J.ophthalmol.(Ukraine).2017;2:33-37.
|
https://doi.org/10.31288/oftalmolzh201723337 Use of photomyostimulation method in treatment of patients with advanced primary open angle glaucoma
V.A. Putienko V.S. Ponomarchuk, Dr.Sc. (Med.), Prof. Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine
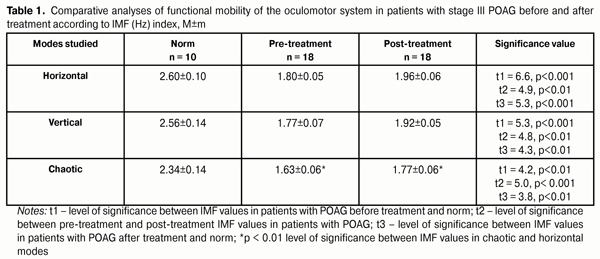
Purpose: To assess the efficacy of a photomyostimulation method in treatment of patients with stage III (advanced) primary open angle glaucoma (POAG) with drug-compensated intraocular pressure. Material and Methods: 18 patients with POAG were examined. Treatment was performed using an ophthalmic photomyostimulation unit (FMS-1). The treatment course consisted of 10 sessions. The duration of the session was 10 minutes with patient’s optimal impulse movement frequency (IMF) in a chaotic mode under scotopic conditions. The treatment success was assessed according to changes in functional mobility of the oculomotor system on the ground of IMF values and in lability of the visual system according to critical flicker fusion frequency (CFFF), Hz, and critical flicker appearance frequency (CFAF), Hz. Also, computed static perimetry and tonography data were assessed. Results: The IMF values in horizontal, vertical and chaotic modes significantly increased after treatment, however, remained far below the norm. The CFFF index of visual system lability both in the static mode and in three kinetic modes (horizontal, vertical, and chaotic) significantly increased after treatment to the norm. The similar changes were noted when studying the lability of the visual system according to the CFAF values in the static and three kinetic modes. The treatment performed resulted in improving the hydrodynamics of the eye. Thus, the facility of aqueous outflow increased by 31.2%, a Ро/С coefficient decreased by 20.0%, and the rate of aqueous flow increased by 35.5%. The mean deviation of light sensitivity (MD) significantly increased by 7.3% and the mean retinal light sensitivity (MS) according to all MS threshold values significantly increased by 8.8% as well. Summarized visual field according to eight quadrants was enlarged after treatment by 12.0%. Conclusions: The data obtained give the evidence that the photomyostimulation method is highly successful in the treatment of patients with stage III POAG and can be included in a therapy of such patients. Key words: glaucoma, oculomotor system, photomyostimulator Background Progressive damage to the nerve tissue in patients with primary open angle glaucoma (POAG) leads to progressive visual field loss, a decrease in contrast sensitivity, deterioration of adaptation to changing light conditions, which affect the quality of life of the patients [1, 2, 3]. Visual field loss increases the load on the oculomotor system since there is the need to make more eye movements towards the visual object [4, 5]. It is known that patients with glaucoma are able to accomplish natural actions almost as quickly as normally sighted controls. However, when performing an unfamiliar task, the glaucoma patients are twice slower, and patients with advanced glaucoma are 3-4 times slower, as compared to controls [6]. Previous investigations have shown that mobility of the oculormotor system in advanced (stage III) POAG patients is significantly decreased according to an impulse movement frequency (IMF) index in all modes. Also, lability of the visual analyzer is decreased according to indices of critical flicker fusion frequency (CFFF) and critical flicker appearance frequency (CFAF). These data give evidence that stimulation of the oculormotor activity in glaucoma patients is of great importance and can significantly increase the quality of life of the patients [7]. One of the oculormotor system stimulation methods is a photomyostimulation technique which enables improving the functions of the extraocular muscles. The method consists in stimulation of the muscular system of the eye by keeping an eye on the illuminated test object, which trains all striated muscles of the oculomotor system and improves their functions. To our best knowledge, the photomyostimulation method has not been used in the treatment of patients with stage III POAG, which was the background of the present investigation. The purpose of the present study was to investigate the efficacy of the photomyostimulation method in the treatment of patients with stage III POAG with compensated intraocular pressure. Materials and Methods We observed 18 patients (18eyes) with primary open angle glaucoma (POAG) of stage III (advanced POAG) with drug-compensated intraocular pressure (IOP). Glaucoma was diagnosed according to data of ophthalmoscopy, gonioscopy, tonography, computed static perimetry, optic coherence tomography (OCT). OCT was performed using Carl Zeiss (CIRRUS Photo 800) and the mean thickness of retinal nerve fiber layer (RNFL) was registered. The patients’ age averaged 68.6±1.07. Visual acuity ranged from 0.1 to 0.5 and averaged 0.32±0.03. Clinically, optic disc cupping was enlarged in all cases and reached the rim of the disc in 15 eyes (83%). In all cases, computed static perimetry data revealed a concentric visual field constriction, up to 15° from the fixation point, in one or more segments. Computed static perimetry was performed using Oculus vision field analyzer (TOPCON) with Glaucoma treshold, 30-2 Fast threshold. Mean deviation (MD) of the retinal light sensitivity from the norm and mean light sensitivity (MS) in all determined threshold values were computed. MD was within -12.6 dB to -15.0 dB with the average value of -13.66±0.14 dB; MS ranged from 2.89 to 6.47 with the average value of 4.62±0.22. The OCT mean thickness of RNFL was 56.05±1.02 mm within 49-94 mm, and the mean cup-to-disc ratio was 0.86±0.07 within 0.81-0.91. Tonography was performed using the A.P.Nesterov method. Mean tonography values were as follows: intraocular pressure, Р0 – 16.05±1.00 mmHg; the facility of aqueous outflow, С – 0.16±0.012 mm3/min/mmHg; the rate of aqueous flow, F – 1.65±0.4 mm3/mean; a P0/C coefficient – 99.7±9.66. The patients were treated using an ophthalmic photomyostimulator unit (FMS-1). The treatment duration was 10 sessions. The session lasted 10 minutes with patient’s optimal impulse movement frequency (IMF) in a chaotic mode under scotopic conditions. The patients kept his eyes on the test object moving for one minute and, then, had one-minute rest. The treatment success was assessed according to changes in functional oculomotor system mobility and visual system lability; the changes in former were determined on the ground of IMF values, Hz, in three kinetic modes: horizontal (H), vertical (V), and chaotic (C), and those of the latter were according to critical flicker fusion frequency (CFFF), Hz, and critical flicker appearance frequency (CFAF), Hz, in three kinetic modes (H, V, C) and a static (motionless) mode with a central fixation point. Also, post-treatment computed static perimetry and tonography data were assessed. STATISTICA 7.0 software package was used for statistic data processing. A pairwise Student (t) criterion and a nonparametric ?2 criterion were used for data analyses. Critical p-level when testing statistical hypothesis was equal to 0.05. Results The mean value of impulse movement frequency (IMF) in the horizontal mode before treatment was 1.80±0.05 Hz and significantly increased after treatment up to 1.96±0.06 Hz. i. e. by 8.9% (р < 0.01). In the vertical mode, the mean IMF value increased by 8.5% from pre-treatment 1.77±0.07 Hz to post-treatment 1.92±0.07 Hz, the difference is statistically significant (р < 0.01). The chaotic mode IMF value was on average 1.63±0.06 Hz before treatment, and significantly increased after treatment to 1.77±0.06 Hz, or by 8.6%, p<0.001. It should be noted that, despite the improvements in mobility of the oculomotor system after the photomyostimulation course performed, the IMF values in the three modes remained significantly below the norm (Table 1).
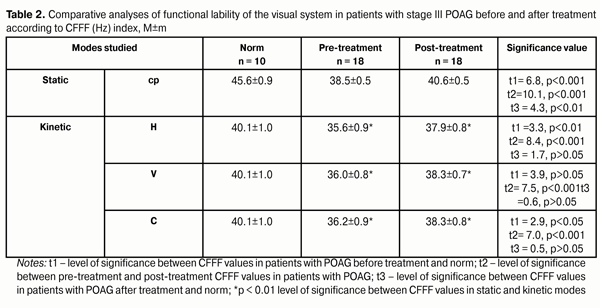
Thus, functional mobility of the oculormotor system was significantly improved after treatment according to the IMF index in the three modes. Moreover, both the pre-treatment and post-treatment IMF values were significantly lower in the chaotic mode than in the horizontal one. The CFFF index of visual system lability in the static mode (central fixation point) was 38.5±0.5 Hz and 40.6±0.5 before and after treatment, respectively, i.e. that increased by 5.5%; the difference is statistically significant, р<0.001. Kinetic H-mode CFFF was 35.6±0.9 Hz and 37.9±0.8 Hz before and after treatment, respectively, i.e. that increased by 6.5%. V-mode CFFF was 36.0±0.8Hz and 38.3±0.7 Hz before and after treatment, respectively, i.e. that significantly increased by 6.4%. The C-mode CFFF value significantly increased by 5.8%, from pre-treatment 36.2±0.9 Hz to post-treatment 38.3±0.8 Hz. The post-treatment CFFF value in the static mode remained significantly lower than the norm; however, that in the kinetic mode did not differ significantly from the norm, (p>0.05). It should be noted that both the pre-treatment and post-treatment mean CFFF values were significantly lower in kinetic HVC-modes than those in the static mode (Table 2).
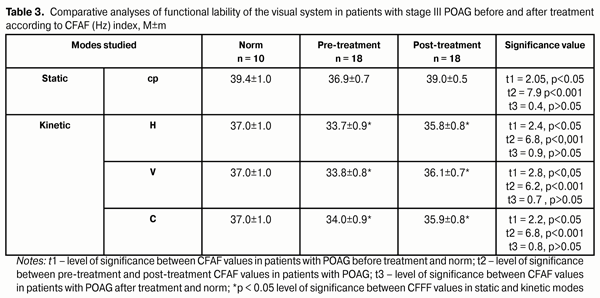
Hereafter, we studied functional lability of the visual system before and after treatment according to the CFAF index. The mean pre-treatment and post-treatment CFAF value in the static mode was 36.9±0.7 Hz and 39.0±0.5 Hz, respectively, i.e the index value increased by 5.7%; the difference is statistically significant (р<0.001). The kinetic H-mode CFAF value also significantly increased by 6.2% (р<0.001), i.e. from pre-treatment 33.7±0.9Hz to post-treatment 35.8±0.8 Hz. The kinetic V-mode CFAF value was 33.8±0.8 and 36.1±0.7 before and after treatment, respectively, i.e. increased by 6.8% (р<0.001). The increase in the chaotic mode was 5.8%, from pre-treatment 34.0±0.9 Hz to post-treatment 35.98±0.8 Hz; the difference is statistically significant. All post-treatment values did not differ significantly from the norm (р>0.05). Moreover, the mean CFAF values were significantly lower in the kinetic HVC-modes than in the static mode (Table 3).
Thus, the treatment performed in patients with advanced POAG resulted in the improvement of visual system functional lability according to all indices studied, except the static-mode CFFF index; it did not differ significantly from the norm, which gives the evidence of a positive effect of photomyostimulation on the visual system lability function in this stage of POAG. Hereafter, we studied the state of the hydrodynamics of the eye before and after the photomyostimulation treatment course. The initial mean value of the facility of aqueous outflow (C) was 0.16±0.002 mm3/min and improved after treatment up to 0.21±0.005 mm3/min, i.e. by 31.2% (р = 0.001). The Ро/С coefficient was 99.7±2.34 and 79.7± 1.83, before and after photomyostimulation sessions, respectively, i.e. significantly improved by 20.0% (р = 0.001). The rate of aqueous flow (F) also improved by 31.5% from 1.65±0.1 to 2.17±0.05 mm3/min (р = 0.001). The therapy performed did not significantly influence on the IOP level. The mean post-treatment IOP (Rо) was 16.55±0.22 mmHg with the initial IOP of 16.05±0.24 mmHg (р=0.12). No statistically significant difference was noted in pre-treatment and post-treatment visual acuity (р=0.56), which was 0.32±0.03 and 0.34±0.03, respectively. Improvement was noted in computed static perimetry data. The mean deviation of light sensitivity improved by 7.3% (р = 0,001), from -13.7±0.14 dB до -12.7±0.15 dB; and the mean retinal light sensitivity according to all MS threshold values increased from 4.62±0.22 dB to 5.03±0.23 dB, i.e. by 8.8% (р = 0.034). Also, a significant enlargement was noted in summarized visual field according to 8 quadrants: from pre-treatment 248.9°±7.03° to post-treatment 278.9°± 7.45°, i.e. by 12.0% (р=0.0041). The data are given in the Table 4.
Thus, oculomotor system stimulation with the method proposed enabled improving the eye hydrodynamics indices: the facility of aqueous flow increased by 31.2%, the Ро/С coefficient decreased by 20.0%, the rate of aqueous flow increased by 31.5%, which can be explained by an increase in blood flow in anterior ciliary arteries that rise from the muscular branches. Generally, the use of the photomyostimulation method in treatment of patients with stage III (advanced) POAG resulted in improving the functional mobility of the oculomotor system (the IMF values in the three modes improved after treatment) and enabled improving the eye hydrodynamics indices as well as enlarging the summarized visual field index and improving significantly the light sensitivity of the retina. Conclusions The data obtained give the evidence that the photomyostimulation method is highly successful in the treatment of patients with stage III POAG and can be included in a therapy of such patients.
References 1. Heijl A, Bengtsson B, Hyman L et al. Early Manifest Glaucoma Trial Group Natural history of open-angle glaucoma. Ophthalmology. 2009;116(12);2271-6. 2. Hirneiss C, Kort?m K. Quality of Life in Patients with Glaucoma. Klin Monbl Augenheilkd. 2016;233 (2):148-53. 3. Lisboa R, Chun YS, Zangwill LM. Association between rates of binocular visual field loss and vision-related quality of life in patients with glaucoma. JAMA Ophthalmol. 2013;131 (4):486-94. 4. Hood DC, Raza AS, De Moraes CGV. Initial arcuate defects within the central 10 degrees in glaucoma. Invest Ophthalmol Vis Sci. 2011;52:940-6. 5. Junoy Montolio FG, Meems W, Janssens MS. Lateral Inhibition in the Human Visual System in Patients with Glaucoma and Healthy Subjects: A Case-Control Study. PLoS One. 2016;11(3). 6. Dive S, Rouland JF, Lenoble Q et al. Impact of Peripheral Field Loss on the Execution of Natural Actions: A Study With Glaucomatous Patients and Normally Sighted People. J Glaucoma. 2016;25(10):889-96. 7. Putienko V.A., Ponomarchuk V.S Mobility of the oculomotor system and lability of the visual analyzer in patients with primary open-angle glaucoma. J.ophthalmol.(Ukraine).2017;1:29-33.
|