J.ophthalmol.(Ukraine).2017;5:56-59.
|
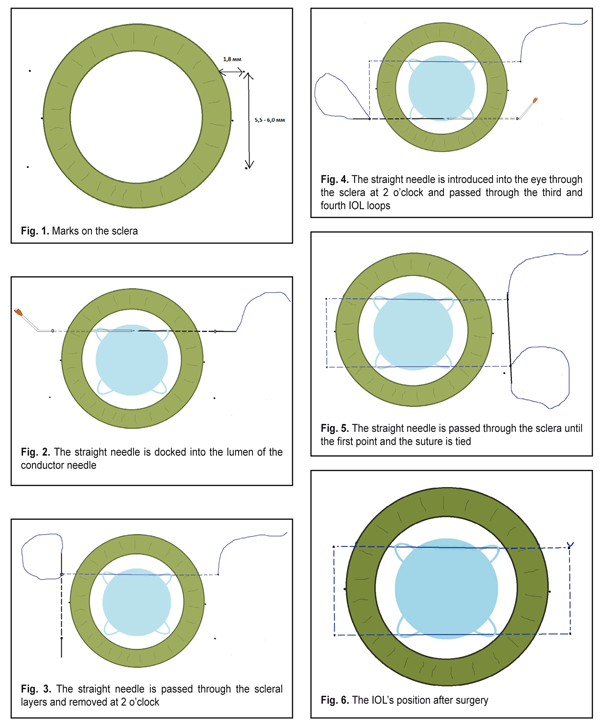
https://doi.org/10.31288/oftalmolzh201755659 The method of four-point fixation of the intraocular lens in the absence of capsular support (preliminary study) I.Ya. Novytskyy, Dr Sc (Med), Prof. Oculus Ophthalmic Clinic Lviv (Ukraine) E-mail: Inovytskyy@gmail.com Introduction. Fixation of an intraocular lens (IOL) in the absence of capsular support is still a challenge for ophthalmic surgeons. Purpose. To develop a technique of four-point IOL fixation in the absence of capsular support and to study its effectiveness. Material and methods. We developed a new technique of four-point fixation of the IOL for the cases of capsular bag loss and used this technique in 5 consecutive cases. An IOL with four loops was inserted into the chamber anterior under viscoelastic protection. A straight needle attached to a 10–0 polypropylene suture was introduced through the sclera 1.8 mm posterior to the limbus at 8 o'clock and was passed through the first and second loops and then was withdrawn from the opposite side 1.8 mm posterior to the limbus. Then needle was passed through the sclera and the same procedure was repeated for the third and fourth loops. The needle was passed through the sclera to the first point and the polypropylene sutures were gently pulled and tied. Results: Postoperative period was without complication. The IOLs in all cases were stable with proper centration. The postoperative best-corrected visual acuity ranged from 0.3 to 0.9 depending on secondary pathology. Conclusion. The technique of four-point fixation of the posterior chamber IOL is effective in cases of capsular bag loss. This technique provides good IOL fixation without creating a corneal wound or a scleral flap. Key-words: absence of capsular bag, four-point fixation of the intraocular lens Background Fixation of an intraocular lens (IOL) in the absence of capsular support is still a challenge for ophthalmic surgeons. A number of problems to be solved occur, in particular, proper IOL centration along the visual axis and inhibiting a tilt of the IOL (fixation parallel to the iris surface). Of hardly less importance are fixation stability and minimal injury rates of the procedure. A maximal simplicity of a method is important for its wide using. So, a search for new IOL fixation methods for cases when capsule support is absent continues to be a current issue of ophthalmology. The purpose of the present paper was to develop a technique of four-point fixation of the IOL in the absence of capsule support and to study its efficacy. Material and Methods We developed a surgical technique as follows: An anterior-chamber IOL with four loops is inserted into the anterior chamber under viscoelastic protection. The conjunctiva is separated from the limbus in sections at 2-4 o’clock and at 8-10 o’clock. The sclera is marked in such a way that the four marks at 8, 4, 2, and 10 o’clock are placed at the distance of 1.8 mm from the limbus and 3 mm from the horizontal meridian (Fig. 1). A straight needle with 10-0 polypropylene is introduced into the eye through the sclera at 8 o’clock and advanced behind the iris until it is seen behind the pupil. Then, the needle is passed through the first IOL loop from the bottom upwards and through the second loop from top downwards. From the opposite site, a 23-gauge needle, which is used as “a conductor”, is introduced into the eye through the sclera at 4 o’clock. The straight needle is docked into the lumen of the conductor needle (Fig. 2) and both needles are removed together from the eye at 4 o’clock. Then, the straight needle is passed through the scleral layers and removed at 2 o’clock (Fig. 3). Likewise, the straight needle is introduced into the eye through the sclera at 2 o’clock and passed through the third and fourth IOL loops (Fig. 4) and removed through the sclera at 10 o’clock. Then, the needle is passed through the scleral layers and removed at the first point at 8 o’clock; the suture is tied (Fig. 5). So, the IOL is fixed on two string-ling sutures (Fig. 6). To achieve an accurate centration along the visual axis, the IOL can be shifted in a horizontal plane. Viscoelastic is washed out by aspiration and irrigation.
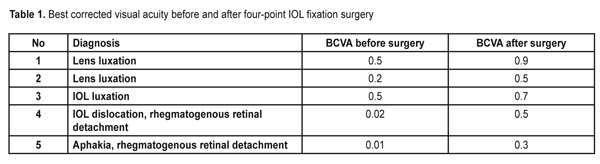
Five patients (5 eyes) were operated on using the technique above: two patients with traumatic lens luxation to the vitreous; one patient with IOL luxation to the vitreous; one patient with IOL dislocation with wide defects of the posterior capsule, anterior capsule fibrosis, planar synechiae and rhegmatogenous retinal detachment (we had to remove the lens capsule during the anterior segment reconstruction); one patient with aphakia and rhegmatogenous retinal detachment. Table 1 gives the data on pre-operative best-corrected visual acuity. Hypertension was noted in one patient with traumatic lens luxation to the vitreous due to pupillary block by the vitreous. The two patients with lens luxation were performed pars plana vitrectomy, lens phacoemulsification, IOL implantation using the fixation technique as described above. The patient with IOL luxation to the vitreous was performed pars plana vitrectomy; after releasing the IOL haptics from capsule bag remnants, the IOL was fixed. The patient with IOL dislocation, with wide defects of the posterior capsule, anterior capsule fibrosis, planar synechiae and rhegmatogenous retinal detachment was performed reconstruction of the anterior segment of the eye, saparation of planar synechiae, removal of the fibrously changed lens capsule, IOL fixation, pars plana vitrectomy, retinal restoration, and vitreous tamponade using silicone oil. The patient with aphakia and rhegmatogenous retinal detachment was performed pars plana vitrectomy, retinal restoration, vitreous tamponade using silicone oil, IOL implantation with four-point fixation. Results No abnormalities were detected in the postoperative course of all patients. In the patient with preop hypertension, the intraocular pressure returned to normal. Best corrected visual acuity ranged from 0.3 to 0.9 at day 7 after surgery (Table 1). In all cases, the IOL was centrally located and parallel to the iris plane.
Here is a case of four-point IOL fixation for capsule support loss. A patient K., 74 y/o., presented with IOL subluxation in the right eye. Three years ago, the patient underwent cataract phacoemulcification of the right eye; an Adapt IOL (Bausch&Lomb) and a capsule tension ring were implanted. Examination findings: OD VA= 0.02; BCVA= 0.5 with sph +11.0 D. The anterior chamber is profound; there are vitreous fibrils in the anterior chamber. The pupil is round, freely mobile. Iridodonesis and pseudophakia are noted. The IOL together with the capsular tension ring is fixed in the capsule bag. The whole complex is displaced downwards and to the vitreous as far as only an edge of the capsule bag can be seen in the narrow pupil. Pars plana vitrectomy was performed, the capsule bag was removed, the capsular tension ring was explanted and the IOL was fixed to the sclera. After performing vitrectomy and removing the capsular bag, the IOL was repositioned to the anterior chamber. To protect the corneal endothelium, the anterior chamber of the eye was filled in with viscoelastic. The four-point fixation technique was used to secure the IOL to the sclera. At Day7 after surgery: Vis OD VA=0.7, uncorrected. The eye is quiet. The anterior chamber is of mean depth. The pupil is round, freely mobile. The IOL is centrally located, parallel to the iris plane. Vitreous loss is noted. The fundus examination showed no abnormalities. Discussion There are a number of IOLs designed for fixation in the absence of the lens capsule. Among them, there are models of mixed fixation in the pupil area and to the iris, which are famous in Ukraine and abroad (US-301 “GYMNAST” designed by M.M. Sergienko and US-304 “SPIDER” designed by L.A. Fedorov) [2, 4]. These models provide secure centration along the visual axis and fixation parallel to the iris plane. The implantation technique is relatively simple but requires a fairly large incision of the cornea. An iris-claw Artisan lens is a popular iris-fixated IOL [8, 9, 14, 15]. The implantation technique for this lens is a bit more difficult and also requires 6 mm incision. The Artisan lens is relatively expensive. Another variant is angle-fixated anterior-chamber IOL implantation [2, 6]. The lens implantation is simple but also requires a fairly large incision. There is an increased risk for corneal endothelial cell loss when implanting the anterior-chamber IOLs. There have been developed a lot of methods for fixation of classic IOLs. A technique of scleral IOL fixation is widely used [1, 5, 7, 12, 16]. The technique is rather complicated; it is difficult to achieve the IOL’s accurate centration and its fixation within the iris plane. Over the last years, a technique of intrascleral haptic-fixated IOL implantation has been often used [10, 12]. This fixation technique is also rather complicated but it enables to achieve a good centration and to avoid, in a certain degree, the lens’ tilting as to the iris plane. Some surgeons prefer iris-fixated IOL implantation [2, 3, 9, 14]. In this case, a suture needle must be advanced through the cornea. Our technique of four-point IOL fixation is relatively simple and does not require special equipment and tools. A similar technique, train track, has been proposed by Sung In Kim, Kiseok Kim for the IOL capture syndrome (2016) [13]. According to the technique proposed, sutures, after needle passing through the sclera, are placed in parallel to one another within the area between the iris and IOL. The sutures are to mark IOL off the iris and to prevent the development of planar synechiae between the iris and the capsular bag. In distinction from that surgery, our surgery was performed for IOL fixation in the absence of capsule support. Our study showed the absence of intraoperative and postoperative complications when performing the surgery using the proposed technique. When the needle is correctly advanced through the sclera to the marked points, IOL fixation within the iris plane is stiffly accurate. Moving the IOL on the pulled sutures enables to precisely position the IOL along the visual axis. Conclusions The technique developed for four-point IOL fixation in the absence of capsular support provides good centration along the visual axis and fixation within the iris plane. The fixation technique is comparatively simple and requires no special equipment. References 1.Akhremenko NV. [Intraocular correction of aphakia using a sparing method of transscleral faxation of posterior chamber intraocular lenses]. Oftalmol Zh. 2006;3:19-22. Russian. 2.Zhaboedov DG. Clinical studies of methods of intraocular lens implantation in the absence of the capsule support: author’s thesis for Cand Sc (Med): specialty 14.01.18, Ophthalmology. Kyiv; 2005. 21p. Ukrainian. 3.Pashtaev NP, Bat'kov EN, Zotov. [Iris suture fixation of posterior-chamber elastic intraocular lens in ligament apparatus laxity]. Vestn Oftalmol. 2010 Jan-Feb;126(1):47-50. Russian. 4.Sergienko NM, Zhaboiedov DG. A method of fixation of posterior-chamber intraocular lens. Oftslmol Zh. 2000;6:111-3. Russian. 5.Takhchidi KhP, Zubarev AB. Surgical Technique of Cataract Removal in Zonule Disorders. Oftalmokhirurgiia. 2004;4:16-8. Russian. 6.Apple DJ, Brems RN, Park RB, Norman DK, Hansen SO, Tetz MR et al. Anterior chamber lenses. Part I: Complications and pathology and a review of designs. J Cataract Refract Surg. 1987;13:157–74. 7.Das S, Nicholson M , Deshpande K, Kummelil MK, Nagappa S, Shetty BKJ . Scleral fixation of a foldable intraocular lens with polytetrafluoroethylene sutures through a Hoffman pocket. Cataract Refract Surg. 2016 Jul;42(7):955-60. 8.Guell JL, Velasco F, Malecaze F, Vazquez M, Gris O, Manero F. Secondary Artisan-Verysise aphakic lens implantation. J Cataract Refract Surg. 2005;31:2266–71. 9.Hirashima DE, Soriano ES, Meirelles RL, Alberti GN, Nos? W. Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome. Ophthalmology. 2010 Aug;117(8):1479-85. 10.Karadag R, Celik HU, Bayramlar H, Rapuano CJ. Sutureless Intrascleral Fixated Intraocular Lens Implantation. J Refract Surg. 2016 Aug 1;32(9):586-97. 11.Kjeka O, Bohnstedt J, Meberg K, Seland JH.. Implantation of scleral-fixated posterior chamber intraocular lenses in adults. Acta Ophthalmol. 2008;86:537–42. 12.Sinha R, Bansal M, Sharma N, Dada T, Tandon R, Titiyal JS. Transscleral Suture-Fixated Versus Intrascleral Haptic-Fixated Intraocular Lens: A Comparative Study. Eye Contact Lens. 2016 May 26. 13.Sung In Kim, Kiseok Kim. Tram-Track Suture Technique for Pupillary Capture of a Scleral Fixated Intraocular Lens Case Rep. Ophthalmol. 2016 May-Aug; 7(2): 290–295. 14.Zheng D, Wan P, Liang J, Song T, Liu Y. Comparison of clinical outcomes between iris-fixated anterior chamber intraocular lenses and scleral-fixated posterior chamber intraocular lenses in Marfan syndrome with lens subluxation. 2012 Apr;40(3):268-74. 15.Van der Meulen IJ, Gunning FP, Vermeulen MG, de Smet MD. Artisan lens implantation to correct aphakia after vitrectomy for retained nuclear lens fragments. J Cataract Refract Surg. 2004;30:2585–9. 16.Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol.2006;141:308–12.
|