J.ophthalmol.(Ukraine).2017;3:37-42.
|
https://doi.org/10.31288/oftalmolzh201733742 Retinal injuries secondary to consumer laser devices in children N.F. Bobrova, Dr Sc (Med), Prof. T.A. Sorochinskaya, Cand Sc (Med) L. A. Sukhodoeva, Cand Sc (Med) E.V. Ivanitskaya, Cand Sc (Med) N.I. Bakhmatskaya I.M. Levitsky Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine, Odessa, Ukraine E-mail: filatov_detskoe@mail.ru Background: In recent years, increased incidence of retinal injuries secondary to consumer laser devices (predominantly, pointers and those used at disco clubs) in children and adolescents have been observed. Purpose: To review the clinical features and structural retinal changes in the macula in pediatric patients following an injury secondary to laser ‘toys’. Materials and Methods: We retrospectively reviewed charts of 5 pediatric patients with retinal laser-induced burns (3 patients with fresh burns, and 2 patients who had a burn injury 1 year and 5 years before). Three patients, one patient and a 16-year-old girl (patient No. 5) received retinal burns from laser pointer, laser flashlight and at a disco club, respectively. On fundus examination, a blurred macular reflex, and 1 to 3 macular foci with pigmentation at the periphery of these foci were noted in three patients with 3 patients with fresh burns. In addition, in patient No. 5, an extensive round-shaped retinal hemorrhage was visualized, and the OCT demonstrated high optical density regions in the fovea under the inner limiting membrane, perifocal areas of thickened internal retinal layers the and loss of the retinal layer structure. In the patient who had a burn injury 5 years before, small foci of RPE atrophy similar to that of retinitis solaris were seen. Results: Patients with fresh burns received systemic and topical antitoxic, dehydration and antioxidant therapy. Laser posterior hyaloidotomy was performed in the patient with retinal hemorrhage. After treatment, in all patients, visual acuity improved substantially from 0.4 with myopic correction to 0.5-0.7. Conclusion: Although complete restoration of retinal foveal structure following pediatric injuries secondary to consumer laser products seems not possible, their timely comprehensive treatment enable high functional outcomes for these patients. Key words: retina, laser burns, children Introduction Recently, a new pediatric retinal pathology (posterior pole injury from the misuse of laser devices like pointers, flashlights, etc) has emerged [1-7]. This is due to the rapid advances in laser technology and wide use of the latter in domestic and entertainment applications; in addition, availability of laser devices at low cost made them popular. So called laser ‘toys’ like pointers, aiming devices, etc. are increasingly available over the Internet and in consumer electronic shops (Fig. 1). However, even in developed countries such ‘toys’ may not meet safety standards [8]. Laser-emitting devices are widely used at various entertainment events including those at youth clubs. This has resulted in increased incidence of maculopathy from consumer laser products in children and adolescents.
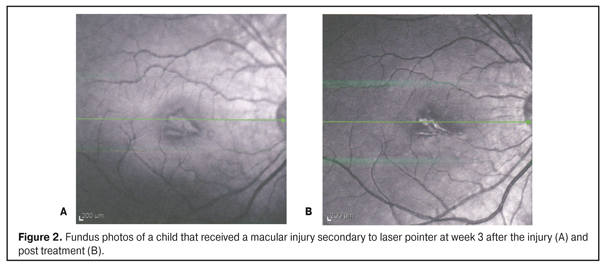
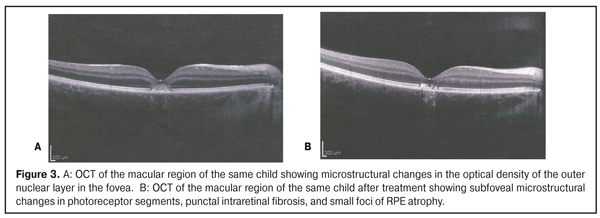
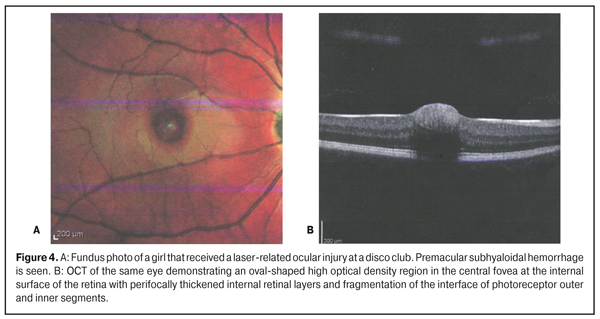
The purpose of the study was to review the clinical features and structural retinal changes in the macula in pediatric patients following burns secondary to laser “toys”. Materials and Methods We retrospectively reviewed the charts of 6 pediatric patients (four boys aged 9, 10, 11 and 15 years and 2 girls aged 7 and 16 years) with laser-induced retinal injury that received treatment at Pediatric Ophthalmology Department of the Institute between 2014 and 2016. Macular injury was unilateral in 4 children and bilateral in 2 children. Four children were admitted to in-patient care within 1-4 days following a burn injury, and 2 bilateral ocular burn patients were admitted 1 year and 5 years following a burn injury, respectively. Four patients and one patient reported to receive a retinal injury while playing with laser pointer and laser flashlight, respectively, and a 16-year girl reported to receive it at a disco club. All the cases were related to green laser. Each patient underwent a standard ophthalmological examination, including visual acuity, retinal biomicroscopy, monochromatic retinal ophthalmoscopy with fundus photography, and optical coherence tomography (OCT). In addition, 4 patients underwent retinal fluorescent angiography (FA). Each patient received treatment depending on the time following a burn injury and the severity of changes in the macula. Results Visual loss was a major complaint in all patients. In addition, the four patients with fresh burns complained of the development of a dark or red spot in front of the affected eye. At presentation, unaided visual acuity (VA) in the affected eye was 0.12 to 0.25 and 0.4 in 3 and 1, respectively, of the 4 patients with fresh burns. One of these four patients, a 16-year girl, developed a cherry-red spot in front of her right eye a week after attending a disco club. The unaided VA was 0.12 OD and 1.0 OS. In the two children who had suffered a bilateral injury, unaided VA at presentation was 0.1 OU (0.5 with myopic correction), and 0.12 OD and 1.0 OS, respectively. In both these patients, the cause of decreased vision was identified only after meticulous history taking and identification of characteristic changes in the fundus. Conjunctival congestion, photophobia, blepharospasm and tearing were observed clinically in the four children with fresh macular injuries. Biomicroscopy found normal anterior segment structures in all patients, optically clear media in 5 patients, and vitreous filaments in the 16-year girl who had sustained a unilateral retinal injury at a disco club. Fundus examination revealed retinal changes only in the macula in all pediatric patients. In three patients with fresh burns, it revealed a blurred macular reflex and 1 to 3 macular foci with marginal retinal edema and initial pigmentation at the periphery of these foci (Fig. 2A), and OCT findings included microstructural changes in photoreceptor outer segments and the outer nuclear layer in the fovea with a non-uniform increase in the optical density, and fragmentation of the retinal pigment epithelium (RPE) (Fig. 3A). An extensive round-shaped retinal hemorrhage was visualized in the 16-year girl who had sustained a unilateral retinal injury at a disco club (Fig. 4A). In this patient, the OCT demonstrated a high optical density region in the fovea under the inner limiting membrane, which was masking perifocal areas of diffusely thickened internal retinal layers. In addition, the OCT findings included loss of the retinal layer structure, microstructural subfoveal changes in photoreceptor outer and inner segments with a non-uniform increase in their optical density, and fragmentation of the interface of outer and inner segments (Fig. 4B).
In the 2 patients who had a burn injury 1 year and 5 years before, there was no macular edema, macular reflex was clear, but there were small parafoveal atrophic foci with pigment spots. In addition, the OCT findings included poorly identified photoreceptor segment structure in the central fovea and areas of low optical density with small foci of atrophy of adjacent RPE and decreased retinal thickness in the foveola; that is, the signs were similar to those of retinitis solaris. Furthermore, an absolute or relative central scotoma was seen. Patients with fresh burns received systemic and topical antitoxic, antihidtopic, anti-inflammatory, desensitizing and antioxidant therapy. A patient with preretinal hemorrhage underwent laser posterior hyaloidotomy for drainage of subhyaloidal hemorrhage into the vitreous, followed by hemostatic therapy. Two patients in the late phase after burn injury received retina stimulation and trophic therapy. Following treatment, VA improved from 0.45 with myopic correction to 0.7-0.85 (unaided) in patients with fresh burns, and from 0.1 with myopic correction to 1.0 with myopic correction in a boy in the late phase after burn injury. In addition, the hemorrhage resolved and visual acuity improved to 0.7 in the patient who underwent surgery. The macula of each patient developed atrophic round-shaped and linear and oval foci without signs of edema, and a decrease in pigmentation was observed (Fig. 2B). In two cases, fundus picture of the eye showed beaten metal appearance in the main focus. Small fresh foci partially resolved. OCT findings included subfoveal microstructural changes at the photoreceptor segment level, punctal intraretinal fibrosis, and small foci of RPE atrophy (Fig. 3B). The analysis of the changes over time in macular microstructure demonstrated that the thickness and optical density of the outer nuclear layer in the fovea restored to normal levels. Photoreceptor segment disruption, small foci of fibrosis and increased atrophy of small foci of RPE were noted. Discussion Laser rays are electromagnetic waves that propagate almost parallel to each other; they are highly directional, are scattered with a very small scattering angle, with a laser beam having a very intensive effect on the exposed surface area. Laser devices with the energy output exceeding 5 mW can pose danger to human health. The potential for injury depends largely on the laser’s wavelength. The human eye is approximately thirty times more sensitive to green light than it is to red light. Lasers are grouped into four classes (class 1 and 1М; class 2 and 2М; class 3A, 3B, and 3R and class 4) based on their power [9-11]. Class 1 laser systems (emitting radiation less than 0.4 mW) are considered to be incapable of producing damaging radiation levels during operation, and are widely used in ophthalmological equipment for aiming. Class 2 laser systems and Class 3A laser systems emit radiation less than 1.0 mW and from 1 mW to 5 mW, respectively, in the visible portion of the spectrum (0.4 to 0.7µm). Class 3B and 3R laser systems have an energy output of 5 mW to 500 mW, whereas Class 4 systems, in excess of 500 mW. Lasers can cause a variety of types of retinal injures, with the severity of the injury and penetration depending on the laser’s type, wavelength, spot size, and duration of exposure. Reports on cases of laser burns to the eye are scarce. Allen and colleagues [9] reported full thickness foveal hole in a man due to accidental exposure from a hand held Nd: YAG laser range finder device. Keunen and co-authors [12], Lim and colleagues [13], and Ozawa [14] also reported on cases of laser-related retinal injury to the macula. Thanos and colleagues [15], and Weng and co-authors [16] reported on cases of maculopathy induced by mirror-reflected light from a laser pointer. Shenoy and co-authors [17] reported on two cases with premacular subhyaloid hemorrhage and a case with a full thickness macular hole from laser pointer misuse. Yittrium aluminium garnet (YAG) laser hyaloidotomy was performed for the second case of premacular subhyaloid hemorrhage, but was unsuccessful. The reports on cases of pediatric laser pointer-induced maculopathy are scarce, possibly because this pathology has emerged relatively recently. Thus, Raoof and co-authors [8] reported on 5 cases of different forms of pediatric maculopathy secondary to exposure to high-power hand-held laser devices. Ocular pain, injection of the conjunctiva, and keratitis symptoms are regarded as symptoms of laser-induced ocular injuries, while metamorphopsia, chromatopsia, scotoma, and loss of vision may develop subsequently [1-7, 9-11]. The cornea and the crystalline lens absorb the major portion of the ultraviolet and infrared spectra as light passes through the ocular media. Although blink reflex, tear production and miosis provide some additional retinal protection, cases of retinal damage occur rather often [6, 11, 18]. Some authors have observed improvements in vision and OCT findings in the treatment of laser-related retinal injuries with systemic corticosteroids [2, 4, 5]; however, we believe that the use of this treatment approach should be discouraged in children, because it can have a range of negative consequences for the child’s body. In the early phase after burn injury, if premacular subhyaloid hemorrhage is present, YAG laser hyaloidotomy is performed, and followed by medical therapy [2]. The prognosis for restoration of vision depends on the following factors: duration of exposure to the laser, the amount of energy delivered by the laser, the time lag from retinal injury to treatment, the location of the lesion with respect to the fovea, extent of chorioretinal injury, and the presence, if any, and severity of subretinal and/or subchoroidal hemorrhages [17]. There is an agreement that in macular injury, the prognosis for restoration of vision is unfavorable [1-7, 9-11, 17]. Nevertheless, in all our pediatric patients, the treatment resulted in a substantial improvement in vision. Thus, the vision improved to the level of 0.5, 0.7 and 0.85, respectively, in three patients with fresh burns, to 1.0 with myopic correction in a patient in the late phase after burn injury, and to 0.7 in the girl who underwent posterior hyaloidotomy for preretinal hemorrhage. The OCT-based analysis of the changes over time in macular microstructure demonstrated that the thickness and optical density of the outer nuclear layer in the fovea restored to normal levels. Small fresh foci partially resolved. It is worth to note that these comparably high functional outcomes were achieved without the use of corticosteroids. Conclusion In a retinal injury secondary to consumer laser products, damage is located in the macula. In these cases, photoreceptor segments are the first to die. In addition, at the injured retinal regions, the RPE cells are subjected to damage, with a decrease in their number. Although complete restoration of retinal foveal structure following pediatric injuries secondary to consumer laser products seems not possible, their timely comprehensive treatment enable high functional outcomes for these patients without the use of corticosteroids. Numerous authors agree that children’s access to laser devices of any class should be limited, and that the need for increased recognition of the potential dangers of retinal injury caused by these devices should be emphasized. Children need to be alerted about the risk of unsupervised use of laser ‘toys’ like LED flashlights and laser pointers that pose a real threat to the pediatric eye. Moreover, adolescents need to be informed about the potential danger the so called disco club events pose to the eye. References
|