J.ophthalmol.(Ukraine).2017;2:25-32.
|
https://doi.org/10.31288/oftalmolzh201722532 Quality of life in patients with AMD after laser stimulation of the retina with subsequent nutrient supplementation
O.V. Guzun, Cand Sc (Med) A.R. Korol, Dr Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: olgaguzun@mail.ru
Background: Previous studies of the psychological component of the quality of life (QoL) in patients with age-related maculopathy (ARM) and macular degeneration (AMD) have found that these patients were more likely to show signs of depression compared to older adults with good vision, which, along with their poor visual function, substantially worsened their QoL. Purpose: To investigate the benefits of laser stimulation of the retina with subsequent 6-month daily nutrient supplementation for QoL in patients with ARM and AMD. Materials and Methods: The study involved 34 patients (42 eyes; 16 (47%) male and 18 (53%) female; age, 47 years to 76 years) with ARM and dry AMD. Most of the patients were younger than 65 years. All study eyes received 10 every-day sessions of diode laser stimulation of the retina (LSR) (wavelength, 650 nm; irradiance, mW/cm2; treatment timing, 300 s). Thereafter, patients were administered one capsule of Nutrof® Total daily for 6 months. They completed the 25-item version of the National Eye Institute Visual Function Questionnaire (NEI VFQ-25) and Hospital Anxiety and Depression Scale (HADS) at baseline, immediately after a course of LSR, and after a subsequent 6-month course of nutrient supplementation. Results: In 30 patients (88%), the mean percentage increase in visual acuity was 33.3% after a 6-month course of nutrient supplementation. The HADS scores decreased by 18% after a course of LSR (this decrease was significant), and by 21% after a subsequent 6-month supplementation with Nutrof® Total. The overall emotional distress score improved by 43.1% in 29 patients (85.3%) after a 6-month daily nutrient supplementation. There was a statistically significant improvement in NEI VFQ-25 overall composite following treatment (F=117.6; p=0.00001). This score increased to 70.1 immediately after a course of LSR, and to 76.4 after 6 months of supplementation with Nutrof® Total. Conclusions: The comprehensive treatment (a course of laser stimulation of the retina with subsequent oral supplementation with Nutrof® Total) for ARM and dry AMD resulted in improved visual function, decreased anxiety and depression, and substantially improved QoL at the 6-month time-point. Key words: age-related macular degeneration, quality of life, laser stimulation of the retina, nutrient supplementation
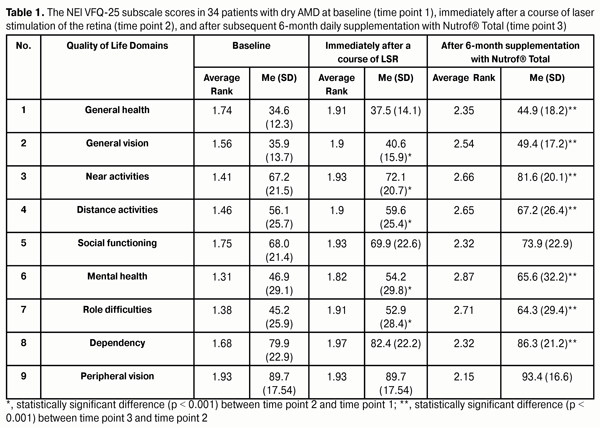
Introduction In 1997, Lee and colleagues [1] reported on the findings of a large-scaled study of the Quality of Life (QoL) of individuals with visual disorders using the SF-36, a general functioning and well-being instrument. They found that the impact of blurred vision on role limitations due to physical health problems was significantly greater than that of the disorders of other organs and body systems (including those presenting an immediate danger to life). This fact caused significant interest in the QoL of patients with various ocular disorders [2]. The 51-item field test version of the National Eye Institute Visual Function Questionnaire (NEI VFQ) was designed in the nineties in the USA to capture the influence of vision on multiple dimensions of health-related quality of life. However, that version was too long and required too much time to complete [3-4]. Therefore, the 25-item and 39-item (the NEI VFQ-25 and NEI VFQ-39) versions were designed and have been used for research and clinical settings [4-6]. Popescu and colleagues [7] have investigated a psychological component of the QoL in patients with age-related eye diseases and found that these patients were more likely to show signs of depression compared to older adults with good vision. Of patients with age-related macular degeneration (AMD), 11% to 44% have been reported to have significant depressive symptoms [8-10]. Depression develops in AMD patients as a result of reduced QoL. Thus, the prevalence of depressive disorders in community-dwelling adults with AMD has been found to be twice as high as that in community-dwelling elderly [11]. The use of low-intensity laser irradiation (LILI) has been found promising in treatment of early AMD due to basic mechanisms of action of LILI and non-invasiveness of the technique. In 1979, Linnik and colleagues demonstrated that increased synthesis of DNA in nuclei of the ganglial and neuroepithelial cells occurred immediately following retinal exposure to LILI and maintained for long periods, with improvement in cell resistance to damaging factors [12]. AMD requires long-term, often complex treatment regimens. Antioxidant agents (including xanthophylls e.g. lutein and zeaxanthin) are known for their capability for selective accumulation in the macula. They improve the function of the retinal pigment epithelium (RPE), and contribute to increase in RPE density and to normalization of retinal metabolic processes. Nutrients from the AREDS2 study (lutein, zeaxanthin, vitamin C, vitamin E, zinc, copper, eicosapentanoic acid [EPA], and docosahexanoic acid [DHA]) remain the most proven nutritional therapy for reducing the rate of advanced AMD [13]. In addition, in a 6-month control trial by Sinn and colleagues [14], it has been found that supplementing a diet with DHA and EPA reduced depressive symptoms and the risk of progressing to dementia in elderly people with mild cognitive impairment. We aimed to investigate the benefits of laser stimulation of the retina with subsequent 6-month daily nutrient supplementation for QoL in patients with age-related maculopathy (ARM) and AMD. Materials and Methods This was a prospective, open pilot study involving 34 patients (42 eyes; 16 (47%) male and 18 (53%) female; age, 47 years to 76 years) with ARM and dry AMD. Most of the patients were younger than 65 years. 91% of patients were of the working age. 42 eyes (62% of eyes of patients) included in the study had early ARM and dry AMD, with extrafoveal focus of atrophy. Twenty-six fellow eyes (38%) had advanced macular degeneration. All study eyes received 10 every-day sessions of diode laser stimulation of the retina (LSR) (wavelength, 650 nm; irradiance, mW/cm2; treatment timing, 300 s) using diode laser SM-4.3. Thereafter, patients were administered one capsule of Nutrof® Total (Laboratories Thea, France) daily for 6 months. The capsule contains polyunsaturated fatty acids of the omega-3 series (EPA, 40%; DHA, 20%); Vitamin C, 240mg; Vitamin E, 30 mg; Marigold extraction (lutein, 10 mg; zeaxanthin, 2 mg) and Vitis vinifera extraction (Resveratrol, 1 mg; copper, 500 ?g; Selenium, 25 ?g; and glutathione). Patients underwent comprehensive clinical and functional ophthalmological examination (visual acuity assessment, perimetry, ophthalmoscopy, fluorescence angiography, fundus camera imaging and optical coherence tomography) at baseline, immediately after a course of LSR, and after 6 months of supplementation with Nutrof® Total. The Russian-language version of the NEI VFQ-25 was used to assess the influence of vision on health-related quality of life. The reliability and validity of the NEI VFQ have been confirmed in a number of studies [15-17]. The 25 questions in the NEI-VFQ-25 are grouped in 12 sub-scales (including general health, general vision, ocular pain, near activities, distance activities, social functioning, mental health, role difficulties, dependency, driving, color vision and peripheral vision). A vision-specific composite score is calculated by averaging the vision-related subscale scores. Scores range from 0 to 100 with higher scores indicating better functioning. Patients completed the NEI VFQ-25 and HADS at baseline, after a course of LSR, and after a subsequent 6-month course of nutrient supplementation. Anxiety and depression were assessed using the Hospital Anxiety and Depression Scale (HADS) designed by Zigmond and colleagues [18]. Interpretation of the subscale scores (range from 0 to 21) was based on the following categories indicating clinical levels of anxiety and depression: 0 to 7, normal (no anxiety or depression); 8 to 10, moderate (subclinical anxiety or depression); and 11 to 21, caseness (clinical anxiety or depression). Patients completed the NEI VFQ-25 and HADS in 5-10 minutes. Longitudinal changes in the QoL were analyzed using Friedman’s ANOVA test. Post-hoc pairwise comparisons were made using the Wilcoxon signed-rank test. Mean (M), median (Ме), standard deviation (SD) and standard error of mean (m) were calculated to demonstrate longitudinal changes in QoL. Changes in composite scores of NEI-VFQ-25 and changes in HADS depression/anxiety scores were evaluated among participants using ANOVA and were presented using M and m. Pearson or Spearman correlation coefficients were used to assess the relationships between study variables. Statistical analysis was performed with the use of STATISTICA-10 software (StatSoft Inc, Tulsa, OK). Results and Discussion Vision-related QoL (NEI-VFQ 25 questionnaire) study results General Health score was not included into the NEI VFQ-25 composite score; however, it did reflect general health conditions. At baseline, 21 patients (62%) assessed their general health as “satisfactory” and 13 (38%) as “good”. Immediately after a course of LSR, one patient (3%) improved his self-assessment of general health to “very good”, with 15 patients (44%) reporting their general health as “good” and 18 patients (53%) as “satisfactory”. Self-assessment of general health worsened in no patients at this time point. Table 1 demonstrates the NEI VFQ-25 subscale scores in patients with dry AMD at baseline (time point 1), immediately after a course of LSR (time point 2), and after 6 months of supplementation with Nutrof® Total (time point 3). The table shows that, at time points 2 and 3, the average ranks in all the NEI VFQ-25 subscale scores in study patients increased compared to those at the preceding time point. At 6 months of nutrient supplementation, a statistically significant mean improvement from baseline was observed in the General Health subscale (?F2=22.3; p=0.0001).
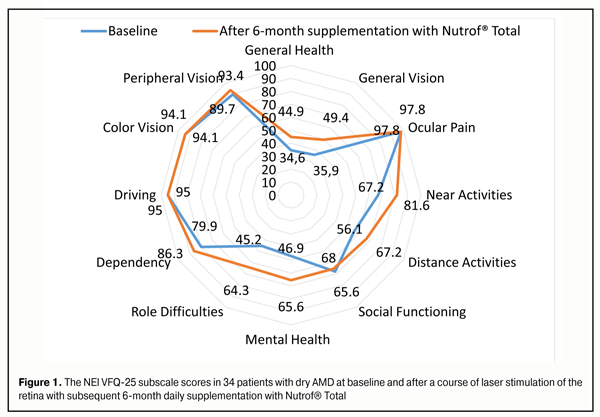
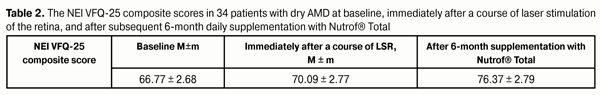
Immediately after a course of LSR and after 6-month nutrient therapy, the General Vision subscale score improved by 13% (p=0.01) and by 22% (p=0.0001), respectively. With regard to the Near Activities domain, the numbers of patients reporting no difficulty, a little difficulty, or moderate difficulty with reading ordinary print in newspapers were 7 (20.6%), 13 (38.2%), and 14 (41.2%), respectively, at baseline. These numbers changed to 11 (32%), 17 (50%), and 6 (17.6%), respectively, immediately after a course of LSR, and to 22 (64.7%), 6 (17.6%) and 6 (17.6%), respectively, after a 6-month course of nutrient supplementation. At 6 months of nutrient supplementation, a statistically significant mean improvement from baseline was observed in the Near Activities subscale (?F2=42.9; p=0.0001). With regard to the Distant Activities domain, the numbers of patients reporting no difficulty, a little difficulty, moderate difficulty or extreme difficulty with reading street signs or names of stores were 7 (20.6%), 9 (26.5%), 10 (29.4%) and 8 (23.5%), respectively, at baseline. Responders’ opinions remained virtually unchanged after a course of LSR. After a 6-month course of nutrient supplementation, the numbers of patients reporting a little or moderate difficulty with reading street signs or names of stores did not change, whereas the numbers of patients reporting no difficulty or extreme difficulty changed to 11 (32.4%) and 4 (11.8%), respectively. Both immediately after a course of LSR and at 6 months of nutrient supplementation, statistically significant mean improvement from baseline was observed in the Distant Activities subscale (?F2=41.4; p=0.0001). With regard to the Social Functioning domain, the numbers of patients reporting no difficulty, a little difficulty, moderate difficulty or extreme difficulty with seeing how people react to things you say were 4 (11.8%), 14 (41.2%), 13 (38.2%) and 3 (8.8%), respectively, at baseline. Immediately after a course of LSR, 6 subjects reported improvement in these problems. However, improvement in the Social Functioning domain was not significant at time points measured (?F2=20.4; p=0.06). With regard to the Mental Health domain, the numbers of patients reporting “being worried about their eyesight” a little of the time, some of the time, most of the time and all of the time were 4 (11.8%), 14 (14.2%), 13 (38.2%) and 3 (8.8%), respectively, at baseline. These numbers changed to 10 (29.4%), 11 (32.4%), 6 (17.6%), and 7 (20.6%), respectively, immediately after a course of LSR, and to 7 (20.6%), 13 (38.2%), 2 (17.6%) and 7 (20.6%), respectively, after a 6-month course of nutrient supplementation. Improvement in the Mental Health domain was significant at time points measured (?F2=20.4; p=0.06). With regard to the Role Difficulties domain, the numbers of patients reporting “being limited in how long they can work or do other activities because of their vision” none of the time, a little of the time, some of the time, most of the time and all of the time were 7 (20.6%), 12 (35.3%), 6 (17.6%), 4 (11.8%) and 5(14.7%), respectively, at baseline. These numbers did not change immediately after a course of LSR, and changed to 20 (58.8%), 7 (20.6%), 2 (5.9%) and 4 (11.8%), respectively, after a 6-month course of nutrient supplementation. Improvement in the Role Difficulties domain was significant at the end of the study (?F2=45.6; p=0.001). The items related to the Dependency domain were answered using a five-point scale: definitely true (1), mostly true (2), not sure (3), mostly false (4), and definitely false (5). Thus, 5 subjects (14.7%), 2 subjects (5.9%), 11 subjects (32.3%) and 16 subjects (47%) scored “I need a lot of help from others because of my eyesight” item as 1, 4, 3 and 5, respectively, at baseline. Improvement in their need for help from others was reported by 4 subjects (11.8%) after a course of LSR, and by 6 (17.6%) more subjects after a 6-month course of nutrient supplementation (?F2=23.1; p=0.001). With regard to the Peripheral vision domain, the numbers of patients reporting no difficulty, a little difficulty or some difficulty with “noticing objects off to the side while they were walking along” were 24 (70.6%), 6 (17.6%), and 4 (11.8%), respectively, at baseline. Responders’ opinions remained virtually unchanged after a course of LSR. Improvement in their difficulty with “noticing objects off to the side” was reported by 5 subjects (14.7%) after a 6-month course of nutrient supplementation (?F2=10.1; p=0.04). With regard to the Driving domain, its items were not included in the composite score, since by the time of the study, only 15 patients had a driving license, and neither of them had any driving difficulty. Ocular Pain domain items and Color Vision domain items were not included in the composite score, since there were no longitudinal changes in these domains (p ? 0.05). Figure 1 presents mean NEI VFQ-25 subscale scores in patients with dry AMD at the tree time points (baseline, immediately after a course of LSR, and after a 6-month course of supplementation with Nutrof® Total). It should be noted that NEI VFQ–25 methodology provides detailed characterization of individual parameters of changes in QoL in patients with dry AMD. We analyzed longitudinal changes in mean VFQ-25 composite score (sum of 9 individual domain subscores) to represent the psychological status of patients in a comprehensive manner (Table 2). At baseline, the mean (SD) NEI VFQ-25 overall composite score was 66.8 (15.6) (range, 36.3 to 90.6). These findings agree with those of Karadeniz and colleagues [19] (84.7 points).
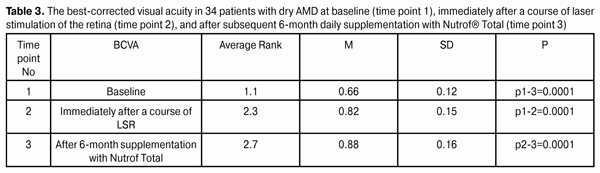
The analysis revealed a statistically significant improvement in QoL composite score following treatment (F=117.6; p=0.00001). The NEI VFQ-25 overall composite score increased to 70.1 (range, 39.4 до 92.8) immediately after a course of LSR. After 6 months of supplementation with Nutrof® Total, the score increased to 76.4 (range, 39.4 до 92.8), with a significant improvement in their social and psychological status. The baseline best-corrected visual acuity (BCVA) ranged from 0.45 to 0.85, with the mean BCVA (SD) of 0.66 (0.12) (Table 3). The mean BCVA (SD) improved to 0.82 (0.15) (range, 0.5 to 1.0) immediately after a course of laser therapy, and to 0.88 (0.16) after 6 months of supplementation with Nutrof® Total. At baseline, the percentage of eyes having a BCVA of 0.5 to 0.6 was substantially higher than of those having a BCVA of 0.9 to 1.0 (44% and 23%, respectively). The latter percentage increased to 47% by the end of the study. Table 3 shows that after a course of LSR and a subsequent 6-month supplementation with Nutrof® Total, an increase in mean visual acuity rank was statistically significant (?F2=59.4; p=0.00001): in 30 patients (88%), the mean percentage increase in visual acuity was 33.3%.
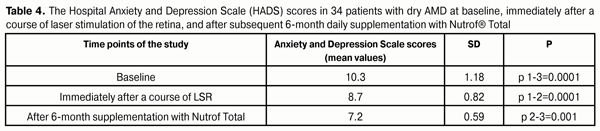
The improvement in the mean composite score after a 6-month nutrient supplementation was found to correlate with the improvement in mean BCVA (r=0.62; p=0.0001) and not to correlate with age (r=0.06; p=0.74) or with baseline BCVA (r=-0.11; p=0.52). Consequently, the improvement in BCVA, if achieved, would improve the QoL even in elderly patients with AMD. HADS questionnaire study results At baseline (before treatment), 17 patients (50%) had clinical or subclinical anxiety and/or depression (with HADS scores >11). Only one patient (2.9%) had clinical anxiety and/or depression after a course of LSR. Twenty-eight patients (82.4%) had normal HADS scores, and only 6 (17.6%) had clinical anxiety and/or depression after a 6-month nutrient supplementation. Although the intersex difference in anxiety and depression levels was not significant, among 31 study patients, the women's baseline (pre-treatment) and post-treatment mean HADS scores were 8% worse than the men's. The HADS anxiety and depression scores in patients with dry AMD ranged from 8 to 12.5 at baseline and decreased by 18% after a course of LSR, ranging from 7.5 to 10.5 points (this decrease was significant), and by 21% after a subsequent 6-month supplementation with Nutrof® Total, ranging from 6 to 9 points (Table 4). The overall emotional distress score improved by 43.1% in 29 patients (85.3%) after a 6-month daily nutrient supplementation.
It is particularly important that, in patients with ARM and dry AMD, at the end-point of the study, after a 6-month supplementation with Nutrof® Total, the mean composite QoL score (76.4) was higher, whereas the anxiety and depression levels were significantly lower than at previous study points, which is consistent with the findings of other studies on the effect of omega-3 fatty acids on depressive and anxiety symptoms [20]. In addition, in our study patients, visual function was found to be stabilized after a course of supplementation with Nutrof® Total. This finding agrees with that of Ma and colleagues [21, 22]. In their study of the effect of lutein and zeaxanthin on macular pigment and visual function in patients with early AMD, macular pigment optical density increased significantly during 48 weeks, and, at 48 weeks, a trend toward improvement was seen in BCVA. The correlation between changes in visual acuity and QoL was moderate and statistically significant nearly on all subscales of the NEI VFQ–25. The absence of significant relationships between peripheral vision and QoL, and between ocular pain and QoL, might be explained by the fact that peripheral vision impairment and ocular pain are not characteristic for patients with AMD. While viewing AMD as a chronic disease that results in a gradual and progressive loss of visual function [23], is should be noted that what is required is not only an objective examination of the patient but also an assessment of the subjective component of the patient’s condition. This results from the fact that vision is not only important for spatial orientation, but also significantly contributes to emotional well-being and to adapting to real-life situations [1]. It has been reported that in patients with AMD, depression scores were positively correlated with visual acuity [24]. In foreign studies on QoL in AMD [25], it has been found that, in spite of the disease, numerous respondents were committed to engage in, and enjoy life. This is an important concept for clinicians and those who offer support programs to integrate into their care planning and reinforce in messaging to patients with the condition [25]. Loss of visual function in patients with AMD affects all QOL domains. However, even in the absence of marked loss of vision in patients with AMD, the patient’s perception of incurability of the disease and fear of possible blindness cause emotions of anxiety [26]. Omega-3 fatty acids like eicosapentanoic acid (EPA) and docosahexanoic acid (DHA) are involved in a variety of processes in neural cells, cell membrane stabilization, and gene expression regulation. Nutrient imbalance and deficiency substantially influence brain function throughout life [14]. After a course of LSR, provision of additional protection to ocular tissues through daily oral supplementation with Nutrof® Total was accompanied by normalization of BCVA and improvement in patients’ social and psychological status, which substantially improved QoL scores and decreased depression scores. This is in agreement with the study by Tao and colleagues [27] in which the authors found correlation between visual acuity and QoL after enhancement of antioxidant defense system. Conclusion The comprehensive treatment (a course of laser stimulation of the retina with subsequent oral supplementation with Nutrof® Total) for ARM and dry AMD resulted in improved visual function, decreased anxiety and depression, and substantially improved QoL at the 6-month time-point.
References 1. Lee PP, Spitzer КА, Hays RD. The impact of blurred vision on functioning and well–being. Ophthalmology. 1997 Mar;104(3):390–6 2. Mihaila V, Enachescu D, Davila С. General Population Norms for Romania using the Short Form 36 Health Survey (SF-36). QoL Newsletter. 2000;26:17–8 3. Lisochkina AB, Kuznetsova TI. [Use of the NEI VFQ-25 for assessing QoL in patients with age-related macular degeneration]. Oftalmologicheskie vedomosti. 2010; 3(1):26–30 Russian 4. Yelin E. Measuring Functional Capacity of Persons with Disabilities in Light of Emerging Demands in the Workplace. Washington (DC): National Academies Press (US); 1999 5. Boiko EV, Sysoev VN, Novik A.A., Kuz'micheva OV. [Quality of life and psychological status of patients with glaucoma and cataract]. Glaucoma. 2010; 1:21–5 Russian 6. Orr P, Rentz AM, Margolis MK, et al. Validation of the National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25) in Age-Related Macular Degeneration. Invest Ophthalmol Vis Sci. 2011 May 18;52(6):3354–9 7. Popescu ML, Boisjoly H, Schmaltz H, Kergoat MJ, et al. Explaining the relationship between three eye diseases and depressive symptoms in older adults. Invest Ophthalmol Vis Sci. 2012 Apr 24;53(4):2308–13 8. Eramudugolla R, Wood J, Anstey KJ. Co-morbidity of depression and anxiety in common age-related eye diseases: a population-based study of 662 adults. Front Aging Neurosci. 2013 Oct 2;5:56 9. Jivraj J, Jivraj I, Tennant М, Rudnisky С. Prevalence and impact of depressive symptoms in patients with age-related macular degeneration. Can J Ophthalmol 2013;48:269–73 10.Mathew RS, Delbaere К, Lord SR, et al. Depressive symptoms and quality of life in people with age- related macular degeneration. Ophthalmic Physiol Opt. 2011 Jul;31(4):375–80 11.Brody BL, Gamst AC, William RA, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration. Ophthalmology. 2001;108:1893–900 12.Linnik LA, Usov NI, Baronetskaia IL et al. [Laser stimulation of the functional activity of ocular tissues. Abstracts of the 5th National Ophthalmological Congress of the USSR]. Tashkent, 25-29 September, 1979. Vol. 3. 126-7 p. Russian 13.McCusker MM, Durrani K, Payette MJ, Suchecki J. An eye on nutrition: The role of vitamins, essential fatty acids, and antioxidants in age-related macular degeneration, dry eye syndrome, and cataract. Clin Dermatol. 2016 Mar-Apr;34(2):276–85 14.Sinn N, Milte CM, Street SJ, et al. Effects of n-3 fatty acids, EPA v. DHA, on depressive symptoms, quality of life, memory and executive function in older adults with mild cognitive impairment: a 6-month randomised controlled trial. Br J Nutr. 2012 Jun;107(11):1682–93 15.Novik AA, Ionova TI. [A guide for assessing quality of life in medical setting]. 2nd ed. Moscow: OLMA Media Group; 2007 Russian 16.Clemons TE, Chew EY, Bressler SB, McBee W. National eye institute visual function questionnaire in the age–related eye disease study (AREDS): Report No. 10. Arch Ophthalmol. 2003 Feb;121(2):211–7 17.Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001 Jul;119(7):1050-8 18.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression scale. Acta Psychiatr Scand. 1983 Jun;67(6):361–70 19.Karadeniz Ugurlu S, Kocakaya Altundal AE, Altin Ekin M. Comparison of vision-related quality of life in primary open-angle glaucoma and dry-type age-related macular degeneration. Eye (Lond). 2016 Nov 4. [Epub ahead of print]. 20.Uauy R, Dangour AD. Nutrition in brain development and aging: role of essential fatty acids. Nutr Rev. 2006 May;64(5 Pt 2):S24–33 21.Lima VC, Rosen RB, Farah M. Macular pigment in retinal health and disease. Int J Retina Vitreous. 2016 Aug15;2:19 22.Ma L, Yan SF, Huang YM, et al. Effect of lutein and zeaxanthin on macular pigment and visual function in patients with early age-related macular degeneration. Ophthalmology. 2012 Nov;119(11):2290–7 23.Cheung LK, Eaton A. Age-related macular degeneration. Pharmacotherapy. 2013 Aug;33(8): 838–55 24.Augustin А, Sahel JA, Bandello F, et al. Anxiety and depression prevalence rates in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2007 Apr;48(4):1498–503 25.Ord LM, Wright J, DeAngelis MM, Feehan M. Quality of Life with Macular Degeneration Is Not as Dark as It May Seem: Patients’ Perceptions of the MacDQoL Questionnaire. Clin Med. 2015 Sep 22;4(9):1841–52 26.Taylor DJ, Hobby АЕ, Binns АМ, Crabb DP. How does age-related macular degeneration affect real-world visual ability and quality of life? A systematic review. BMJ Open. 2016 Dec 2;6(12):e011504 27.Tao Y, Jiang Р, Wei Y, et al. ?-Lipoic Acid Treatment Improves Vision-Related Quality of Life in Patients with Dry Age-Related Macular Degeneration. Tohoku J Exp Med. 2016;240(3):209–214
|