J.ophthalmol.(Ukraine).2017;3:30-36.
|
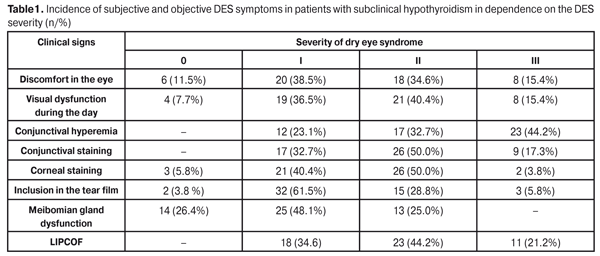
https://doi.org/10.31288/oftalmolzh201733036 Characteristics of dry eye syndrome in patients with subclinical and manifest hypothyroidism G.I. Drozhzhyna1 M.I. Pavlovskii2 1 Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine, Odessa, Ukraine 2 Lvov regional clinical hospital, Lvov, Ukraine E-mail: cornea@te.net.ua Background. The most common pathology of the thyroid gland is hypothyroidism. The decreased level of thyroid hormones in the body leads to development of hypothyroidism and is accompanied by metabolic, functional, and structural changes in different body organs and tissues including the eye. Thyroid gland disorders are known to be associated with the risk of development of dry eye syndrome (DES). However, the characteristics of the clinical course of DES in subclinical and manifest hypothyroidism remain almost unstudied. The purpose of the present paper was to reveal clinical characteristics of dry eye syndrome in patients with subclinical and manifest hypothyroidism. Material and Methods. A total of 87 patients (174 eyes) with primary hypothyroidism, aged 19 to 78 (М=50.5 SD12.5), were studied. The patients were diagnosed primary hypothyroidism by an endocrinologist and had dry eye syndrome. All the patients were recorded with Lvov Regional Clinical Diagnostic and Treatment Endocrinologic Center. Of them, there were 72 (82.8%) women and 15 (17.2%) men. Severity of DES was assessed according to DEWS classification (2007) that included patients’ self-assessment of severity and frequency of subjective symptoms. Tear film break up time (TFBUT), tear production (Schirmer I) test, biomicroscopy of the anterior eye, and fluoroscein staining were also performed. Results. The patients with subclinical hypothyroidism were more often revealed to have clinical symptoms and objective signs of DES corresponding to stage I and II of the syndrome while the symptoms and clinical signs corresponding to DES stage III were more common in manifest hypothyroidism. The most differences were noted in such signs as discomfort in the eye, conjunctival staining and the presence of inclusions in the tear film. A summed value of tear production was 9.4 (SD5.9) mm in subclinical hypothyroidism while that was significantly lower, in manifest hypothyroidism, 6.1 (SD5.4) mm, (р=0.0002). Stability of tear film was also lower in manifest than in subclinical hypothyroidism, 5.04 (SD2.0) and 5.84 (SD2.2) s, respectively, (р=0.0110). DES stage III was 5 significantly more often revealed in manifest hypothyroidism as compared to the subclinical type, 20 patients (54.1%) and 5 patients (10.0%), respectively, (?2 = 20, 22, р=0.00004). Conclusions. Tear production disorders are revealed both in subclinical and manifest hypothyroidism. In manifest hypothyroidism, the disorders are more apparent, which is evidenced by a decrease in tear production functional samples and a higher incidence of the severe stage of DES. In this regard, the hypothyroidism patients require ophthalmologist’s examination and follow up for an adequate tear substitute therapy to be prescribed and keratopathy development to be prevented. Key words: dry eye syndrome, hypothyroidism, subclinical and manifest hypothyroidism Background Thyroid diseases take the lead in the structure of endocrine pathology [1, 7, 9, 16]. The most common pathology of the thyroid gland is hypothyroidism. Hypothyroidism is a clinical syndrome caused by longstanding constant hunger of thyroid hormones in the body or their decreased action at the tissue level. Symptoms revealed at the early stage of the disease are extremely non-specific and can imitate various non-thyroidal illnesses [7, 8]. Thus, thyroid patients can come in sight of different discipline specialists including ophthalmology specialists. Thyroid hormone deficiency leads to metabolic imbalance and changes in activity of all body organs and systems including the eye. The literature has described different manifestations of hypothyroidism as open-angle glaucoma, keratoconus, dry eye syndrome, neurodegenerative changes in the retina and others [13, 18, 21, 23]. There are two forms of hypothyroidism: subclinical (latent) and clinical (manifest) ones. Subclinical hypothyroidism is characterized by an increased level of thyroid stimulating hormone (TSH) in the blood against the normal level of triiodothyronine (T3) and thyroxine (T4); clinical signs of hypothyroidism are absent as a rule. Manifest hypothyroidism is characterized by the increased TSH level against the decreased T3 and T4 level and the presence of typical clinical signs of hypothyroidism [3-8, 16]. Different authors have reported that the prevalence of manifest and subclinical hypothyroidism in population averages 2% and 1-17%, respectively, depending on gender and age. Hypothyroidism can be observed in any age; women suffer more often. Hypothyroidism prevalence can reach 12% and more in group of over-50-year-old women and 20% in women over 60 years old [7-9, 16]. Thyroid hormones (TH) are known to act through the interaction of triiodothyronine (T3) with nuclear receptors to it. It has been proved that receptors to thyroid hormones are present in acinus epithelial cell nucleus in the lacrimal gland, cornea and conjunctiva [11, 12]. Through these receptors, thyroid hormones regulate the structure and functions of cells and intracellular organelles, protein synthesis, cell proliferation, and lipid production, and are responsible for oxidative metabolism in these tissues [19, 23, 24]. The decreased level of thyroid hormones in the body leads to development of hypothyroidism and is accompanied by metabolic, functional, and structural changes in different body organs and tissues including the eye and, in particular, in the tear gland and ocular surface tissues, the conjunctiva and the cornea. Thyroid gland disorders are known to be associated with the risk of development of dry eye syndrome (DES) [2, 12, 17, 22]. Dias A. et al. have shown experimentally that the decrease in the level of thyroid hormones contributes to DES development [11]. Single papers have reported the data on DES incidence in patients suffering from hypothyroidism [18, 22]. Despite the prevalence of hypothyroidism, the literature data on changes in the ocular tissues are mainly related to decompensated and complicated forms of hypotheroidism while the characteristics of the clinical course of DES in subclinical and manifest hypothyroidism remain almost unstudied. The purpose of the present paper was to reveal clinical characteristics of dry eye syndrome in patients with subclinical and manifest hypothyroidism. Material and Methods A total of 87 patients (174 eyes) with primary hypothyroidism aged 19 to 78 (М=50.5 SD12.5) were studied. The patients were diagnosed primary hypothyroidism by an endocrinologist and had dry eye syndrome. All the patients were recorded with Lvov regional clinical diagnostic and treatment endocrinologic center. Of them, there were 72 (82.8%) women and 15 (17.2%) men. Hypothyroidism was caused by autoimmune thyroadenitis and postoperative hypothyroidism in 39 (44.3%) and 49 (55.7%), respectively. The duration of the disease did not differ significantly in both groups and was 6.6 (SD8.0) and 6.9 (SD7.6) years in patients with autoimmune and postoperative hypothyroidism, respectively, (р=0.9). The course of hypothyroidism was of a stable character in all patients. Of the patients, hypothyroidism was subclinical and manifest in 52 (59.8%) and 35 (40.2%) patients, respectively. Ophthalmic examination of the patients included external inspection, biomicroscopy of the anterior eye, fluorescein test, visual acuity test, tonometry, perimetry, and ocular fundus ophthalmoscopy. Severity of DES was assessed according to DEWS classification (2007) that included patient’s assessment of severity and frequency of subjective symptoms (ocular discomfort, feeling dryness, foreign body, burning sensation, "sandpaper" in the eyes) and disorders of visual functions during the day (changes in visual acuity, poor visual performance) as well as objective signs, assessed by an ophthalmologist, such as: conjunctival hyperemia, fluoroscein staining of the cornea and conjunctiva, the presence of characteristic changes of the tear fluid (inclusions in the tear film, mucus aggregates) and on the corneal surface (degenerative changes of the epithelium, punctuate keratopathy, filamentary keratitis), meibomian gland dysfunction. Quantitative indices were also assessed: tear film break up time (TFBUT) and tear production (Schirmer I test) were determined [10]. The quantitative indices were assessed on a four-point grading scale according to DEWS classification where: 0 score – the absence of a sign; 1 score – mild or episodic occurrence of the sign; 2 scores – moderate episodic or chronic occurrence of the sign under environmental stress; 3 scores – severe frequent or constant occurrence of the sign without stress; 4 scores – the presence of the severe disabling constant sign [10] . In biomicroscopy of the anterior eye, we performed a diagnostic test revealing the presence and intensity of lid parallel conjunctival folds (LIPCOF test) [14]. LIPCOF test was performed during slit lamp examination for temporal and nasal areas of the limbus on the bulbar conjunctiva above the rim of the lower eyelid using 18-27 magnification. LIPCOF were classified as follows: 0 – no folds; stage I – one fold which is smaller than tear meniscus; stage II – two folds which are smaller than tear meniscus; stage III – more than two folds which are larger than tear meniscus [14, 15]. Exclusion criteria were: the presence of Sj?gren's syndrome, rheumatoid arthritis, diabetes mellitus, surgical treatment of the eye, contact lens wear, and menopause-aged patients receiving a hormonal replacement therapy. Statistica 10.0 (StatSoft Inc., the USA) was used to perform statistical processing of the data. Results and Discussion As a result of the study, we determined the incidence and main clinical characteristics of dry eye syndrome in subclinical hypothyroidism, which are given in the Table 1.
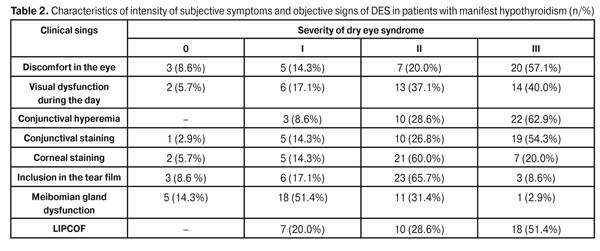
As it can be seen in Table 1, patients with subclinical hypothyroidism were more often revealed clinical symptoms and objective signs of DES corresponding to stage I and II of the syndrome. Thus, complaints of discomfort in the area of the eyeball and visual dysfunction during the day, which refer to DES stages I and II, were presented by 73.1 and 76.9 of patients, respectively. Conjuctival fluoroscein staining corresponding to DES stages I and II was noted in 82.7% and 90.4 %, respectively. Conjunctival hyperemia corresponding to stages I and II of DES was noted in 55.8% of patients and that corresponding to stage III was noted in 44.2% of patients with subclinical hypothyroidism. Inclusions in the tear film and conjunctival folds corresponding to DES stages I and II were observed in 90.3% and 78.8%, respectively. Meibomian gland dysfunction of stages I and II was revealed in 73.1 of patients. Clinical symptoms and objective signs of DES corresponding to DES stage III were less often revealed. In manifest hypothyroidism the symptoms and clinical signs corresponding to DES stage I were rarer while those corresponding to stage III were more often (Table 2). Thus, complaints of discomfort in the eyeball corresponding to stage I and stage III of DES were presented by 14.3% and 57.1% of patients, respectively. Complaints of visual dysfunction, corresponding to DES stage I, were in 17.1% of patients vs. 40.0% of patients with those corresponding to stage III. Conjunctival hyperemia corresponding to stage I and stage III was noted in 8.6% and in 62.9% of patients. Conjunctival staining corresponding to stage I and to stage III of DES was noted in 14.3% and 54.3%, respectively. LIPCOF corresponding to DES stage I were in 29.0% of patients vs. 51.4% of patients with stage III LIPCOF. Clinical signs of DES as corneal staining, inclusions in the tear film, and meibomian gland dysfunction in manifest hypothyroidism more often corresponded to stage II of DES: 60.0%, 65.7%, and 51.4% of cases, respectively.
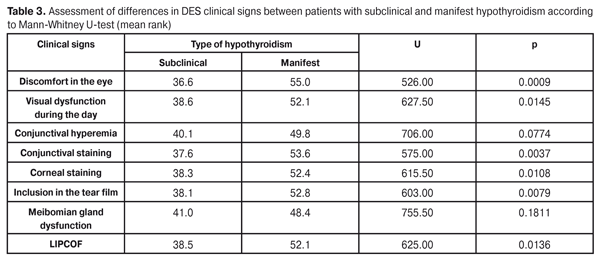
Studying the contingency between clinical hypothyroidism and DES clinical symptoms revealed the presence of significant relation by such signs as discomfort in the eyeball (?2=17.322, р=0.006), visual dysfunction during the day (?2=7.926, р=0.047), conjunctival staining (?2=15.497, р=0.091), conjunctival staining (?2=10.432, р=0.015), the presence of inclusions in the tear film (?2=17.000, р=0.001), and the presence of lower lid parallel conjunctival folds (LIPCOF test) (?2=8.659, р=0.013). No significant difference in such signs as conjunctival hyperemia (?2=4.071, р=0.1306) and meibomian gland dysfunction (?2=3.376, р=0.337) was revealed in subclinical and manifest hypothyroidism. Since DEWS assessment of DES severity includes variables reflecting subjective and objective signs which are presented as ordered categories showing the increase of sign intensity from 0 to 4, we used a Mann-Whitney rank test to assess the differences between two groups, with subclinical and manifest hypothyroidism. The results of this study are given in Table 3.
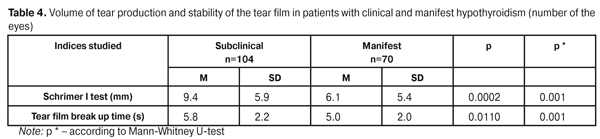
Data in Table 3 demonstrates that, of eight DES clinical signs studied, the indices of six ones (discomfort in the eye, visual dysfunction during the day, conjunctival and corneal staining, the presence of inclusion in the tear film, the presence of lower lid parallel conjunctival folds) were significantly different in patients with subclinical and manifest hypothyroidism. Herewith, the most differences in mean ranks of DES signs studied were noted in such signs as discomfort in the eye, conjunctival staining and the presence of inclusions in the tear film. Comparison of the quantitative indices that characterize the volume of tear production and tear film stability in patients with subclinical and manifest hypothyroidism showed that a summed value of tear production was 9.4 (SD5.9) mm in subclinical hypothyroidism while that was significantly lower, 6.1(SD5.4) mm, in manifest hypothyroidism (р=0.0002). Stability of the tear film was also lower in manifest than in subclinical hypothyroidism, 5.04(SD2.0) and 5.84(SD2.2) s, (р=0.0110), respectively (Table 4).
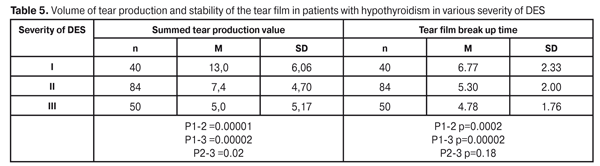
Taking into consideration a wide space of data, assessment of a difference level of the quantitative indices studied was also performed using the Mann-Whitney rank test. Difference evaluation inspection showed a statistical significance with high-level U=2185.00, р=0.00001 for Schirmer I test and U=2827.50, р=0.001 for TFBUT test. Since the patients with hypothyroidism had been revealed three stages of DES severity, we analyzed the values of the tear production indices (summed tear production and tear film stability) corresponding to each severity stage (Table 5).
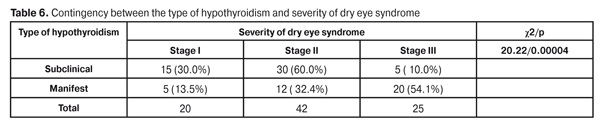
Studying the dependence between Schirmer I test values and DES severity stage, we determined that the summed value of tear production was significantly higher in DES stage I as compared to stage II and to stage III: 13.0 (SD 6,06) mm, 7.4 (SD 4.7) (р=0.00001), and 5.0 (SD 5.17) mm (р=0.0002), respectively. Statistically significant difference in Schirmer I test was also revealed between Stages II and III of DES severity (р=0.02). Stability of the tear film of stage I of DES severity equaled 6.77 (SD 2.33) s that was significantly higher as compared with stages II and III, where TFBUT was 5.3 (SD2.0) (р=0.0002) and 4.78 (SD1.76) s (р=0.0002), respectively. However, no significant differences were revealed in TFBUT between stages I and II of DES severity (p=0.18). The contingency between a type of hypothyroidism (subclinical and manifest) and DES severity intensity was studied (Table 6).
Data in Table 6 demonstrates that stage I of DES severity was diagnosed in 30.0% and in 13.5% of patients with, respectively, subclinical and manifest hypothyroidism. DES stage II was diagnosed in 30 patients (60.0%) and 12 patients (32.4%), with, respectively, subclinical and manifest hypothyroidism. DES stage III was 5 times more often revealed in manifest hypothyroidism as compared to subclinical type, 20 patients (54.1%) and 5 patients (10.0%), respectively. Thus, the contingency was determined between the type of hypothyroidism and DES severity: severe stage of DES was significantly more often observed in manifest hypothyroidism (?2 = 20. 22, р=0.00004). Tear production impairment determined in the patients with hypothyroidism can be caused by the influence of the chronically decreased level of thyroid hormones both on the tear fluid secretion and on inflammation of the ocular surface tissues which can result in tear film instability as well as in damage of the conjunctiva and cornea, which is evidenced by fluorescein staining of these tissues. It should be noted that this is common that an ophthalmologist is one of the first specialists that hypothyroidism patients apply to. That is why it is so important to know ocular manifestations of endocrine pathology. The presence of symptoms and clinical signs of DES can serve as an indicator of thyroid gland dysfunction and can allow the ophthalmologist to recommend determining the level of thyroid hormones in the blood and endocrinologist consultation in all cases where etiology of DES is unclear. Conclusions 1. The most significant differences in clinical signs of dry eye syndromes in patients with subclinical and manifest hypothyroidism are discomfort in the eyeball, conjunctival fluorescein staining and the presence of inclusions in the tear film. 2. Tear film stability and tear production volume is lower in manifest hypothyroidism as compared to subclinical hypothyroidism: 6.1 (SD 5.4) mm and 5.04 (SD 2.0) s; 9.4 (SD 5.9) mm and 5.84 (SD2.2) s, respectively.
3. Severe stage of dry eye syndrome was significantly more often observed in manifest hypothyroidism as compared to subclinical hypothyroidism: 54.1% and 10.0%, respectively. References
|