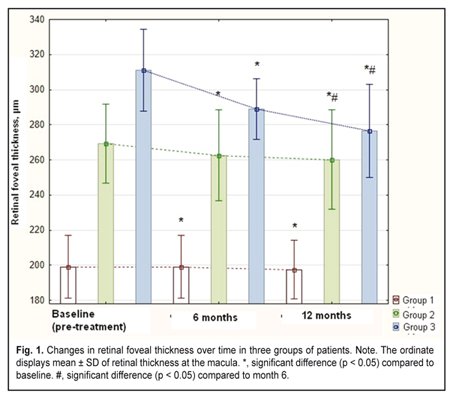
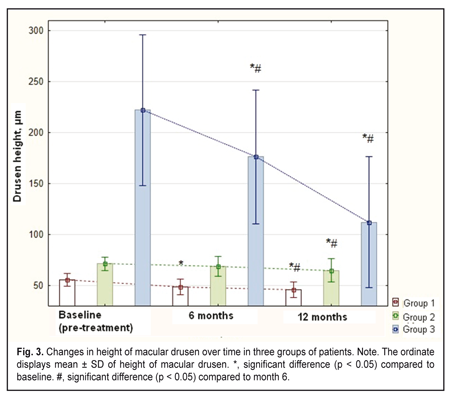
https://doi.org/10.31288/oftalmolzh201754549 Efficacy of 577-nm retinal pigment epithelium laser photocoagulation in age-related maculopathy patients with various extents of morphological and functional loss S.A. Fedchenko, Ophthalmologist, Post-grad Student, O.S. Zadorozhnyy, Cand Sc (Med), A.R. Korol, Dr Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy E-mail: laserfilatova@gmail.com Background: There is no unanimously adopted approach to titrating laser settings in subthreshold retinal laser photocoagulation (LPC) without ophthalmoscopically visible fundus changes. The efficacy of this approach to treatment of retinal diseases is still to be investigated. Purpose: To investigate the efficacy of 577-nm RPE LPC in the treatment of age-related maculopathy (ARM) with various extents of morphological and functional loss. Materials and Methods: The study involved 57 patients (57 eyes) diagnosed with ARM. 577-nm micropulse laser photocoagulation was applied to the RPE at the macula. Patients were followed-up for 12 months. Results: Three groups of ARM eyes with a similar extent of morphological and functional loss at baseline were created using Ward’s clustering method. Changes in visual acuity, retinal foveal thickness diameter and height of macular drusen, as well as incidences of subretinal neovascularization (SNV) and geographic atrophy over the follow-up for the groups were investigated. We observed no cases of SNV or geographic atrophy during the follow-up. Conclusions: 577-nm micropulse RPE laser photocoagulation with power titrated in micropulse mode was found to be efficacious and safe treatment for ARM patients with a wide variation in the extent of morphological and functional loss, including patients with drusenoid pigment epithelium detachment. Key-words: micropulse laser photocoagulation, retinal pigment epithelium, age-related maculopathy Introduction Because of poor natural outcomes of age-related macular degeneration (AMD), and given the ever increasing prevalence of the disease, the approaches to preventive treatment at early stages of age-related maculopathy (ARM) are of special interest [1-3]. Conventional retinal laser photocoagulation is known to carry a risk of side effects and may be followed by visual field alterations, reduction in contrast sensitivity, and development of subretinal neovascularization (SNV) [4, 5]. It is considered that it is not necessary to damage all retinal layers in order to achieve therapeutic efficacy of laser [6]. Thus, 532-nm indirect selective retinal pigment epithelium (RPE) laser photocoagulation (LPC) has been reported to be efficacious in AMD [7]. In addition, subthreshold RPE photocoagulation with millisecond pulses from 577-nm or 810-nm laser has been found beneficial in various macular disorders [5, 6, 8, 9]. Therefore, retina-sparing laser photocoagulation can be considered as an alternative to conventional laser treatments in macular diseases like ARM. The purpose of this study was to investigate the efficacy of 577-nm RPE LPC in the treatment of ARM with various extents of morphological and functional loss. Materials and Methods This was a prospective open non-controlled study on the effect of 577-nm micropulse laser photocoagulation on the retina of patients with ARM. The study was conducted at the Laser Department of the Filatov Institute and involved 57 patients (57 eyes) diagnosed with ARM. 577-nm micropulse laser photocoagulation was applied to the RPE at the macula. The primary aim was to assess the changes in visual acuity and retinal morphology at month 12 after 577-nm micropulse laser photocoagulation of the RPE at the macula. In addition, we aimed to assess the incidences of subretinal neovascularization (SNV) and geographic atrophy during the follow-up. At baseline and at months 6 and 12, patients underwent examination including best-corrected visual acuity (BCVA) assessment, color fundus photography, optical coherence tomography (OCT; SOCT Copernicus OPTOPOL Technology S.A., Zawiercie, Poland) and retinal fluorescein angiography (FA; TRC-50EX; Topcon, Tokyo, Japan). OCT data were used to derive (1) retinal foveal thickness (RFT) and (2) diameter and height of macular drusen. Diameter and height of macular drusen were measured manually using the electronic caliper from the Copernicus software. Only the largest druse or drusenoid retinal pigment epithelium detachment (DPED) present in the eye was considered. DPED was defined as per the AREDS study,[10] as a well-defined, pale yellow or white, large mound consisting of many large drusen or confluent drusen which was at least 350 microns in the narrowest diameter and appeareds elevated on stereoscopic fundus photographs. FA was used to reveal the signs of SNV in the macula. All procedures were performed by one surgeon, with the laser delivered through the central part of a Goldmann three-mirror lens. The 577-nm Supra laser (Quantel Medical, Clermont-Ferrand, France) was used in the study. In micropulse laser treatment, the laser was switched to micropulse mode at 15% duty cycle (pulse train (burst time), 0.3 s; 0.17 ms ON, 1 ms OFF). Laser power was adjusted with the laser applied along the course of the vascular arcades, until grade 1 burn (according to the L'Esperance’s classification) was obtained at the site of laser exposure. The eye was treated with a laser power halved to become 0.15 W to 0.45 W [11]. The laser spot size was maintained at ~100 ?m. Laser was applied to the druzen-free areas of the non-foveolar macula (i.e., with the use of indirect laser photocoagulation). All patients were followed up for 1 year and received no laser re-treatment. Statistical analysis Cluster analysis (Ward’s method with Manhattan distance and k-means clustering) was used to determine groups of patients with similar morphological and functional values. Group means and standard deviations (SD) were calculated for all variables. Student t test and Mann-Whitney U test were used for intergroup comparisons. Statistical analysis was performed using STATISTICA 10 software (StatSoft, Inc.). Results Given a significant heterogeneity of the cohort (in terms of investigated parameters), Ward’s clustering was used to create three groups of patients eyes with a similar extent of morphological and functional loss. It is noteworthy that k-means clustering led to the same cluster solution. Group 1 (mild baseline morphological and functional loss) involved 22 eyes having mean visual acuity of 0.68 ± 0.17, mean RFT of 203 ± 19.7 ?m, and mean drusen height of 55.5 ± 6.3 ?m at baseline. Group 2 (moderate baseline morphological and functional loss) involved 25 eyes with mean visual acuity of 0.3 ± 0.2, mean RFT of 269 ± 22.6 ?m, and mean drusen height of 71.5 ± 6.7 ?m at baseline. Group 3 (DPED group; severe baseline morphological and functional loss) involved 10 eyes with mean visual acuity of 0.22 ± 0.15, mean RFT of 311 ± 23 ?m, mean DPED height of 222.5 ± 74 ?m, and mean DPED diameter of 1032 ± 475 ?m at baseline. There were statistically significant differences (p < 0.01) in each of the parameters between groups; the only exception was the difference (p = 0.22) in visual acuity between Group 2 and Group 3.
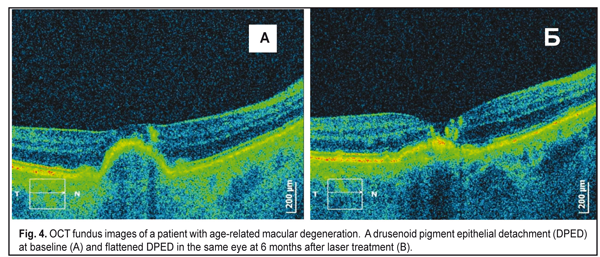
At 12 months, visual acuities in eyes of Group 1, Group 2 and Group 3 improved to 0.77 ± 0.18 (t test for paired samples, p = 0.0001), 0.37 ± 0.18 (p = 0.002), and 0.33 ± 0.2 (p = 0.01), respectively. In addition, in eyes of Group 1, Group 2 and Group 3, RFT improved (Fig. 2) to 197.5 ± 16.6 ?m (t test for paired samples, p = 0.0003), 260 ± 28.3 ?m (p = 0.0009), and 276.5 ± 27 ?m (p = 0.008), respectively, and drusen height decreased (Figs. 3, 4) to 45.7 ± 7.7 ?m (p = 0.00001), 65.1±12 ?m (p = 0.0004), and 112.2±64.2 ?m (p = 0.0004), respectively.
Over the follow-up period, we observed no cases of SNV or geographic atrophy in patients of the study. Discussion Authors vary in their views on how 577-nm micropulse subthreshold laser photocoagulation should be used for retinal disorders and demonstrate various approaches to titration of laser power parameters [1, 4, 7, 8, 12, 13]. We believe that the most expedient approach to titration of laser power parameters for micropulse subthreshold laser treatment is to titrate power levels in micropulse mode, and to decrease the power once the power level threshold has been identified [8, 11, 14]. Therefore, with this approach, the effect of subthreshold micropulse laser applied in the absence of retinal photocoagulation lesions becomes more predictable. The approach was mathematically substantiated and validated in our previous study on the ultrastructural changes in the rabbit chorioretinal complex following 577-nm micropulse laser photocoagulation of the fundus [11, 14]. Gatsu et al [4] (2014) reported on the outcomes of various laser treatments for soft macular drusen in dry AMD. They used 810-nm and 532-nm lasers in subthreshold micropulse modes to deliver laser energy to the non-foveolar macula drusen-free areas and in between them, and found subthreshold micropulse laser photocoagulation to be ineffective for soft macular drusen. Unfortunately, those authors did not specify the laser power titration procedure. In that study, however, indirect subthreshold laser photocoagulation (STLPC) and direct STLPC were found to be equally effective in terms of regression of small, soft confluent macular drusen, but resulted in no improvement in retinal functional parameters. In addition, a distinct type of drusen (so-called PED-like drusen, i.e. resembling pigment epithelium detachment) of the size greater than 800 ?m, did show an improvement in the morphological appearance as well as retinal function with direct treatment [4]. In the current study, we found improvements in morphological parameters and visual function at 12 months after indirect laser photocoagulation with a 577-nm laser in micropulse mode in patients with DPEDs greater than 350 ?m in diameter. Pasyechnikova et al [7] found selective RPE photocoagulation with millisecond pulses from a 532-laser to be efficacious for ARM, with decreased drusen height and improved visual function post treatment. In that study, drusen height and visual function, although did not change significantly in Group 1 (BCVA of 0.7 or better; RFT ? 200 ?m; and drusen height ? 60 ?m at baseline), did change significantly in Groups 2 and 3 (BCVA worse than 0.7; RFT > 200 ?m; and drusen height > 60 ?m at baseline) after treatment. In the current study, patients with mild baseline morphological and functional loss (Group 1; mean visual acuity of 0.68±0.17, mean RFT of 203 ± 19.7 ?m, and mean drusen height of 55.5±6.3 ?m) demonstrated improvement in visual function and retinal morphology after subthreshold laser micropulse photocoagulation with a 577-nm laser. In addition, decreased drusen height and improved vision were also demonstrated in patients of Groups 2 and 3 at 12 months. A 10% incidence of SNV was seen by Gatsu et al [4] at month 12 after indirect subthreshold laser treatment of drusen. In the study of Pasyechnikova et al [7], no patient with ARM developed SNV during the 2-year follow-up after indirect selective RPE photocoagulation. In the present study, we observed no cases of SNV or geographic atrophy during the 12-month follow-up. Conclusions First, clustering was used to create three groups of age-related maculopathy eyes with a similar extent of morphological and functional loss at baseline, Group 1 (mean BCVA, 0.68±0.17; mean RFT, 203 ± 19.7 ?m; mean drusen height, 55.5±6.3 ?m), Group 2 (mean BCVA, 0.3 ± 0.2; mean RFT, 269 ± 22.6 ?m; mean drusen height, 71.5 ± 6.7 ?m), and Group 3 (mean BCVA, 0.22 ± 0.15; mean RFT, 311 ± 23 ?m; mean DPED height, 222.5 ± 74 ?m; mean DPED diameter, 1032 ± 475 ?m). Second, 577-nm micropulse RPE laser photocoagulation with power titrated in micropulse mode was found to be efficacious and safe treatment for age-related maculopathy patients with a wide variation in the extent of morphological and functional loss, including patients with drusenoid pigment epithelium detachment.
Finally, in the present study, we observed no cases of SNV or geographic atrophy during the 12-month follow-up. References 1. Pasyechnikova NV, Ivanitska OV, Katsan SV. [Optimizing the management of macular drusen in age-related maculopathy]. Naukovyi visnyk Uzhgorods’kogo universitetu. 2004;22:75-78. Ukrainian 2. Bressler SB, Maguire MG, Bressler NM, et al. Relationship of drusen and abnormalities of the retinal pigment epithelium to the prognosis of neovascular macular degeneration. The Macular Photocoagulation Study Group. Arch Ophthalmol. 1990;108:1442–7. 3. Klein R, Peto T, Bird A, et al. The epidemiology of age-related macular degeneration. Am J. Ophthalmol. 2004;137:486–95. 4. Gatsu MV, Gordeyeva MV. [Modern concepts of laser treatment of soft macular drusen]. Oftalmologicheskie vedomosti. 2014;7(1):72-81 Russian 5. Youssef PN, Sheibani N, Albert DM. Retinal light toxicity. Eye (Lond). 2011 Jan; 25(1): 1–14. 6. Roider J, Brinkmann R, Wirbelauer C, et al. Subthreshold (retinal pigment epithelium) photocoagulation in macular diseases: a pilot study. Br J Ophthalmol. 2000;84(1):40–7 7. Pasyechnikova NV, Katsan SV, Maltsev EV. [Indirect selective laser photocoagulation for age-related maculopathy: Results and mechanisms of action]. Oftalmol Zh. 2008;3:10-12. Russian 8. Scholz P, Ersoy L, Boon CJ, Fauser S. Subthreshold Micropulse Laser (577 nm) Treatment in Chronic Central Serous Chorioretinopathy. Ophthalmologica. 2015;234(4):189-94 9. Yadav N, Jayadev C, Mohan A, et al. Sub-threshold micropulse yellow laser (577 nm) in chronic central serous chorioretinopathy: safety profile and treatment outcome. Eye (Lond). 2015 Feb; 29(2): 258–65. 10. Cukras C, Agr?n E, Klein ML, et al. Natural history of drusenoid pigment epithelial detachment in age-related macular degeneration: Age-Related Eye Disease Study Report N?. 28. Ophthalmology. 2010 Mar;117(3):489–499. 11. Fedchenko SA, Zadorozhnyy OS, Molchaniuk NI, Korol AR. [Ultrastructural changes in the rabbit chorioretinal complex following 577-nm laser photocoagulation]. Oftalmol Zh. 2017;4:51-5. Russian 12. Romanova TA. [The ultrastructural changes of the choroid and retinal pigment epithelium of rabbits after exposure to subthreshold lasers with 532nm, 577 nm, and 810 nm wavelengths using millipulse and micropulse laser modes]. Kharkivska khirurgichna shkola. 2014;4:74-9. Russian 13. Maia A. A New Treatment for Chronic Central Serous Retinopathy. Retina Today. 2010 Jan-Feb (1):1-3. 14. Semenyuk V. Thermal interaction of multi-pulse laser beam with eye tissue during retinal photocoagulation: Analytical approach. Int J Heat Mass Transf. 2017;112(1):480-488.
|