J.ophthalmol.(Ukraine).2017;3:20-29.
|
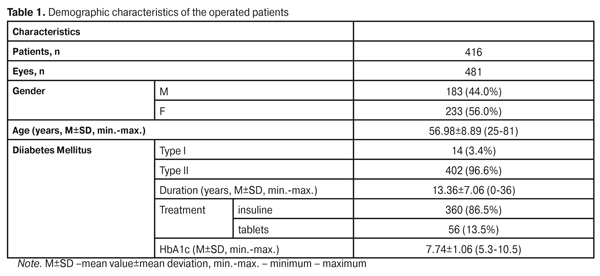
https://doi.org/10.31288/oftalmolzh201732029 Incidence, risk factors and results of treatment of rhegmatogenous retinal detachment after 23 gauge vitrectomy in proliferative diabetic retinopathy M. I. Kerimov E. M. Kasimov I. J. Aliyeva National Centre of Ophthalmology named after acad. Zarifa Aliyeva Baku, Azerbaijan E-mail: mushfikk@mail.ru Purpose. To study the incidence, risk factors, and results of treatment of retinal detachment developed after 23 gauge vitrectomy in patients with proliferative diabetic retinopathy. Material and Methods. A total of 416 patients (481 eyes) were operated on for the sequelae of proliferative diabetic retinopathy at Department of Ocular Complications of Diabetes Mellitus in National Centre of Ophthalmology named after acad. Zarifa Aliyeva within the period from July, 2009 to December, 2015. 23 gauge pars plana vitrectomy was performed in all patients using an Accurus 800 CS surgical system. The post-operative follow-up period of the patients after vitrectomy was 20.7±17.8 months with 1 month and 96 months as min and max, respectively. Results. With one surgery, complete retinal attachment was noted in 459/481 eyes (95.4%); 21/481 eyes (4.4%) had rhegmatogenous retinal detachment in the early post-operative period (within one month). In other four eyes, retinal detachment developed after silicone oil removal and, in other three eyes, in a remote post-operative period (within 3-24 months). There were a total of 28 cases of rhegmatogenous retinal detachment. Logistic regression analysis revealed that complete adhesion of the posterior hyloid membrane (more than two quadrants in the periphery), tractional-rhegmatogenous detachment and tractional detachment as vitrectomy indications, expressed bleeding during the membrane dissection, and the presence of intraoperative iatrogenic breaks increased the risk of postoperative retinal detachment development. Re-operations were performed in 24/28 eyes and anatomical success was achieved in 20/28 eyes (71.4% of all eyes with retinal detachment). Comparing to baseline, visual acuity increased in 13/28 eyes (46.4%), unchanged in 4/28 eyes (14.3%), and decreased in 11/28 eyes (39.3%). Conclusion. Rhegmatogenous retinal detachment developed after DR vitrectomy is still an extremely unfavorable complication and is characterized by quick development of ischemic and proliferative changes in the retina. Its timely detection and surgical intervention can partially preserve the visual functions in some cases. Key words: proliferative diabetic retinopathy, vitrectomy, rhegmatogenous retinal detachment, risk factors Background Diabetic retinopathy is a leading cause of blindness and visual impairment in working-age persons in the developed countries [9]. Despite the success of laser coagulation and inhibitors of vascular endothelial growth factor (VEGF) in conservative therapy for diabetic retinopathy, approximately 5% of patients with diabetes mellitus (DM) have complications developing in the course of a lifetime and requiring vitrectomy [4]. One of the rare but predictably unfavorable complications after vitrectomy in patients with proliferative diabetic retinopathy is rhegmatogenous retinal detachment (RRD). Although improvement of surgical technique and development of new tamponade agents have enabled to reduce the incidence of this severe complication, treatment outcomes can often be poor [2, 3]. In the literature, there are rare papers on analysis of risk factors and outcomes of treatment of retinal detachment after diabetic vitrectomy [5, 13, 14, 17]. The purpose of the present paper was to study the incidence, risk factors and results of treatment of retinal detachment developed after 23 gauge vitrectomy in patients with proliferative diabetic retinopathy. Material and Methods This was a retrospective study of clinical examination results of 416 patients (481 eyes) operated on for complications of proliferative diabetic retinopathy (PDR) at Department of Ocular Complications of Diabetes Mellitus in National Centre of Ophthalmology named after acad. Zarifa Aliyeva within the period from July, 2009 to December, 2015. Demographic data of the patients are given in Table 1.
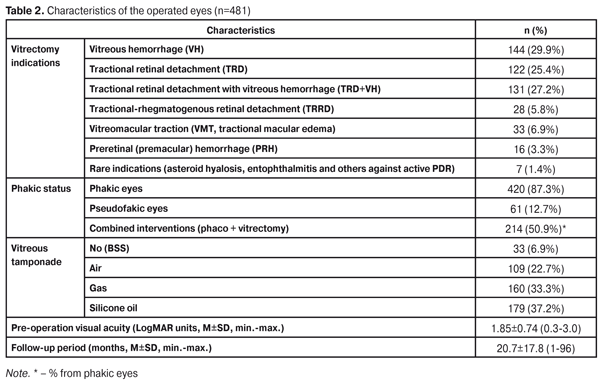
Vitrectomy indications and characteristics of surgical intervention are presented in Table 2. The main indications for vitreoretinal surgery were non-absorbable vitreous hemorrhage (144 eyes, 29.9%), tractional retinal detachment (122 eyes, 25.4%) and tractional retinal detachment with vitreous hemorrhage (131 eyes, 27.2%). Of the operated eyes, 420/481 (87.3%) eyes were phakic; of them, 214/420 eyes (51.2%) were performed phaco with IOL implantation and vitrectomy. The post-operative follow-up period of the patients after vitrectomy was 20.7±17.8 months with 1 month and 96 months as min and max, respectively.
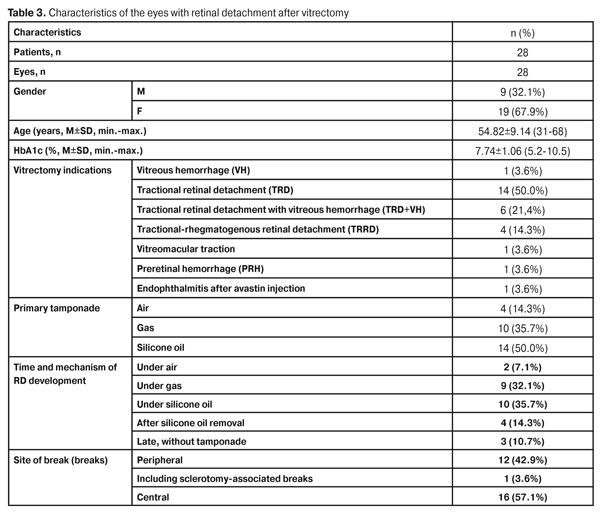
Surgical technique. Surgeries were performed using an Accurus 800 CS surgical system (Alcon, Forth Worth, Tex., the USA) under Zeiss Lumera Т and Zeiss Lumera 700 surgical microscopes (Carl Zeiss, Germany) with an integrated HD video recording camera. For posterior segment eye imaging, we used a wide-angle viewing system B?OM 4m (Oculus, Germany). The surgeries were performed under the local anesthesia with 2% lidocain. Disposable 23 gauge trocars were inserted into the eye at a 30° angle with conjunctival displacement. When carrying out the combined interventions, at first, phaco with IOL implantation in the capsular bag was performed and 10:0 nylon sutures were placed into the corneal insision to stabilize the anterior chamber when performing anterior vitrectomy. Vitrectomy started with core vitrectomy followed by staining and separation of the posterior hyloid membrane (PHM) using triamcinolone acetonide. Peripheral vitreal rhexis was first to release. Fibrovascular membranes in the posterior pole were separated and removed using a 23 gauge vitreous cutter, scissors were rarely used. If the inner limiting membrane (ILM) was to remove, we used brilliant blue G (BBG). The surgery was completed with vitreous tamponade using gas in 160 eyes (33.3%), air in 109 eyes (22.7%), balanced salt solution (BSS) in 33 eyes (6.9%), and silicone oil with viscosity of 1000 cst in 179 eyes (37.2%). The state of the posterior hyloid membrane was assessed according to B-scan data at baseline (pre-operation examination) and was determined later during the surgery. Since there is no commonly-accepted classification of PHM adhesion to the retina, we used our own working classification to analyze the role of PHM in RD development. According to this scale, we determined four degrees of PHM adhesion to the retina in PDR patients: 1, complete PHM or single adhesion; 2, flat adhesion (>1DD) limited by the anterior pole (periphery is free within 360°); 3, sectoral adhesion of PHM in periphery less than two quadrants in length (as a rule with nasal adhesion remained); 4, complete or almost complete PHM in periphery and in the posterior pole (more than two peripheral quadrants). Statistical analysis. The data obtained were processed using SPSS software (IBM SPSS Statistics, version 20.0). The quantitative variables were given as mean ± standard deviation (M±SD). To assess the impact, we used the univariate logistic regression analysis with detection of odds ration and 95% confidence interval. The value of p <0.05 was taken for statistical significance, which corresponds to standard criteria of medical investigations. If the value of p was less 0.001, it was pointed as p<0.001. Results In a total of 481 eyes with the PDR complications, 23 gauge pars plane vitrectomy resulted in primary anatomic success (complete retinal attachment after the first surgery) in 459 eyes (95.4%); in 21 eyes (4.4%), we noted retinal detachment, caused by a complete or partial rhegmatogenous componenet, in the early postoperative period (within 1 month after surgery). In four eyes, rhegmatogenous retinal detachment occurred later, after the silicone oil removal; three eyes without tamponade had rhegmatogenous retinal detachment occurred in late post-operative period from 3 to 24 months. Among the followed-up patients, there were 28 cases with post-operative retinal detachment with the rhegmatogenous componenet (5.8% of all operated eyes) (Table 3).
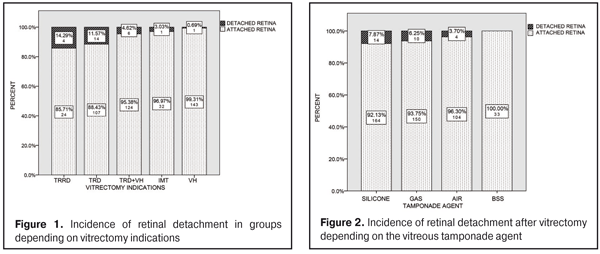
Besides, in one eye with tractional retinal detachment (TRD), the removal of membranes was not completed during the first vitrectomy due to poor functional prognosis, so the tractional detachment was not managed; in another eye, tractional detachment of the macula without a retinal break was observed after silicone oil removal. The latter two cases were excluded from the statistical analysis. In half the cases of post-operative detachment (14 eyes, 50.0%), TRD vitrectomy was performed. If we add the eyes with co-existing tractional detachment and vitreous hemorrhage (6 eyes, 21.4%) then a total of eyes with tractional detachment will be 20 (71.4% of all eyes with post-operative detachment). Tractional-rhegmatogenous retinal detachment (TRRD) was the indication for four eyes (14.3%). Only in one eye with post-operative retinal detachment, vitrectomy was performed due to non-absorbable vitreous hemorrhage (VH) (3.6%). The incidence of post-operative retinal detachment was different in groups in dependence on vitrectomy indications. As it can be seen in Fig. 1, a relative frequency of postop retinal detachment was of the highest level in TRRD group and equaled 14.9%; this index in eyes of TRD group and TRD+VH group was 11.57% and 4.62%, respectively. In other main groups, with vitreous hemorrhage and with vitreomacular traction (VMT), post-operative detachment was noted only in one eye in each group, i.e. 0.69% and 3.03%, respectively. As it can be seen in Table 3, retinal detachment after vitrectomy was more often observed in the eyes with primary silicone tamponade (14 eyes, 50.0%), that was rarer after gas (10 eyes, 35.7%) and air (4 eyes, 14.3%) tamponade. No retinal detachment in the post-operative period was noted in the eyes with balanced salt solution (BSS). Figure 2 demonstrates theincidence of retinal detachment in the post-operative period in groups with various tamponade agents. Retinal detachment with a partially rhegmatogenous component was observed in the post-operative period in 7.84 % of 178 eyes with primary silicone tamponade, in 6.25% of 160 eyes with gas tamponade, and in 3.70% of 108 eyes with air tamponade. Excluding the eyes with silicone tamponade, theincidence of detachment after vitrectomy comprised 4.7 % (14/301 eyes). Data on adhesion othe posterior hyaloid membrane (PHM) in the eyes with detachment in the post-operative period differed much from data of all operated eyes (Fig. 3). If complete PHM adhesion was noted only in a forth of the operated eyes (124/481 eyes, 23.8%), then it was observed more often in the eyes with retinal detachment in the post-operative period (17 eyes, 60.7%). Complete PHM detachment occurred in 11.4% of all eyes and only in one eye with retinal detachment (3.6%). In general, there was a clear tendency that PHM adhesion was of a higher degree of in group with retinal detachment in the post-operative period than in group of all operated eyes.
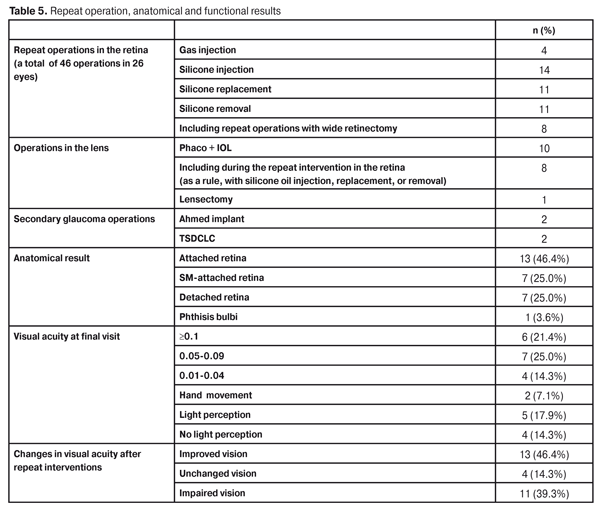
To determine the risk factors for development of rhegmatogenous retinal detachment in the post-operative period, we studied characteristics as follows: vitrectomy indications, phakia/pseudophakia, a state of adhesion of the posterior hyaloid membrane, the performance of preoperative panretinal laser coagulation, a preoperative antiangiogenesis injection (bevacizumab), preoperative visual acuity, intraoperative hemorrhage. For that purpose, we performed the univariate logistic regression analysis. Logistic regression analysis revealed some statistically significant factors for postoperative development of retinal detachment. It was revealed that complete PHM adhesion (more than two peripheral quadrants) 10 times enhanced the chance of retinal detachment after performing the surgery. Vitrectomy indications were also revealed to be significant for the risk of postoperative retinal detachment development. TRRD as a vitrectomy indication increases the risk of detachment 26 times and 21 times as compared with vitreous hemorrhage and tractional retinal detachment, respectively. Expressed hemorrhage during membrane dissection as well as the presence of iatrogenic breaks during the surgery was found to increase the risk of retinal detachment, 14 times and 16 times, respectively. The absence of full preoperative panretinal laser coagulation, preoperative intravitreal anti-VEGF injections, preserving the natural lens, which theoretically could obstruct the complete hyaloid membrane removal in periphery, poor preoperative vision appeared to be not significant risk factors for retinal detachment in the postoperative period. Results of re-perations. Repeat surgical interventions were performed only in 26 eyes (Table 5); 24 of them were due to retinal detachment. No effort to repair retinal detachment was made in four eyes since the functional prognosis was poor.
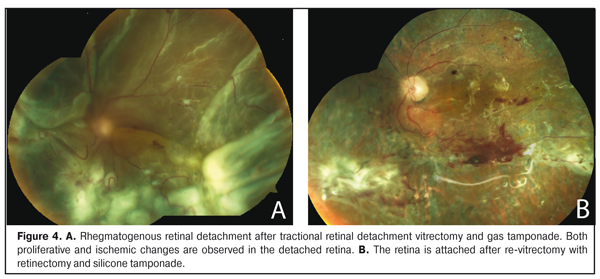
Anatomic success was achieved only in 20/28 eyes (71.4%): in 18/20 eyes after one surgery and in 2/20 eyes after two surgeries. Silicone tamponade was permanent in 7/28 eyes (25.0%). The retina was detached in 7 eyes at final visit, although three of them were re-operated. In one more eye, despite the repeat interventions, the process ended with phthisis bulbi. As it can be seen from Table 5, gas injection could help only in four eyes, the rest of eyes required silicone oil injection or replacement; moreover, eight eyes were performed expand (more that 180°) retinectomy. Phaco with IOL implantation was performed in ten eyes and only once after gas resorption; in the rest of cases, cataract surgery was a part of the combined interventions (together with introduction, replacement. and removal of silicone oil). As for severe postoperative complications, it should be noted that decompensated secondary glaucoma was present in four eyes (14.3%). Two eyes with preserved visual functions were performed Ahmed implantation; two eyes with vision loss were performed transscleral diode cyclo laser coagulation (TSDCLC). In general, comparing to baseline visual acuity before the primary intervention (vitrectomy), vision improved in 13 of the followed-up eyes (46.4%), unchanged in 4 eyes (14.3%), and decreased in 11 eyes (46.4%). The endpoint visual acuity was ?0.1 in six eyes (21.4%), 0.05-0.09 in seven eyes (25.0%), and 0.01-0.04 in four eyes (14.3%). Very poor vision, hand movement, was noted in two eyes (7.1%) and only light perception was in five eyes (17.9%). No light perception was in four eyes (14.3%). Figure 4 demonstrates an example of rhegmatogenous retinal detachment development in the eye with TRD and the eye condition after re-operation.
Discussion Rhegmatogenous retinal detachment (RRD) is a severe complication after vitrectomy in the PDR eyes and is characterized by quickly developing proliferative changes and extremely poor functional results after repeat interventions. Our purpose was to study clinical characteristics and results of treatment for retinal detachment which developed after vitrectomy for the sequelae of proliferative diabetic retinopathy and was caused, at least partially, by the rhegmatogenous component. To our best knowledge, only a few studies are devoted to studying RRD after diabetic vitrectomy. Brown et al. have analyzed the causes of re-operations in the 41 of 484 eyes (8.5%) after diabetic vitrectomy due to vitreous hemorrhage and tractional retinal detachment. Indications for re-operations were retinal detachment in 18 eyes (17 eyes had RRD, 3.5% of all eyes) and recurrent vitreous hemorrhage in 21 eyes. Only 4 of 18 reoperations for retinal detachment were a success [2]. Functional results of the operations were also poor: 10 of 18 eyes were with no light perception. Schrey et al. have observed RRD developed after vitrectomy only in four of 93 eyes (4.3%). However, in this series the vitrectomy indications were vitreous hemorrhages in 80 eyes (86.1%) and tractional retinal detachment in only 13 eyes (13.9%) [14]. A. Ruban has reported on RRD developed after vitrectomy in PDR patients in 1.5% of cases, and imcomplete attachment of the retina in a result of tractional retinal detachment in 8.4% of cases [12]. Helbig et al. have retrospectively reviewed results of vitrectomy performed in 389 eyes with diabetic retinopathy and retinal detachment have been observed in 18 % of cases (70 eyes). 29 eyes (7.5%) had retinal breaks; reproliferation in the retina caused detachment in 31 eyes. In 10 cases, the cause of the detachment was not identified because of the presence of vitreous hemorrhage. Herewith, the authors have noted an expressed relation between the incidence of retinal detachment and vitrectomy indications. The incidence of retinal detachment was 54 % after vitrectomy for tractional detachment of the macula, and only 5% after vitrectomy for vitreous hemorrhage [5]. Abunajma et al. have reported that, of 96 eyes with chronic TRD after vitrectomy, anatomical success was acheived in 87 eyes (90.6%), TRD remained in six eyes, RRD occurred in two eyes (it was successfully reoperated), TRRD was observed in one eye. In our study, RRD occurred in 5.8 % and and the retina was detached only in one eye of 144 eyes (0.7%), which had been operated on for VH; most eyes were with TRD and TRRD. It should be noted that in the literature, in most cases, RRD development after vitrectomy has been assessed in the eyes without silicone tamponade while the character of retinal detachment has not been specified in the eyes with silicone oil tamponade. However, in the clinical practice, both mechanisms, rhegmatogenous and tractional, play an important role in the development of retinal detachment after surgery. Castellarin et al. have reviewed 23 eyes operated on for PDR with silicone oil infusion: with one operation, the retina has been attached in 75% cases in the eyes with primary vitrectomy and in 73% in the eyes with re-vitrectomy. Of six eyes with retinal detachment remained, the retina was attached after additional surgery; however, the authors have not detailed the character of detachment after vitrectomy. In general, functional results of the surgeries performed have been shown to be poor. In the whole group, postoperative visual acuity improved only in 10 eyes (44%), decreased in 10 eyes (44%), and unchanged in three eyes (12%). In our study, in 12 eyes after vitrectomy, retinal detachment was caused by both traction and iatrogenic retinal breaks. As a rule, this was common for eyes with pre-operative presence of TRD, with completely attached PHM, active neovascularization and severe intraoperating bleeding. PHM adhesion increased the risk of iatrogenic breaks while expressed bleeding in membrane discission worsened fundus imaging and made it unpossble to completely remove the membranes. Thus, traction and breakes remained resulted in situation where the retinal detachment was enlarged and the rhegmatogenous component was added. The presence of the preretinal blood under silicone oil in the postop period stimulated reproliferation of the membranes and appearance and enlargement of the retinal breaks [18]. Logistic regression analysis showed that the statistically significant risk factors for retinal detachment development in the post-operative period were tractional and tractional-rhegmatogenous retinal detachment as a vitrectomy indication, complete PHM adhesion in the retina, iatrogenic breaks and severe intraoperative bleeding. Many authors have drawn their attention to the importance of the PHM state for successful PDR surgery [8, 15, 19]. Kamura et al. have studied the causes of iatrogenic break occurrence in diabetic retinopathy [15]. Patients were devided into three groups regarding the vitrectomy indications (VH, fibrovascular membrane without TRD, fibrovascular membrane with TRD). The authors noted the higher incidence of the iatrogenic breaks in the eyes with the fibrovascular membranes (FVM), the breaks were more often to form during membrane dissection. Retinal detachment in the postoperative period occured more often in group with TRD and FVM (8.2%), and significantly rarer in group with FVM without TRD (1.9%). Analysis of the risk factors has revealed that the iatrogenic breaks in membrane dissection 8 times increase the risk of retinal detachment (р<0.001). Our study also showed that a high degree of PHM adhesion in the ocular fundus periphery 10 times incrteased the risk of TRD development after surgery as compared to complete PHM detachment before surgery. Improved microsurgical techniques, in particular, microinvasive vitrectomy with a cannula system and a wide-angle imaging system, have significantly decreased the incidence of the iatrogenic breaks associated with sclerotomy [6, 10, 16, 17]. We identified the sclerotomy-associated retinal break only in one patient with TRD developed after surgery. In our group of patients, retinal detachment occurred after silicone oil removal in four of 93 eyes. In the literature, the incidence of re-detached retina after silicone oil removal in diabetic eyes is 12-15% [7, 11]. In our study, the incidence was significantly lower (4.3%); however, it should be noted that silicone oil was not removed for various reasons in 84 of 177 eyes with silicone tamponade. Repeat surgical interventions in the eyes with TRD after DR vitrectomy are highly sophisticated and are not always successful. In our study, re-operations for retinal detachment were performed only in 24 eyes and often required relaxing retinotomy and retinectomy, which made it possible to attach the retina in 20 eyes (7 cases with permanent silicone tamponade). Despite the anatomical attachment, final visual acuity ?0.05 was achieved only 13 eyes (46.4% of all eyes); in nine eyes, visual acuity at final visit was assessed as light perception or no light perception. Optic nerve atrophy associated with ischemic neuropathy was the most common cause of poor visual functions. Conclusion
Rhegmatogenous retinal detachment after DR vitrectomy is still an extremely unfavorable complication and is characterized by quick development of ischemic and proliferative changes in the retina. Its timely detection and surgical intervention can partially preserve the visual functions in some cases. Reference
|