J.ophthalmol.(Ukraine).2017;3:15-19.
|
https://doi.org/10.31288/oftalmolzh201731519 Effect of phosphocreatine on ocular hemodynamics and functional status of the macula in patients with dry age-related macular degeneration V.V. Savko Snr, Dr Sc (Med) V.V. Savko Jnr, Cand Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: valchuk2001@ukr.net Background. Age-related macular degeneration (AMD) comprises 12.5% and 22% in the structure of ocular incapacitation among persons of working and pension age, respectively. The important role in the pathogenesis of AMD belongs to ocular hemodynamics disorders. The lack of efficacy of a therapy for AMD determines the need to search for new drugs which would improve ocular hemodynamics in the disease. Purpose. To study the effect of phosphocreatine on ocular hemodynamics and the functional state of the macular area in patients with dry age-related macular degeneration. Material and Methods. Twenty-three patients (36 eyes) comprised Study group in which a complex therapy included phosphocreatine as a Neoton drug, in a dose of 1 g diluted in 50 ml of 0.9% sodium chloride, for 8 days. Twenty-five patients (39 eyes), comprising Control group, did not receive phosphocreatine in their treatment. Each patient was performed ultrasonic Doppler examination of the ophthalmic artery and a photostress test. Results. After treatment, the values of Doppler examination and photostress test were improved only in patients of Study group. Maximal and minimal blood flow velocity in the ophthalmic artery increased by 29% and 30%, respectively; vascular resistance index decreased by 14%; and photostress recovery time decreased by 33%. These indices did not change significantly in Control group patients. Conclusions. Inclusion of the phosphocreatine-containing drug in the complex therapy for the patients with dry AMD corrects ocular hemodynamics disorders, improves the functional state of the macular area and improves treatment outcomes. Key words: age-related macular degeneration, dry form, Doppler examination, ophthalmic artery, photostress test, phosphocreatine Introduction Age-related macular degeneration (AMD) is one of the most severe eye diseases, which is caused by its central localization, inconvertibility of dystrophic process progression and mainly bilateral damage to the retina [7, 21, 24, 28, 29]. In Ukraine, ocular incapacitation caused by AMD comprises 12.5 % among persons of working age and 22% among pension age persons [2]. AMD pathogenesis is complicated, many-sided and remains incompletely studied. Of AMD trigger mechanisms, the important part belongs to unbalance in free-radical oxidation and the anti-radical system state both in the retina and in the whole mechanism [16, 23, 29]. A decrease in blood oxygen-transporting, changes in rheological properties of the blood and tends to blood micro thrombosing as well as protein and lipid exchange and immune disorders are of essencial importance in AMD development [4, 10, 15, 26]. Many authors give the leading role in AMD pathogenesis to vascular disorders in the choroid and retina that develop against atherosclerosis. Hypercholesterinemia results in disturbances of energetic metabolism in capillary endothelium, which leads to cell destruction and, thus, to microcirculation disorders [5, 9, 19, 24]. Choriocapillary microcirculation disorders against impaired energetic metabolism have been proved to play a role not only in the development but also in the progression of AMD since choriocapillaries are the only source for blood supply in the macula, [11, 13, 27]. In turn, the microcirculation disorders in AMD can be caused by changes in regional hemodynamics secondary to the atherosclerotic disease of vessels, supplying the eye with the blood; this contributes to development of chronic ischemia and hypoxia in the retina and the further disease progression [1, 4, 17, 18]. Antioxidants, vasoactive, polypeptide, and immunotropic medications, vasoprotective, neotropic, and antisclerotic drugs, and systemic enzymotherapy drugs are used in treatment of dry AMD [7, 8, 14, 20, 22, 23, 28]. However, despite the wide range of pharmaceutical products, treatment of the disease appears ineffective, existing methods cannot provide the achievement of a stable medicinal effect and longstanding process stabilization [12, 21, 28, 29]. The lack of efficacy in the existing methods for AMD treatment as well as the presence of pathogenic dependence between the energetic metabolism disorders in vascular and retinal capillary endothelium and the following development of ischemia in these tissues have drawn our attention to phosphocreatine, being manufactured as a Neoton drug (registered NoUA/9671/01/01). Phosphocreatine plays a fundamental role in intracellular energetic processes and is used for resynthesis of an ATF energy source. The medication is not only a donor of high-energy compounds but also an activator of lactic dehydrogenase enzyme and succinate dehydrogenase enzymes which participate in cell energy supplying processes. A neuroprotective action of phosphocreatine is conditioned by preserving the cellular pool of adenine nucleotides, by inhibiting the degradation of phospholipids as well as by improving the microcirculation in the ischemic section [6]. Neoton is widely used in the complex therapy for acute myocardial infarction, acute and chronic cardiac failure, chronic ischemic cardiomyopathy, acute cerebral circulation disorders, and central nervous system ischemic damage. As for the phosphocreatine usage in ophthalmology, to our best knowledge, there is the only report on its using as a medication improving the reparation of corneal epithelium and endothelium in experimental contusion trauma of the eye [3]. The effect of phosphocreatine on ocular hemodynamics as well as on the functional state of the macula in AMD has not been studied. Purpose: to study the effect of phosphocreatine on ocular hemodynamics and the functional state of the macula in patients with dry age-related macular degeneration. Material and Methods Forty-eight patients (75 eyes) with dry AMD aged 49-64 y/o, of them 21 men and 27 women, were examined. 13 patients had a hypertensive disease; 19 patients had cerebral atherosclerosis; 11 patients had an ischemic heart disease. Concomitant eye conditions were: lens sclerosis (21 eyes), early cataract (27 eyes), hypertonic angiopathy (26 eyes), and marginal keratitis, “arcus senilis”, (6 eyes). In 31 patients (49 eyes), in the macula there were localized yellowish-white accumulations: both hard and soft drusens of different sizes, which were alternated with lipoid inclusions and sections of hypo- or hyperpigmentation of the retinal pigment epithelium. In 17 patients (26 eyes), dystrophic changes in the retina were more apparent and even spread from the macular area to the temporal branches of retinal central arteries and vein. The patients were divided into two groups: Study and Control groups comprised 26 patients (36 eyes) and 25 patients (39 eyes), respectively, comparable in gender (р=0.638), age (р=0.753), duration of the disease (р=0.528), visual acuity (р=0.752), and visual field (р=0.684). The patients of both groups were performed a therapy according to the protocol of medical aid delivery to patients with AMD: actovegin, 0.5 ml parabulbarly and 1.0 – 1.5 intramusculary for 10 days; pentoxifylline, 400 mg intake 3 times a day for 1 month; ocuvite complete, 1 tablet twice a day for 2-3 months. The patients in Study group were additionally administered phosphocreatine in a form of Neoton intravenous drip, in a dose of 1 g diluted in 50 ml of 0.9% sodium chloride, for 8 days. The patients tolerated the drug administration well; side effects were noted in none patient. Each patient was performed a visual field test, perimetry, biomicroscopy and ophthalmoscopy. The state of regional hemodynamics was studied using ultrasonic Doppler examination ("LOGIQ3 Expert", manufactured by "General Electric Co") with 4 MHz sensor frequency. In the ocular artery we detected blood flow indices as follows: Vmax – maximal velocity of the blood flow (cm/s); Vmin – minimal velocity of the blood flow at end diastole (cm/s); Ri – resistance index, reflecting the state of resistance to blood flow more distally from the measuring point. The functional state of the macula of the retina was assessed according to a photostress recovery test: time of visual field recovery after dosed bleaching of the retina [25]. Ocular hemodynamics and photostress testing was performed in 21 fellow eyes without focal retinal changes and served as controls. SPSS 10.0 software was used for statistical data processing. Quantitative indices were mathematically processed using Student t-criterion. Aanalysis of variance was performed using Mann–Whitney U test for independent samples). The level of significance (p) ? 0.05 was assumed. Results and Discussion The therapy performed resulted in an increase of visual acuity (VA) from 0.31±0.02 to 0.42±0.03 (р<0.001) in Study group patients while the VA increase in Control group was not significant, from 0.28±0.02 to 0.33±0.02 (р>0.05). The patients of both groups had the increase in the 8 meridian visual field index: from (432.4±5.2)° to (488.3±6.8)° (р<0.01) and from (424.8±7.3)° to (473.5±8.2)° (р<0.01), in Study and Control groups, respectively. The picture of the ocular fundus did not change much in the course of treatment in patients of both groups. Ultrasonic Doppler examination of the ophthalmic artery was carried out at baseline and after treatment in order to study ocular hemodynamics in patients of both groups. The data are given in Table 1.
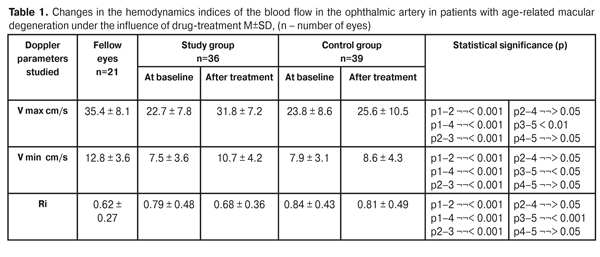
At baseline the Vмах indices were significantly decreased, in comparison with those of the fellow eyes, in both groups: from (35.4±1.8) cm/s to (22.7±1.3) cm/s (by 36%) and from (23.8±1.4) cm/s (by 33%) in Study and Control groups, respectively. The Vmin indices were also significantly decreased in both groups: from (12.8±0.8) cm/s to (7.9±0.5) cm/s (by 41% and 38%, respectively). Ri was significantly increased from (0.62±0.06) to (0.79±0.08) and to (0.84±0.07) (by 27% and 35%, respectively). At baseline, Doppler indices in both groups did not differ significantly from each other (р>0.05). On treatment completion, a significant difference in the hemodynamycs indices was noted only in Study group patients, in particular, Vмах and Vmin increased to (31.8±1.2) cm/s, (by 29%) and to (10.7±0.7) cm/s (by 30%), respectively; and Ri decreased to (0.68±0.06) (by 14%). In the patients of Control group, these indices did not change significantly. Table 2 demonstrates data on the photostress test indices in Study and Control groups at baseline and after treatment.
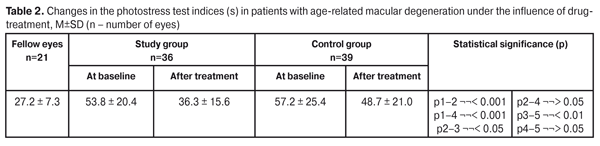
At baseline, the photostress indices of patients in Study and Control groups did not differ significantly from each other; however they were increased in comparison with the follow eyes by 98% and 110%, respectively, (27.2±1.8) s vs (53.8±3.4) s and (57.2±4.1) s, respectively. On treatment, the photostress indices significantly decreased only in Study group patients: to (36.3±2.6) or by 33%. This index did not change significantly in patients in Control group. Thus, the increased levels of systolic and diastolic velocity of the blood flow in the ophthalmic artery and the decreased vascular resistance give the evidence of improved blood circulation in the posterior pole of the eyes in patients with dry AMD after the complex therapy performed using the phosphocreatine-containing drug. This, in turn, is accompanied by the improvement of the functional state of the macula and is confirmed by the decreased photostress recovery time. Conclusions Inclusion of the phosphocreatine-containing drug in the complex therapy for patients with dry AMD has an apparent correcting action on the ocular hemodynamycs disorders in the posterior pole of the eye, which is evidenced by the increased systolic and diastolic velocity of the blood flow in the ophthalmic artery by 29% and 30%, respectively, and the decreased vascular resistance index by 14%. Using phosphocreatine in the complex therapy in dry AMD patients facilitates improving the functional state of the macula that is evidenced by the reduced photostress recovery time by 33%. Using phosphocreatine made it possible to improve treatment outcomes in patients with dry AMD that is evidenced by apparently increased visual acuity and expanded visual field. Reference
|