J.ophthalmol.(Ukraine).2017;2:38-43.
|
https://doi.org/10.31288/oftalmolzh201723843 Indications for inpatient treatment of cataract
M.I. Kovtun1, Cand Sc (Med) I.I. Lapkina2, Ass. Prof., Cand Sc (Med) M.L. Kochina2, Prof., Dr Sc (Biol) 1Hirshman Kharkiv Municipal Clinical Hospital No.14 2Kharkiv Medical Academy of Post-Graduate Education
Kharkiv, Ukraine E-mail: innalapkina@mail.ru
Purpose: To develop indications for inpatient cataract treatment based on the retrospective review of case histories of cataract patients. Materials and Methods: We retrospectively reviewed 636 case histories of cataract patients treated on an inpatient basis for at least two days. In addition, 20 experts working at Ukrainian tertiary care institutions responded to questions on potential causes of complications in cataract surgery, and their opinions were used to substantiate the indications for inpatient cataract treatment. Results: Hypertensive disease (HTD) and ischemic heart disease (IHD) were found in 34.6 ± 2.1% and 28.9 ± 2.0%, respectively, of the study patients. The presence of HTD and the presence of IHD in the cataract patient were associated with 1.8-times and 2.5-times, respectively, increased risk of postoperative complications when compared with patients without these comorbidities. The presence of glaucoma and the presence of mature cataract in the cataract patient were associated with 3.7-times and 1.8-times, respectively, increased risk of postoperative complications when compared with patients without these comorbidities. Inpatient treatment is in need in one-eyed cataract patients with very severe glaucoma and low vision or with mature cataracts, patients with bilateral mature cataracts, as well as cataract patients with lens subluxation, severe systemic disorders or mental disorders that prevent establishing productive contact with the patient. Key words: cataract, postoperative complications, systemic and ocular comorbidities Introduction Globally, cataract-related issues are the most common reason for visiting an ophthalmologist for elder and senile patients, which is largely attributable to the ageing of the world population. The number of cataract patients has substantially increased in recent decades, and is expected to rise even more in the nearest future. Surgery for cataract accounts for 60% of total surgical procedures performed at ophthalmology departments and clinics [1-3]. According to the WHO, by 2025, the global number of persons over 65 with lens opacity is expected to rise to 120 million, with as much as 40 million of them requiring surgical treatment. Recent studies have demonstrated that cataract has high prevalence both in developing and developed countries. Globally, more than 53 million persons have become unable to work because of a cataract-related disability, with 52 million of them living in developing countries. The prevalence of cataract in developed countries is also rather high. Nearly 20.5 million Americans age 40 and older have cataract, or 17.2% of that population. In particular, 42% of 52- to 64-year-olds Americans have this condition, increasing to 60% and to as much as 91% for those aged 65 to 74, and 75 to 85, respectively. Currently, there are more than 3 million surgical procedures for cataracts performed each year in the USA. In the UK, nearly 50% of the population aged 65 and older, and more than 70% of the population aged 85 and older, have some degree of cataract development. By the age of 65 and by the age of 85, 20% and 60%, respectively, of the French population develops some form of cataracts. In addition, in Australia, the incidence of cataract cases increases 2-fold for every decade of life after the age of 40, and 100% of the population aged 90 and older have some degree of lens opacity. Similar trends in the prevalence of cataract have been reported for other developed countries [4, 5]. Currently, the most common approach to cataract treatment involves phacoemulsification with IOL implantation. Recent technical and pharmacological advances in phacoemulsification have significantly contributed to reduced risk for developing peri- and post-operative complications in cataract surgery, which makes it possible to perform the procedure on an outpatient basis in most of cases. Ambulatory cataract surgery is the current standard of treatment for cataract in many countries. In Ukraine, ambulatory treatment of cataract is regulated by the Unified Clinical Protocol for Primary, Secondary (Specialized), and Tertiary (highly specialized) Medical Care [3]. Cataract treatment outcomes, however, depend not only on the equipment and technologies used, and on the surgeon’s skill and experience, but also on the number of factors contributing to the risk of complications. A decision for in-patient treatment should be made whenever a patient is in the high-risk group for postoperative complications. In addition to state and local public providers of ophthalmic care to cataract patients, there are private ophthalmic care providers (clinics and centers), with their number increasing year by year. Most of them have no inpatient beds, which limits their potential for providing care to high-risk patients. After initial examination, private clinics usually refer these patients to tertiary care institutions. If, in spite of risk-based pre-selection of patients, a postoperative complication does occur, the issue of inpatient treatment is resolved through personal contacts and interpersonal arrangements between doctors of state-run and private structures. This situation requires legal regulation and development of pertinent norms and guidelines, which would enable protection of patient rights and would improve quality of treatment. The purpose of the study was to develop indications for inpatient cataract treatment based on the retrospective review of case histories. Materials and Methods Out of 4543 case histories of cataract patients treated at the Hirchman Kharkiv City Clinic Hospital No 14 during the years 2014-2015, we selected and reviewed 636 case histories of patients treated on an inpatient basis for at least two days. In each specific case, the reason for inpatient treatment was identified. Case histories were reviewed for gender, age, cataract stage, reason for inpatient treatment and length of inpatient stay (postoperative complications, treatment of ocular comorbidity, and patient’s “will”), and type of complication. In order to develop indications for inpatient cataract treatment, we used individual opinions of 20 experts working at Ukrainian tertiary care institutions. Each of these experts noted the conditions he/she believes may cause peri- and/or post-operative complications based on his/her personal expertise in the field of cataract surgery. The results of expert opinions are presented in Fig. 1.
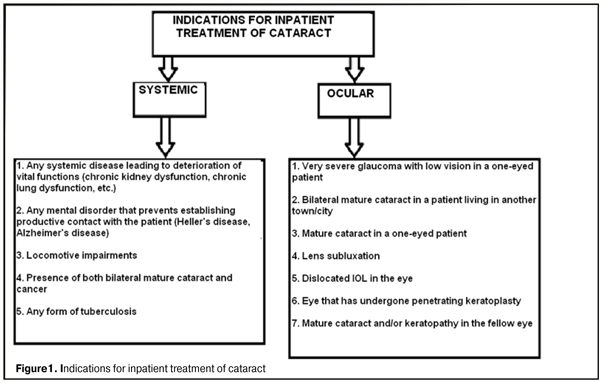
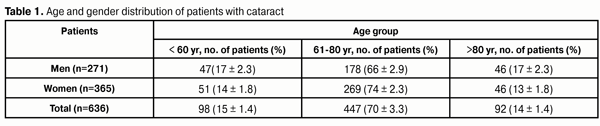
The case history data were analyzed using descriptive statistics, Pearson’s chi-square tests and split-half analysis [6]. Contingency tables were used to calculate odds ratios. Results and Discussion The indications for inpatient cataract treatment (Fig. 1) were conventionally divided into two groups: systemic and ocular indications. Systemic indications for inpatient cataract treatment included severe systemic disorders as well as mental disorders that prevent establishing productive contact with the patient. Patients with these disorders need special care and should be supervised by specialists during pre- and post-surgery periods, which can be ensured only in the special in-patient department setting. Private clinics usually deny surgical treatment to such patients and refer them to state-run or community medical institutions for inpatient care. Ocular indications for inpatient cataract treatment included a severe concomitant eye condition, cataract in one-eyed patient, and any eye condition requiring a more complex surgery. Patients with above ocular conditions represent a substantial commercial risk to a private clinic, and are also referred to special state-run or community medical institutions for inpatient care. Outpatient cataract surgery is not performed in most of patients with conditions presented in Fig.1, and such patients receive inpatient treatment for different periods of time. Previously, we have analyzed gender differences in the time from diagnosis of cataract to surgery [7, 8], prevalent post-surgical complications [9], and prevalent ocular and systemic comorbidities [10, 11]. A similar analysis was performed in the study reported here in 636 case histories of patients treated on an inpatient basis for at least two days. Table 1 shows the age and gender distribution of patients. Patients were conventionally divided into three age groups (Group 1, working-age patients (defined as < 60 yr); Group 2, retired patients, 60 yr ? age < 80 yr; Group 4, retired patients, ?80 yr). Group 2 was the most numerous, whereas the two others were almost equal in size.
Peri- and post-operative complications were identified in 52 (8.2±1.1%) out of 636 patients (Table 2). Corneal edema and iridocyclitis were the most common post-operative complications (p<0.01). These complications usually are an ocular response to surgical trauma. The rate of complications identified was similar to those reported in the literature [4, 5, 12-14].
The following factors may contribute to the risk of developing corneal edema after cataract surgery: prolonged manipulation in the anterior chamber during aspiration-irrigation; prolonged manipulation in the anterior chamber at surgery, resulting in endothelial damage; low number of endothelial cells in the cornea; and a dense nucleus requiring much greater ultrasound power than do soft nuclei, with increased risk of traumatic damage to the corneal endothelium. Corneal edema was identified in 23 (3.6±0.7%) out of 636 patients. The common causes or postoperative iridocyclitis are (a) lens matter left at the periphery of the capsular bag, (b) reactive edema resulting from IOL contact with ocular structures (the ciliary body and/or iris), especially in transscleral IOL fixation; and (c) edema of the Schlemm’s canal and trabecular meshwork zone in anterior chamber IOL implantation. In addition, postoperative iridocyclitis can be caused by individual immunologic differences. Ciliochoroidal detachment was the third most common post-operative complication and was identified in 8 (1.3±0.4%) out of 636 patients. All cataract patients with glaucoma patients underwent complex ocular procedures (cataract extraction and IOL implantation combined with glaucoma surgeries). The most common systemic comorbidity was hypertensive disease (HTD), followed by ischemic heart disease (IHD) (34.6±2.1% and 28.9±2.0%, respectively) (Table 3). These diseases contribute to ocular and systemic metabolic abnormalities, with the potential for developing postoperative complications. Therefore, patients with these diseases are at some risk for developing postoperative complications. Postoperative complications were significantly higher in cataract patients with IHD, and this comorbidity was associated with a 2.5-times increased risk of postoperative complications (?2=10.7; OR=2.5; p<0.05). A similar significant association was found between the presence of HTD in cataract patients and postoperative complications (?2=4.4; OR=1.8; p<0.05). Women had higher rates of all comorbidities examined except for glaucoma (Table 3). Gender differences in rates of different comorbidities were analyzed using split-half analysis. We have reported recently that cataract patients with diabetes mellitus (DM) are at a rather high risk of developing an exudative inflammatory response as a postoperative complication [10]. In the study reported here, this comorbidity was found in 79 patients (12.8±1.5%), with almost no gender difference in the rate of exudative inflammatory response. The presence of diabetes mellitus in a cataract patient should be taken into consideration preoperatively, since these patients are characterized by increased local inflammatory activity and immune response which can result in postoperative inflammatory complications. Arthritis and podagra (joint disorders associated with systemic abnormalities) were another common comorbidity (6.7±1.1 %). The presence of this pathology can also cause postoperative inflammatory complications in the form of inflammatory response [10]. Although no statistically significant influence of DM or joint disorders on postoperative complications of cataract surgery was identified in our study, it has been reported previously that these disorders can contribute to postoperative complications, and this should be taken into consideration when making a choice between inpatient and outpatient cataract treatment. According to the literature, highly myopic patients with cataract are at high risk for perioperative complications, which is believed to be associated with the features of cataract development in their eyes. These features include dense nuclei, subcapsular opacities with intimate adhesion to the posterior capsule, and zonular laxity. The complication rate in cataract surgery in highly myopic eyes is 1.5-2 times higher than that in eyes with senile cataract [10]. Our statistical analysis did not reveal any significant association between the presence of high myopia and incidence of postoperative complications. Further studies of larger patient cohorts might demonstrate the relationship between high myopia and success of cataract surgery. Glaucoma and cataract are the leading causes of blindness and visual impairment, and have been found to occur concomitantly in 17–38.6% of cataract cases [15]. Takhchidi et al [16] believe that the following are the most common early postoperative complications of cataract surgery in the presence of POAG: corneal edema, inflammatory response, fibrin in the anterior chamber, hypotony, and hyphema. In the study reported here, preoperatively, glaucoma was present in 53 cataract patients (7.8±1.2%). We performed a more detailed analysis of all cases of concomitant cataract and glaucoma, with an emphasis on gender differences. Both disorders were present in 33 male patients (12.1±2.1%; median age, 75±8.7 years; range, 53 years to 88 years; inpatient stay, 6.3±3.1 days; number of cases with inpatient stay of ? 6 days, 22) and 20 female patients (5.5±1.4%; median age, 73±8.2 years; range, 54 years to 91 years; inpatient stay, 6.0±2.4 days; number of cases with inpatient stay of ? 6 days, 6). Chi-square analysis found significant influence of concomitant glaucoma on the development of postoperative complications, and this comorbidity was associated with a 3.72-times increased risk of postoperative complications (?2=13.9; OR=3.72; p<0.05). It should be noted that, among cataract patients with concomitant glaucoma, no statistically significant gender differences with regard to age or inpatient stay were detected. Long inpatient stays (i.e., those of ? 6 days) were for the following reasons: postoperative complications, additional treatment required for vascular disorders, and the patient’s will to remain in hospital under observation. Postoperative complications are usually more common in eyes with mature cataract, which is associated with the need for long ultrasound time in phacoemulsification compared to early or immature cataract. By the time of surgery, out of 639 cataract cases, the numbers of patients with mature, immature and early cataract were 192 (30±1.8%; 75 male (12±1.3%) and 117 female (18±1.5%)), 328 (52±2.0%; 141 male (23±1.6%) and 187 female (29±1.8%)), and 116 (18±1.5%; 56 male (8±1.1%) and 60 female (10±1.2%)), respectively. Mature cataract was found statistically significantly more often in women than men (?2=4.6; p<0.05); the same was true for immature cataract (?2=12.9; p<0.05). Complications were detected statistically significantly more often in mature cataract than in immature and early cataract (?2 = 3.95; OR =1.8; p < 0.05). The mean inpatient stay was longer in women than in men (5.4 ± 2.8 days vs 4.8 ± 2.7 days). The mean age was 70.1± 10.4 years for men and 73.0 ± 8.8 years for women. Among men and women, there were 9 (12%) and 9 (8%), respectively, patients younger than 60 years. Postoperative corneal edema was the most common complication identified in the study. Conclusions First, systemic indications for inpatient cataract treatment included severe systemic disorders and mental disorders that prevent establishing productive contact with the patient. One-eyed patients with very severe glaucoma and low vision, patients with bilateral mature cataracts, one-eyed patients with mature cataracts, and patients with lens subluxation need inpatient treatment of cataract. Second, the most common systemic comorbidity was hypertensive disease (HTD), followed by ischemic heart disease (IHD) (34.6±2.1% and 28.9±2.0%, respectively); the presence of either of them might be a risk factor for developing postoperative complications. The presence of HTD and the presence of IHD in the cataract patient were associated with 1.8-times and 2.5-times, respectively, increased risk of postoperative complications when compared with patients without these comorbidities. Third, among cataract patients with concomitant glaucoma, no statistically significant gender differences with regard to age or inpatient stay were detected, and mean inpatient stay was 6 days or more. The presence of glaucoma in the cataract patient was associated with a 3.7-times increased risk of postoperative complications when compared with patients without this comorbidity. Finally, the presence of mature cataract was associated with a 1.8-times increased risk of postoperative complications when compared with patients with immature or early cataract.
References 1. [Adapted Evidence-Based Guidelines: Cataract. 2015]. 2. Rykov SO, editor. [Organization of ophthalmological care at the present time]. Kyiv: Doktor Media; 2008 Ukrainian 3. [Unified Clinical Protocol for Primary, Secondary (Specialized), and Tertiary (highly specialized) Medical Care: Cataract. Decree No.49 issued by Ukraine’s Ministry of Health dated 28 January 2016]. 4. Chitkara DK, Hall AB, Rosenthal AR. Pathophysiology and Epidemiology of Cataract. In: Yanoff M, Duker JS, Augsburger JJ et al. editors. Opthalmology, 2nd ed. Philadelphia, PA: Mosby; 2004. p.275-9 5. Robertson S. Cataract Epidemiology. 6. Lakin GF. [Biometry]. Moscow: Vysshaia shkola; 1990 Russian 7. Kovtun MI. [Analysis of gender differences in time from diagnosis of cataract to surgery]. Vestnik problem biologii i meditsiny. 2012;4(2):91-5 Russian 8. Kovtun MI. [Medical and social characteristics of patients with cataract]. Vestnik problem biologii i meditsiny. 2015;2(3):135-9 Russian 9. Kovtun MI. [Organization of ophthalmological care for patients with cataract under reforms in Ukraine]. Arkhiv oftalmologii Ukrainy. 2015;3(2):14-9 Russian 10.Kovtun MI. [Results of Structure Assessment which Accompanying Morbidity of Cataract Patients]. Vestnik problem biologii i meditsiny. 2012;4(1):120-4 Russian 11.Kovtun MI. Assessment result of cataract stages distribution and concomitant diseases structure. East European Scientific Journal. 2016; 6(1):48-52 12.Clark A, Morlet N, Ng JQ, et al. Whole population trends in complications of cataract surgery over 22 years in Western Australia. Ophthalmology. 2011 Jun;118(6):1055-61 13.Greenberg PB, Tseng VL, Wu WC. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. 2011 Mar;118(3):507-14 14.Jaycock P, Johnston RL, Taylor H, et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye. 2009;23:38–49 15.Kurmangaliieva MM. [Surgical treatment of glaucoma in combination of cataract]. Takhchidi KhP, Panteleiev EN, Bessarabov AN, et al. [Predicting early postoperative complications in patients undergoing simultaneous cataract and glaucoma surgery]. Oftalmokhirurgiia. 2009;2:8-13 Russian
|