J.ophthalmol.(Ukraine).2017;4:14-19.
|
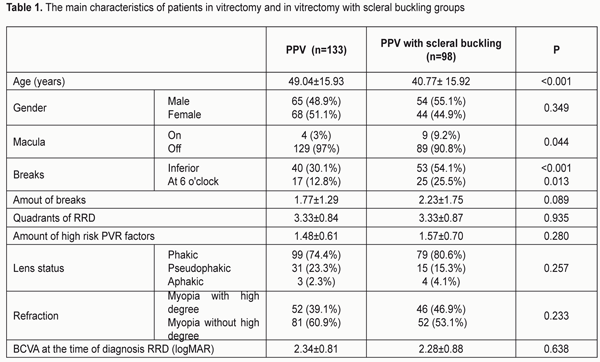
https://doi.org/10.31288/oftalmolzh201741419 Comparison study of results of vitrectomy and vitrectomy with scleral buckling for the treatment of patients with rhegmatogenous retinal detachment at high risk proliferative vitreoretinopathy L.A. Akhundova, M.I. Kerimov National Centre of Ophthalmology named after acad. Zarifa Aliyeva, 32/15 Javadkhan str., Baku, Azerbaijan, AZ1114 E-mail: lala.akhundova@yahoo.com The aim of our study was to analyze the effectiveness of vitrectomy and vitrectomy with scleral buckling in patients with a high risk of proliferative vitreoretinopathy. Material and Methods: Of the 367 patients (394 eyes) who applied in 2011-2014, in the National Center for Ophthalmology named after acad. Zarifa Aliyeva with diagnosis of primary rhegmatogenous retinal detachment (RRD) we selected 217 patients (231 eyes) with a high risk of proliferative vitreoretinopathy. The patients were considered to be of a high risk of proliferative vitreoretinopathy (PVR) development if they had RRD in three or more quadrants, more than one hour retinal breaks, pre-operative PRV, vitreous hemorrhage, aphakia/ pseudophakia, choroidal detachment. Vitrectomy and vitrectomy with scleral buckling were performed in 133 eyes (57.6% of cases) and 98 eyes (42.4% of cases), respectively. Results: The primary anatomical success of the surgery was noted in 71.4 and 70.4% of cases after vitrectomy and vitrectomy with scleral buckling, respectively, p=0.866. The final anatomical success was observed in 88.7 and 92.9%, after vitrectomy and vitrectomy with scleral buckling, respectively, p=0.290. In pseudophakia the primary anatomical effect was noted in 80.6 and 53.3% of cases after vitrectomy and vitrectomy with scleral buckling, respectively, p=0.054. In RRD associated with lowere breaks, the final anatomic success was observed in 85% and 96.2% of cases after vitrectomy and vitrectomy with scleral buckling, respectively, p=0.05. Conclusion: In rhegmatogenous retinal detachments in patients with a high risk of developing proliferative vitreoretinopathy, vitrectomy is more effective in pseudophakic patients and vitrectomy with scleral buckling is more effective in retinal detachments caused by inferior breaks. Key-words: Rhegmatogenous retinal detachment, pars plana vitrectomy, scleral buckling, proliferative vitreoretinopathy Rhegmatogenous retinal detachment (RRD) is one of the severest eye diseases which leads to complete or partial visual loss. Scleral buckling, pars plana vitrectomy and pneumatic retinopexy are considered the three most common surgical methods for treating patients with primary RRD [9]. Morphological characteristics of RRD, the lens status or the surgeon's preferences contribute to the choice of a surgical method [4]. One of the frequent reasons for the unsuccessful surgery for RRD is the occurrence of postoperative proliferative vitreoretinopathy (PVR) and the development of recurrent RRD. For example, some studies have identified characteristics of patients associated with the development of postoperative PVR, such as RRD in 3 or more quadrants, retinal breaks for more than 1 hour, preoperative PVR, vitreous hemorrhage, aphakia / pseudophakia, choroidal detachment [3,15,16]. Scleroplastic surgeries are often used in vitrectomy with complicated forms of RRD. However, the question of the effect on the primary anatomical success of the operation and development of PVR, an additional scleral buckling in vitrectomy is still open [1,2,6,7,8,9,12,13,17]. In recent years, there have been randomized controlled and retrospective studies that evaluated vitrectomy with or without scleral buckling in patients with RRD. However, most clinical studies have focused on RRD without a high risk of developing PVR, and prospective studies in complicated cases of RRD, such as a high risk of developing PVR, are lacking. The aim of our study was to analyze the effectiveness of vitrectomy and vitrectomy with scleral buckling in patients with a high risk of proliferative vitreoretinopathy. Materials and methods This study was prospective, randomized, controlled. Of the 367 patients (394 eyes) who applied with diagnosis of primary RRD in the National Center for Ophthalmology named after acad. Zarifa Aliyeva in 2011-2014, we selected 217 patients (231 eyes) with a high risk of proliferative vitreoretinopathy. Vitrectomy was performed in 133 eyes (57.6% of cases) and vitrectomy with scleral buckling was in 98 eyes (42.4% of cases). Patients with a minimal follow-up period of up to 3 months and with the age over 16 years were included in this study. At the time of the diagnosis of RRD, these 2 groups were not statistically different in terms of sex, visual acuity, number of breaks, quadrants of RRD, the number of risk factors for development of PVR, the status of the lens (Table 1).
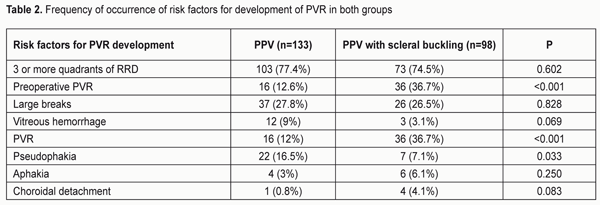
Risk factors for the development of PVR were observed as: 3 or more quadrants of RRD in 176 eyes, large breaks in 63 eyes, vitreous hemorrhage in 15 eyes, proliferative vitreoretinopathy in 52 eyes, pseudophakia in 29 eyes, aphakia in 10 eyes, choroidal detachment in 5 eyes (Tab.2.).
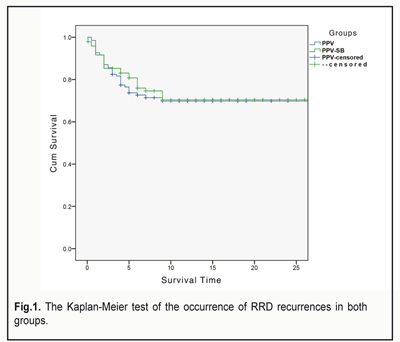
The prevalence of retinal detachment in most cases was 4 quadrants in the vitrectomy group (56.2%) and in the vitrectomy with scleral buckling group (58.2%). The difference was statistically insignificant, U=6.406, z=0.082, p=0.935, r=0.005. The primary tamponade was performed with gas in 38 eyes (28.6%) and in 5 eyes (5.1%), with silicone oil in 95 eyes (71.4%) and 93 eyes (94.9%), respectively, in vitrectomy and vitrectomy with scleral buckling, ?2=20.515, p<0.001. Silicone oil was removed after 5.1 ± 4.35 months (in the range, 1-36) and 6.28 ± 3.92 months (in the range of 0.5-21), respectively, in the vitrectomy and vitrectomy with scleral buckling groups, U=3.119, z=2.29, p=0.022, r=0.19. Surgical technique: The operation was performed under general or local anesthesia using a 23-gauge 3-port transconjunctival sutureless vitrectomy with or without an additional scleral buckling (# 240) using a non-contact, wide-angle viewing system with an image inverter (BIOM; Oculus, Germany). Accurus 800CS system with pneumatic vitreotome and xenon light source (Alcon Laboratories, Inc., Fort Worth, TX, USA) was used for all operations. Depending on the surgeon's preference, gases (C3F8-perfluoropropane and SF6-sulfur hexafluoride) and silicone oil (Alcon, DORC) were used as endotamponade. Statistical studies were performed with the IBM SPSS 20 (SPSS Inc., Chicago, IL, USA) software version. Shapiro-Wilk and Kolmogorov-Smirnov tests were used to study the normality of variables. The variables were not normally distributed, so the non-parametric Mann-Whitney U-test (Wilcoxon rank sum test) was used to compare quantitative variables. For the analysis of qualitative variables, a Chi-square test was used. In order to identify the risk factors for PVR development, we conducted a statistical analysis-binary logistic regression. Kaplan-Meyer test was used to determine the time of occurrence of recurrent RRD. In all cases, the value of p <0.05 was taken for statistical significance. Results The primary anatomical success of the surgery was noted in the vitrectomy group in 95 eyes (71.4%), and in the vitrectomy with scleral buckling group in 69 eyes (70.4%), ?2=0.029, p=0.866. The final anatomical success was observed in 118 eyes in the vitrectomy group (88.7%), and in 91 eyes in the second group (92.9%), ?2=1.120, p=0.290. Primary anatomical success among patients with high myopia was observed in 39 eyes in the vitrectomy group (75%), and in 34 eyes in the vitrectomy with scleral buckling group (73.9%). The final anatomical success among patients with high degree myopia was observed in 46 eyes in the vitrectomy group (88.5%), and in 42 eyes in the 2nd group (91.3%). In the phakic group, the primary anatomical success of the surgery was observed in 68 eyes (68.7%) and in 58 eyes (73.4%), respectively, in vitrectomy and vitrectomy with scleral buckling groups, ?2=0.476, p=0.490. In the pseudophakic group, in 25 eyes (80.6%) and in 8 eyes (53.3%), respectively, in vitrectomy and vitrectomy with scleral buckling, ?2=3.719, p=0.054. In the aphakic group in 2 eyes (66.7%) in the vitrectomy group and in 3 eyes (75%) in the vitrectomy with scleral buckling group, ?2=0.058, p=0.809. In the phakic group, the final anatomical success of the operation was observed in 85 eyes (85.9%) and 74 eyes (93.7%), respectively, in the vitrectomy and vitrectomy with scleral bcukling groups, ?2=2.812, p=0.094. In the pseudophakic group in 30 eyes (96.8%) and in 13 eyes (86.7%), respectively, in the vitrectomy and vitrectomy with scleral buckling group, ?2=1.194, p=0.193. In the aphakic group in 3 eyes (100%) in the vitrectomy group and in 4 eyes (100%) in the vitrectomy with scleral buckling group (statistically there are no differences). In RRD caused by inferior breaks, the primary anatomical success was observed in 29 eyes (72.5%) in the vitrectomy group and in 36 eyes (67.9%) in the vitrectomy with scleral buckling group, ?2=0.227, p=0.634. In RRD caused by inferior breaks, the final anatomical success was observed in 34 eyes (85%) in the vitrectomy group and in 51 eyes (96.2%) in the vitrectomy with scleral buckling group, ?2=3.654, p=0.05. Recurrent RRD in the vitrectomy group occurred in 38 eyes (28.6%) and in 29 eyes (29.6%) in the vitrectomy with scleral buckling group (p = 0.866). We conducted a Kaplan-Meier test (Fig. 1). The survival time, that is, the occurrence of recurrent RRD in both groups, does not differ statistically (?2=0.127, df =1, p=0.721, log rank test). Mean time of the occurrence of recurrent RRD in both groups is 10 months after the operation.
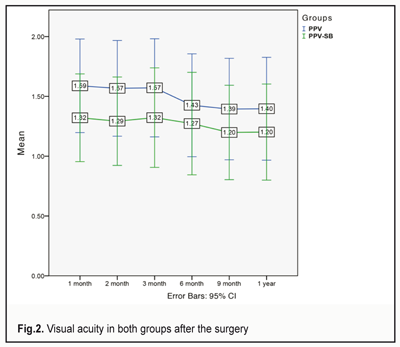
In a univariate analysis, the presence of preoperative PVR, vitreous hemorrhage and the prevalence of RRD are predictive factors in the development of postoperative PVR, which, however, have not been confirmed in a multivariate analysis, except for preoperative PVR. The remaining risk factors for the development of PVR in both the univariate and multivariate analyzes are statistically insignificant. In the presence of PVR before surgery, the risk of PVR in the postoperative period is 2.79-2.85 times higher than in the absence of PVR before surgery. In the vitrectomy group, 55.6% of patients, and in the vitrectomy with scleral buckling group 57.1% of patients had visual acuity <0.01 (LogMAR>2.0), ?2=2.087, p=0.555. BCVA in the vitrectomy group before surgery- 2.34 ± 0.81 LogMAR (in the range 0.3-3.0 LogMAR), and in the vitrectomy with scleral buckling group 2.28 ± 0.88 LogMAR (in the range 0.4-3.0 LogMAR), U=6.305, z=-0.470, p=0.638, r=-0.03. The final visual acuity in the vitrectomy group was 1.32 ± 0.80 LogMAR (in the range 0.3-3.0 LogMAR), in the vitrectomy with scleral buckling group 1.36 ± 0.79 LogMAR (in the range 0.4-3.0 LogMAR), U=6.750, z=0.469, p=0.639, r=0.031 (Fig. 2). In both groups, visual acuity was improved (p <0.001). In the vitrectomy group, 69 patients (52.7%), and in the vitrectomy with scleral buckling group, 53 patients (55.2%) will acquire the ability to read, ?2=0.143, p=0.705.
Discussion One of the reasons for the low success after vitreoretinal surgeries is considered to be a high risk of developing PVR in the postoperative period [15]. In previous studies, the risk of PVR was estimated as 3-12% for RRD without a high risk of developing PVR compared to our study, in which the risk of PVR was 22.6-25.5%, which confirms the accuracy of the selected category of patients for the study [11,17]. The question of the use of scleral buckling or vitrectomy for the treatment of RRD remains open [4,5,6]. However, once vitrectomy is selected as a method of surgery, the question of the use of an additional scleral buckling remains controversial [7,8,13,14,15,17]. Some authors argue that the use of additional scleral buckling improves the results of the operation, but others note that with careful vitrectomy in the vitreous base, the need for scleral buckling becomes unnecessary or even harmful. Pournas et al. compared vitrectomy and vitrectomy with scleral buckling in pseudophakic RRD and found no statistical difference between the two groups [10]. A retrospective study examining vitrectomy and vitrectomy with scleral buckling, with uncomplicated pseudophakic RRD, showed the same results of primary anatomical success between the two operations, but the final visual acuity was better in the vitrectomy group [17]. Kinori et al., in a retrospective comparison of vitrectomy and vitrectomy with scleral buckling, showed that the use of an additional scleral buckling in RRD does not change the results of the operation and slightly reduces the visual acuity than with only vitrectomy and in addition, does not affect the surgical outcome and is combined with an extended operation time and more frequent use of general anesthesia [7]. In one large retrospective study, 7,778 cases found that, in uncomplicated RRD, patients who had only vitrectomy had a higher anatomical surgical success than those with vitrectomy and scleral buckling, regardless of lens status [1]. However, in all the aforementioned retrospective studies of uncomplicated RRD, various risk factors for the development of PVR were excluded from the study, including patients with PVR of grade C, vitreous hemorrhage, large breaks, etc., which complicates comparison of our study with them. In another study in patients with risk of PVR, vitrectomy with scleral buckling is associated with a significantly higher rate of anatomical success compared to vitrectomy alone [15]. Lindsell et al. conducted a similar study and found no statistically significant difference between the groups in the primary anatomical outcome, the onset of PVR, and the final visual acuity [8]. In our study, a statistically significant difference was found in the pseudophakic group, in which improvement of the primary anatomical success of the surgery in the vitrectomy group (80.6%) was observed compared to the vitrectomy with scleral buckling group (53.3%), p=0.054. In the treatment of RRD without a high risk of developing PVR, the primary anatomical success of the surgery varies from 68% to 99% [2,14,17]. In a study by Storey et al., the primary success of surgery with a high risk of developing PVR was 63.1% [15]. In our study, the difference between the primary and final anatomical success is statistically insignificant and is 70.4% -71.4% for primary and 88.7% -92.9% for the final anatomical success of the surgery. In a retrospective survey, 512 patients who underwent vitrectomy with RRD Heimann et al. reported a high percentage of repeated detachments in patients with inferior RRD [6]. Therefore, some authors suggest the use of vitrectomy with scleral buckling in inferior RRD, although this issue still remains controversial [2]. However, according to Schneider et al., good anatomical success after vitrectomy with inferior breaks can be achieved without the use of scleral buckling and / or 360-degree laser retinopexy [12]. In our study, in RRD with inferior breaks, the final anatomical success was observed in 85% of cases in the vitrectomy group and in 96.2% of cases in vitrectomy with scleral buckling group, p=0.05. Conclusion In rhegmatogenous retinal detachments in patients with a high risk of the development of proliferative vitreoretinopathy, vitrectomy is more effective in pseudophakic patients and leads to improvement in the primary anatomical success of the surgery, and vitrectomy with scleral buckling is more effective in retinal detachments caused by inferior breaks and leads to improvement of the final anatomical success of the surgery. References:
|