J.ophthalmol.(Ukraine).2017;3:3-8.
|
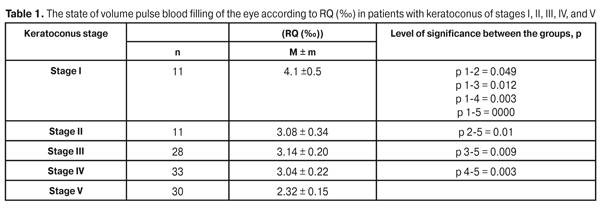
https://doi.org/10.31288/oftalmolzh2017338 Ocular hemodynamics in patients with stage I-IV keratoconus E.V. Ivanovskaia, Cand. Sc. (Med.) N.I. Khramenko, Cand. Sc. (Med.) G.I.Drozhzhyna, Dr. Sc. (Med.). Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: ivlen0502@mail.ru Background. Keratoconus is a progressive dystrophic condition of the cornea. Dystrophic changes in keratoconus are observed in the connective tissues of the sclera, drainage area, and iris. The role of a vascular factor in the development of such diseases as glaucoma, uveitis, and cataract is well-known. In this respect, studying the ocular blood supply in keratoconus appears to be reasonable. Material and Methods. Rheography was performed in 90 patients (125 eyes), aged 16-39, with keratoconus of stages I-V and the volume pulse blood flow in the eye was determined according to rheographic coefficient (RQ (‰)). In 21 eyes, stage IV-V keratoconus was accompanied by ocular hypertension and non-penetrating deep sclerotomy was performed. Depending on volume pulse blood flow rates and a vascular tone in the eye, 14 patients (28 eyes) with stage I-V keratoconus were treated using anti-ischemic and antioxidant drugs. Results. The decreased blood flow rates were noted in the eyes in each group as compared to norm. Volume blood flow was decreased by 26.7% in the eyes of the patients with stage II, III, and IV and by 44.8% in stage V keratoconus as compared to healthy patients of the same age. Volume blood flow RQ was 2.36±0.40 ‰ in stage IV-V keratoconus, complicated by ocular hypertension above 27 mmHg, i.e. by 43.8% lower than the age norm. Volume blood flow in the patients with stage IV keratoconus and intraocular hypertension was by 22.3% lower as compared with the uncomplicated course of stage IV keratoconus. Non-penetrating deep sclerotomy (NPDS) for ocular hypertension in the patients with stage IV-V keratoconus facilitated an increase in volume blood flow by 72.5%; RQ increased from 2.36±0.4 ‰ to 4.07±0.7 ‰), р <0.05. The vascular tone increased in large vessels in 41.6-82.3% of cases in all disease stages and in small vessels in 21.4-33.3% of cases in initial stages and in 50-71.4%% in III-V stages. The treatment resulted in significantly increased volume blood flow in the eye: RQ increased from initial 2.56±0.23 ‰ to 3.20±0.26 ‰, i.e by 25% (р = 0.006). Conclusions. 1. Volume pulse blood flow in the eyes of the keratoconus patients was significantly decreased as compared to the age norm: by 26.6% and by 44.7% in patients with keratoconus of stages II-IV and of stage V, respectively. 2. When keratoconus was complicated by intraocular hypertension, the decrease in volume pulse blood flow was more expressed: that was by 22.6 % lower in stage IV patients than in those with eutonia and by 44% lower than the age norm. 3. Surgery (NPDS) in patients with stage IV-V keratoconus, complicated by intraocular hypertension, facilitated the improvement of visual functions, normalization not only of intraocular pressure but also of ocular blood circulation, which was evidenced by the increase of volume pulse blood flow by 72.5%. 4. The comprehensive drug treatment including anti-ischemic and antioxidant medications resulted in improved ocular hemodynamics in volume pulse blood flow by 25%, stabilized visual functions and subjectively better visual performance. Key words: keratoconus, ocular hemodynamics, rheography Background Keratoconus is a progressive dystrophic, commonly- bilateral disease of the cornea which is characterized by changes in the structure of the central and, then, peripheral cornea that leads to its thinning and deformation, and to impaired visual acuity. Numerous research works have reported that possible fermentative defects in keratocytes, collagen disorders, changes of interstitial substance are responsible for strength properties of the cornea, in particular, keratoconus development, which leads to dehydratation abnormality in corneal tissues [21, 22, 25, 26]. Dystrophic changes in keratoconus and other genetically-caused corneal ectasias have been revealed not only in the cornea but in the connective tissue of the sclera [8, 12]. Biomicrogonioscopic investigations which we have performed in patients with progressive ectasias of the cornea (keratoconus, keratoglobus, pellucid marginal corneal degeneration) have shown that the absolute majority of the eyes (96.7%) are characterized not only by mesodermal tissue dysgenesis (remnants of Barkan's membrane in the anterior chamber angle) but also by atrophy, subatrophy of the iris, iris root and near-root [7]. In general, these data speak for dystrophic processes in the whole fibrous capsule of the eye. All structures of the anterior eye (sclera, iris, drainage system, ciliary body with the accommodative muscle, and lens) are characterized not only by a single topographic location but by common blood supply of this area. There is an idea that vascular changes in the eyeball follow anatomic ones, resulting in dystrophic changes and visual impairment. Thus, most researchers on glaucoma pathogenesis have marked a vascular factor among important factors of development and progression of primary open-angle glaucoma (POAG) [3, 4, 13, 17, 18]. Altered cerebral blood flow stands out in the pathogenic glaucomatous process [6]. Some papers [16, 23, 24] have noted the effect of an increased level of intraocular pressure on the state of microcirculation and its changes when intraocular tension is decreased. Research performed by Petrakovskii [18] has shown that, in myopia patients, inadequate blood supply in the anterior eye correlates with the character of sclera stretching: it’s more expressed in equatorial and mixed and less expressed in axial stretching. Blood supply deficiency in anterior eye segment (AES) gets worse as refraction strengthens. The role of vascular factor in development of such ocular conditions as uveitis [9, 18, 19], myopia [1, 9, 18], iridocyclitis [14], cataract [5, 18] is generally recognized. Ocular blood supply disturbances have been noted in age-related macular dystrophy [11], recurrent herpetic keratitis [20]. In numerous papers on general microcirculation in various conditions, attention has been directed to the presence of various types of microhemodynamics, which impact both the course of the treatment and the character of drug therapy [2, 10, 15]. In this regard, studying blood supply of the anterior segment of the eye in keratoconus appears to be reasonable. The purpose of the present paper was to study the characteristics of ocular hemodynamics in patients with keratoconus of various stages and to improve their treatment on the ground of this studying. Material and Methods A total of 90 patients (125 eyes) with keratoconus of stages I, II, II, IV, and V (according to classification by Puchkovskaia-Titarenko) aged 16 to 39 years were observed. The mean age was (28.6 +1.1) y/o. There were 66 men and 24 women. Keratoconus was of stage I in 17 eyes, stage II in 11 eyes, stage III in 28 eyes, stage IV in 33 eyes, and stage V in 30 eyes. Three patients had recurrent keratoconus after penetrating keratoplasty in both eyes. In twenty-one eyes, stage IV-V keratoconus was accompanied by ocular hypertension up to 27.0-30.0 mmHg and non-penetrating deep sclerectomy (NPDS) was performed. Surgical intervention efficacy endpoints were normalization of hydrodynamic parameters and stability of functional data. 14 patients (28 eyes) with stage I-IV keratoconus, who were prescribed treatment in dependence on the state of relative pulse blood circulation in the eye and a vascular tone, were followed up for 3 to 12 months. Comprehensive drug treatment included medications as follows: 1. Vincamine (a pharmacological class of vasodilators and microcirculation correctors): the medication decreases and stabilizes peripheral vascular resistance in the brain and has a unique property to normalize cerebral and ocular blood circulation. 2. Thiotriazoline (a pharmacological class of antihypoxic drugs and antioxidants): its pharmacological effect is determined by anti-ischemic, antioxidant, membrane-stabilizing, and immunomodulatory properties. 3. Metamax (a pharmacological class of Ib antiarrhythmic agents) has an anti-ischemic effect in vascular and dystrophic ophthalmic pathology. 4. Emoxypine (a pharmacological class of capillary-stabilizing (capillary-protective) drugs) has a pharmacological retina-protective effect. It protects the retina from the damaging action of highly intensive light, facilitates ocular hemorrhage resolution, decreases capillary permeability, reduces blood coagulability, and increases brain resistance to hypoxia and ischemia. Drug treatment efficacy endpoints were an increase of relative pulse blood circulation in the eye, according to rheographic coefficient RQ (‰), as well as an improvement of visual functions of the eye. Examination methods used were: visual acuity test, keratometry, refractometry, videokeratography, ultrasonic pachymetry, tonometry, and goniobiomicroscopy. Rheography was performed to all patients: volume pulse blood circulation in the eye according to rheographic coefficient RQ (‰) was determined. The normal range for volume pulse blood circulation in the eye at this age patients corresponds to RQ= (4.2±0.02) ‰. The indices of the state of the ocular blood vessel tone used are: ?1/Т–duration of anacrotic limb, referring to a shortwave differentiating curve, to duration of the whole rheographic pulse wave, characterizing the vascular tone in the eye; ?2/Т –duration of the second part of anacrotic limb, referring to a longwave differentiating curve that characterizes the tone of arterioles and capillaries according to ophthalmic rheogram. Statistical analysis was performed using Student criteria. Results and Discussion Stage I (initial) keratoconus (n=17) was characterized by mild optometric changes in the cornea with appearance of mild astigmatism with preserved visual functions and corneal thickness. RQ (‰) in this group patients was (4.1±0.5) ‰ that was within the normal range. In stage II keratoconus (n=11), a curvature of the cornea in the opposite meridians averaged (43.47 ± 0.58) and (43.45 ± 0.83) D with maximal and minimal values equal to 48.0 D and 38.75 D, respectively. The mean corneal thickness was (528.44±9.38) µm with a maximum of 583 µm and a minimum of 481 µm. Changed corneal parameters caused the impairment of uncorrected visual acuity at an average to (0.78±0.13) with max 1.0 and min 0.12, and of spectacle-corrected visual acuity to (0.93±0.05) with max 1.0 and min 0.6. Correction averaged (-1.5±0.28) D with -1.0 D and - 2.0 D as maximal and minimal values, respectively. IOP averaged (19.5±1.30) mmHg with max 22.5 and min 16.0 mmHg. RQ (‰) in patients of this group was (3.08 ±0.34) ‰. Stage III (developed) keratoconus (n=28) was characterized by more apparent optometric changes in the cornea. The curvature of the cornea in opposite meridians averaged (48.93±1.31) D and (49.89±1.01) D, with the minimal and maximal values of 58.0 D and 42.80 D, respectively. The mean corneal thickness reached (436.26±10.77) µm, with max 478 µm and min 412 µm. Changed corneal parameters caused the impairment of uncorrected visual acuity at an average to (0.18±0.04) with max 0.4 and min 0.03, and of spectacle-corrected visual acuity to (0.53±0.08) with max 0.85 and min 0.09. Correction ranged from -13.0 D to -2.5 D and averaged (-7.50±1.05) D. IOP in conversion to the corneal thickness averaged (22.44±1.66) mmHg with max 25.0 and min 20.0 mmHg. RQ (‰) in patients of this group was (3.14 ±0.20) ‰. Stage IV (expressed) keratoconus (n=33) was characterized by both optometric and clinical changes in the cornea including ectasia, thinning in the cone top, Vogt's lines, irregular astigmatism. The curvature of the cornea in the opposite meridians was (56.45±1.75) D and (55.05±2.03) with max 77.4 D and min 46.5 D. The mean corneal thickness equaled (347.83±22.27), µm with max 427.0 µm and min 179.0 µm. Uncorrected visual acuity was (0.08±0.01) with max 0.25 and min 0.12. Spectacle-corrected ranged from -16.0 D to -2.5 D and averaged (- 7.06±1.83) D. IOP in conversion to the corneal thickness averaged (25.66±3.27) mm Hg with max 30.0 and min 21.0. RQ(‰) in patients of this group equaled (3.04 ±0.22) ‰. Stage V (advanced) keratoconus (n=30) was characterized by apparent corneal ectasia with notable thinning in the cone point, blurring in subepithelial layers, and irregular astigmatism. The corneal curvature in the opposite meridians averaged (60.48±2.54) D and (61.52±3.14) D with max 81.3 D and min 49.45 D. The mean corneal thickness was (208.60±29.05) µm. Uncorrected visual acuity was (0.07±0.02) with max 0.2 and min 0.005; spectacle-corrected visual acuity was (0.17±0.05) within the range from -17.0 D to – 5.0 D. IOP in conversion to the corneal thickness averaged (23.44±2.35) mmHg with max 29.0 and min 23.0 mmHg. RQ (‰) in patients of this group equaled (2.32 ±0.15) ‰. Analysis of volume pulse blood circulation in the eye according to RQ (‰) showed that RQ (‰) in keratoconus of stages II, III, IV, and V was significantly lower than the age norm ranges (p<0.05) (Table 1).
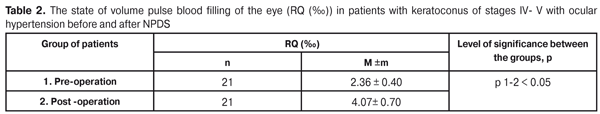
Non-penetrating deep sclerectomy (NPDS) was performed in twenty one cases of stage IV-V keratoconus complicated by ocular hypertension up to 27.0-30.0 mm Hg and anterior chamber angle closure with mesodermal tissue remnants. Pre-operative RQ (‰) in patients of this group equaled (2.36 ±1.53)‰. Visual acuity averaged (0.04 ±02). After NPDS surgery IOP normalization at an average to (17.50 ±1.45) mmHg and visual acuity improvement to (0.13± 0.06), p=0.001, were observed. RQ (‰) increased up to (4.07 ±0.70) ‰, p<0.05 (Table 2).
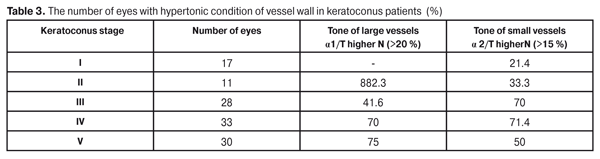
A percent reduction of blood circulation in the eye as compared to norm was determined in each group. Thus, volume blood circulation in the eye in patients with stage II, III, and IV keratoconus was decreased by 26.7%, and by 44.8% in patients with stage V keratoconus, compared with healthy patients of the same age. In patients with stage IV-V keratoconus complicated by ocular hypertension over 27 mmHg, volume pulse circulation in the eye was by 43.8% lower than the age norm, RQ= 2.36±0.40 ‰. Pulse blood circulation in patients with stage IV keratoconus and ocular hypertension was by 22.3% lower compared with uncomplicated course of the stage IV disease. Surgical intervention (NPDS) due to ocular hypertension in patients with stage IV-V keratoconus helped to increase volume blood circulation by 72.5%: RQ increased from 2.36±0.4 to 4.07±0.7‰, р<0.05. Three patients (6 eyes) had recurrent keratoconus, corneal ectasia with peripheral thinning, at 18-20 years after penetrating keratoplasty. Gonioscopy revealed that in the anterior chamber angle there were mesodermal tissue remnants covering the filtrating area that facilitated an IOP increase and corneal ectasia progression. RQ in patients of this group was (1.35 ±0.28)‰. The decrease of volume blood circulation in the eye in keratoconus patients was accompanied by the increased tone of both large and small vessels of the eye. Table 3 demonstrates that stage I-V keratoconus patients had the increase of the tone in large and small vessels by 20% and 15%, respectively, compared to norm.
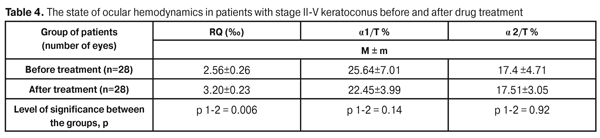
The data given in Table 3 show that the increased tone was observed in large vessels of the eye in 41.6-82.3 % of cases in all stages of the disease; and that in small vessels was in 21.4-33.3% of the cases in initial stages of the disease and in 50-71.7% in stage III-V of keratoconus. The data on blood circulation disorders in keratoconus (the decreased volume blood circulation, the increased tone of both large and small vessels of the eye, as compared to norm) made it possible to verify the possibility of vasoactive therapy to influence on ocular blood circulation disorders in keratoconus. We observed 14 patients (28 eyes) with keratoconus from initial to advanced stages for 3-12 months; the patients were treated in dependence on the rates of the relative pulse blood circulation in the eye and the vessel tone. Data on pre- and post-operation indices of the relative pulse blood circulation and the vessel tone in the eyes of keratoconus patients are given in Table 4.
The treatment performed resulted in a significant increase in the indices of pulse blood circulation of the eye: RG was increased by 25 % up to 3.20±0.26 ‰ vs. initial 2.56±0.23 ‰, (p =0.006). Subjectively, the patients noted the disappearance of eye stress and strain in visual workload, the improved tolerance of spectacle correction, improved overall health and better visual performance. Conclusions 1. Volume pulse blood circulation in the eye was significantly decreased after surgery: by 26.6% in patients with keratoconus of stages II, III, IV and by 44.7% in patients with stage V, as compared to the age norm. 2. When keratoconus was complicated by intraocular hypertension, the decrease in volume pulse blood circulation was more expressed: that was by 22.6 % lower in stage IV patients than in the those with eutonia and by 44% lower compared with the age norm. 3. Surgery (NPDS) in patients with stage IV-V keratoconus complicated by intraocular hypertension facilitated the improvement of visual functions, normalization not only of intraocular pressure but also of ocular blood circulation, which was evidenced by the increase of valume pulse blood circulation by 72.5%. 4. The comprehensive drug treatment including anti-ischemic and antioxidant medications resulted in the improvement of ocular hemodynamics in the index of volume pulse blood circulation by 25%, stabilization of visual functions and subjectively better visual performance. References
|