J.ophthalmol.(Ukraine).2017;2:18-24.
|
https://doi.org/10.31288/oftalmolzh201721824 Typology of macular edema associated with retinal vein occlusion: variety of pathomorphological picture of the eye fundus. Part I
T.A. Romanova, Postgraduate Student
M.P. Kulbida, Junior Research Associate
Filatov Institute of Eye Diseases and Tissue Therapy
Odessa, Ukraine
E-mail: kulbidamp@gmail.com
Background. Conservative treatment of macular edema associated with retinal vein occlusion is often unable to control progression of the disease. ME chronization is observed in ?30% patients, excludes spontaneous resolution, is difficult to treat and is considered a cause of decreased visual acuity (VA). A pathomorphological picture is very variable: there are both rich and poor pathologic semiology of the eye fundus. Despite the long history of studying, this variability and its connection with VA are understudied, which increases the treatment uncertainty. The time terms and sequence of therapeutic actions, medication doses, retinal laser coagulation (LC) modes, a number of repeated interventions, long-term outcomes of the treatment are objects of multi-center randomized investigations and a subject of discussion today. One of the ways to improve the treatment of persisting ME is a search for clear criteria for patients’ differentiation and to perform treatment in regard to the state of a certain patient. This differentiating approach refers to a precise detection of ME using maximum information that can be provided by traditional and brand new examination methods.
Purpose. To assess the variety of pathologic semiology of the ocular fundus in patients with macular edema associated with retinal vein occlusion who were resistant to conservative treatment.
Material and Methods. 160 patients, of a total of 377 patients with RVO-associated ME, who were resistant to conservative treatment were observed. The patients underwent the course of conservative treatment (which was not a success) at Eye Microsurgery Centre, Kyiv, within 2009-2012; they were not performed laser coagulation (LG) of the retina; they had no other macular disorders; the optic media of the eye were transparent and artery hypertension was compensated. There were 77 men and 83 women, aged, on average, 60.7±9.2 and 62.7±11.1, respectively. The CT course was performed twice with a one-month interval and included topical and systemic vasodilators, fibrinolytics, vasoprotectives and corticosteroids. At admission to the clinic with recommendation to continue treatment using laser therapy, medical history of a patient was taken, complaints were recorded and standard general and ophthalmic examination was performed.
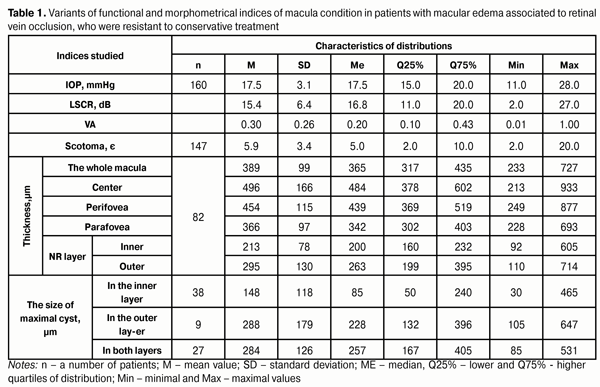
Results. In cohort of RVO-associated ME patients resistant to conservative treatment, a great variability of the parameters studied was observed: VA, 0.01-1.0; LSCR, 2-27 dB; scotoma rates, 2-20?; IOP, 11- 28 mmHg; ME thickness in the center, 249-877 µm; ME thickness in the parafovea, 228-693 µm; inner NR layer thickness, 92-605 µm; outer NR layer, 110-714 µm. Patients’ distribution was unimodal in regard of NR inner layer thickness; however, as for NR outer layer thickness, the whole cohort was divided into two subgroups with local modes of 205 и 385 µm (320 µm section). The variations of the ME thickness can explain only ? 11% of VA variations.
Conclusion. Pathomorphological picture of the disease varies a lot in ME associated with retinal vein occlusion that was resistant to concervative treatment. Significant heterogeneity of the cohort studied and differences in mutual correlation of the pathological symptoms point to the possibility of objective classification of the disease according to the pathologic symptomatology complex.
Key words: macular edema, retinal vein occlusion,ocular fundus, symptomatology Background To our best knowledge, there is no pathogenically proven treatment for macular edema (ME) associated with retinal vein occlusion (RVO) than can improve the vision or reduce visual acuity loss in the long term [6, 14]. Efforts of pathogenic surgical treatment of RVO, such as radial optic neurotomy, arteriovenous adventitial sheathotomy with a purpose to decompress the venule at the site of arteriovenous crossing with/without vitrectomy [24], have been rarely used or have not proven their clinical efficacy (including “price/quality” ratio). These efforts might have been grounded on the wrong theoretical ideas (for instance, a concept of increased intraocular pressure as a cause of RVO) [9] and are not used today [6, 16, 18]. None of the methods (conservative, laser, or surgical) for RVO-associated macular edema treatment guarantees a successful outcome. Symptomatic conservative treatment (CT) includes the course of medication therapy and aims at: 1) decongestion; 2) inflammation management (corticosteroids, nonsteroidal anti-inflammatory drugs, antioxidants); 3) angiogenesis suppression; 4) increase of perfusion of the affected vein (vasodilators, anticoagulants, thrombolytics, disaggregants); 5) reduction of ischemic consequences of RVO [2]. However, conservative treatment of RVO-associated ME is not able to stop disease progression in many cases [6]. Persisting chronic ME is observed in about a third of patients; it is hard to treat and considered to be the leading cause of visual impairment [20]. The pathomorphological picture at the initial examination of such patients varies a lot: there are cases of both rich and poor pathologic semiology of the ocular fundus. A use of maximum information that can be provided by traditional and brand new retinal examination methods appears to be optimal. The insufficiency of methods for diagnostics of ocular fundus vascular pathology such as biomicroophthalmoscopy, fundus imaging with commercial fundus cameras and fundus fluorescein angiography (FFA) is impossibility to obtain a high-spatial resolution image as well as shadowing and overlapping of images. The main result of FFA is the assessment of neovascularization and zones of retinal ischemia. However, FFA data are often concidered as old-fashioned and less informative and used in clinical practice more like as tradition demands [6]. Moreover, the ethical question on the use of this invasive diagnostic method in patients with high VA is still open [4]. The development of optical coherence tomography (OCT), both a technique and mathematical methods of data processing, has significantly broadened the possibilities for registering and measuring the state of the retina, diagnosing [1] and predicting treatment outcomes [11] in RVO-associated ME. The time terms and sequence of therapeutic actions, doses of drug administration, modes of retinal laser coagulation (LC), a number of repeated interventions, long-term outcomes of the treatment are objects of multi-center randomized investigations and a subject of discussion today [6]. The most perspective direction seems to be a combination of intravitreal or subtenon corticosteroids and inhibitors of vascular endothelial growth factor (anti VEGF-drugs) with laser coagulation (LC) of the retina. The issue of treatment of patients with central retinal vein occlusion (CRVO) is an unsolved problem of ophthalmology: in most cases, only VA stabilization can be achieved; the loss of vision and/or bad pain syndrome can force the decision of enucleation [10, 15]. Active implementation of up-to-date RVO treatment strategies determines the relevance of search for clear criteria for selection of patients, the management of which requires a multidisciplinary approach in order to identify and correct the associated risk factors [14], including potential injury during LC, toxic and side effects of physiologically highly active pharmaceutical drugs, and a treatment-related state of the retina which is hard to predict. Material and Methods 160 patients, of a total of 377 patients with RVO-associated ME, who were resistant to conservative treatment, were observed. The patients underwent the course of conservative treatment (which was not a success) at Eye Microsurgery Centre, Kyiv, within 2009-2000; they were not performed laser coagulation (LG) of the retina; they had no other macular disorders; the optic media of the eye were transparent and artery hypertension was compensated. There were 77 men and 83 women, aged, on average, 60.7±9.2 and 62.7±11.1, respectively. The principal diagnosis was made in all patients according to the type and location of the occlusion: central retinal vein occlusion (CRVO) of a nonischemic type, 34 (21%) patients; branch retinal vein occlusion (BRVO) of a nonischemic type, 71 (44%) patients; central retinal vein occlusion of an ischemic type, 19 (12%) patients; branch retinal vein occlusion of a nonischemic type, 36 (23%) patients. The CT course was performed twice with a one-month interval and included topical and systemic vasodilators, fibrinolytics, vasoprotectives and corticosteroids. At admission to the clinic with recommendation to continue treatment using laser therapy, medical history of a patient was taken, complaints were recorded and standard general and ophthalmic examination was performed. There were measured and recorded: visual acuity (VA), the light sensitivity in the central retina (LSCR), intraocular pressure (IOL), occurrence (presence/absence) and expansion (quantity and/or area) of such pathological symptoms (PS) on the ocuar fundus as ophthalmoscopically revealed macular edema, intraretinal hemorrhage (IRH), ischemic zones (IZ), vascular neoplasms (VN), microaneurysm (MA), “soft” exudates (SE), “hard” exudates (HE), and detachment of the neurosensory retina (DNS). OCT (Stratus OCT 3000) was used to measure the thickness of nine ME segments, inner and outer layers of neurosensory retina as well as the height of the detachment of the neurosensory retina and the size of the biggest cystic lesion. The data analysis was performed according to state standards and statistic analysis guidance [1, 3]. Results and Discussions Data at presentation varied significantly: VA, 0.01-1.0; LSCR, 2-27 dB; scotoma rates, 2-20?. IOP variation was weaker: 11-28 mmHg. In 142 (89%) patients, IOP rates were within reference norm intervals (9-21 mmHg), 18 patients were detected to have slightly increased IOP within 21-27 mmHg (Table 1).
Ophthalmoscopy revealed diffuse macular edema in 84% of ischemic type CRVO patients and only in 10% of patients with nonischemic type. ME was within 1 DD in 21% of patients, 2 DD in 46 %, 3 DD in 13%, and 4DD in 21% of patients. The thickness in the centre of ME varied from 213 to 933 µm (coefficient of variation CV%=33%); the perifovea and parafovea thickness ranged from 249 to 877 µm and from 228 to 693 µm, respectively, (CV%?25% for both rings) (Table 1); herewith, the consistency of thickness variations in ME center and parafovea was not high: Pearson correlation coefficient (RP) was 0.69% It should be noted that correlation was weak between VA and OCT morphometry data of ME: multiple correlation coefficient (R) between VA and all nine OCT map segments was -0.33. Thus, in the cohort of patients with RVO-associated ME, variations of the macula thickness can explain only R2 ? 11% of cases of VA variations. The sources of the rest ?89% of VA variations in the cohort studied should be searched for among other indices and factors, and, first of all, in diversity of pathologic symptoms of the ocular fundus. In cystic RVO-associated ME, which had been revealed in 141 patients – 88% of the whole cohort, VA was significantly decreased: VA = 0.20 [0.08; 0.40] in the presence of cysts and VA = 0.55 [0.40; 0.90] in the absence of cysts (a Mann-Whitney test: р<0.00001). The cysts were located in the inner layer, in the both layers, and in the outer layer of the neurosensory retina (NR) in 51%, 37 %, and 12%, respectively. The patients’ distribution according to the size of the maximal cyst was bimodal. If the cysts were noted only in the inner NR layer, they were of a relatively small size and averaged 88±31 µm. The much larger cysts with an average size of 329±104 µm were revealed in the outer NR layer, not depending on their absence or presence in the inner NR layer. The presence of the cysts in the outer NR layer was associated with a decrease of VA=0.20 (0.10; 0.30) (n=9+27=36). VA=0.30 (0.10; 0.40) (n=38). When the cysts were located only in the inner layer (Table 1), the character of the cysts’ distribution throughout the NR thickness was associated with the location of the cystic cavities in the NR layers. The mean thickness of the inner and the outer NR layers was 213±78 µm and 295±130 µm, respectively. Herewith, patients’ distribution was unimodal in regard of NR inner layer thickness; however, as for NR outer layer thickness, the whole cohort was divided into two subgroups with local modes of 205 и 385 µm (320 µm section). 70 patients (44%) had blood flow disturbances in the affected vein, which were more common for the patients with ischemic RVO. A complete blockage of blood flow in the affected vein at early stages compared to the paired vein was revealed by FFA only in BRVO: in 9 patients with ischemic BRVO and 2 patients with non-ischemic BRVO. Zones of ischemia (ZI) were revealed in 128 (80%) patients, of them: 41 patients (32% of all ZI cases) ?3 DD; 30 (23%) =4-6 DD; 44 (34%) = 7-10 DD and 13 patients (10%) >10 DD. Detachment of NR was revealed in 25% of patients. The presence of NR detachment was associated with a decrease in VA: VA averaged ?0.1 and 0.3 in the presence and the absence of NR detachment, respectively. The distribution of the patients in regard of the height of NR detachment was clearly bimodal with modes of 75 and 275 µm (225 µm section). Herewith, NR detachment, engaging the center of the macula, was six times more often against the ischemic type as compared to the non-ischemic type of ME associated to RVO, 18% and 3%, respectively. At presentation, all patients were revealed IRH in the ocular fundus: single IRH in 63 (39%) and throughout all four sectors of the macula in 9 (6%) patients. Microaneurysms (MA) were revealed in 62 (39%) patients with hemorrhages, of them, MAs were single in 50 patients (81%). MAs were 1.9 times more often in the patients with occlusion of the non-ischemic type than in those with the ischemic type occlusion, 65% vs. 35%, and ?2 times more often in the occurrence of BRVO than of RVO, 67% vs. 33%. The occurrence difference was significant in both cases (Fisher's z-test: р<0.01). Vascular neoplasms (VN) were revealed in 31 (19%) patients. Single VNs were in three patients (10%); VNs were 1 DD and > 1 DD in 21(68%) and 10 (22%) patients, respectively. Soft exudates (SE) were noted in 89 patients (56%), of them: 1-3 focuses of ?1 DD were revealed in 54 patients (61% of all SE cases); SEs of 2-4 DD and ?5 DD were in 27 and 8 cases. The number of focuses and SE area were closely related to each other: Spearman's rank correlation coefficient Rs = 0.63 (n=16) in CRVO of the ischemic type; Rs = 0.83 (n=25) in BRVO of the ischemic type; Rs = 0.45 (n=28) in BRVO of the non-ischemic type; р<0.003 for all coefficients. However, this relation did not occur in CRVO of the non-ischemic type, Rs = 0,002 (n=17). Hard exudates (HE) were noted in 21 (13%) patients: single HEs were in 14 patients; five patients had HE in one sector; and only one patient had HE in all four sectors of the macula. A large variety of pathological symptoms of the ocular fundus in the patients with ME associated with RVO makes it more difficult to come to a therapeutic decision of the individual approach to LC. The most common and, in fact, tautological explanation of the diversity in conditions of patients, admitted for LC treatment, is characteristics of changes in the development of the disease in every certain case. The variety of changes can be due to the deeper cause: ethiopathogenetic heterogeneity of a “retinal vein occlusion” nosological entity, under which there can be hidden several diseases of various ethiopathogenesis. This idea has been represented by Hayreh [8] when pathologic symptom elimination rates in CRVO and BRVO have been compared. It should be noted that selection a cohort of patients with ME, who were resistant to conservative treatment, as a subject of investigation facilitates verifying the hypothesis of S. Hayreh [8] since this excludes cases of edema spontaneous resolution. As we determined before, diffuse macular edema is more likely to develop in the patients with ischemic RVO, which can also point to the difference in development mechanisms of RVO-associated ME. It is consistent with S. Scholl’s idea [20] that diffuse ME is caused by general diffuse leakage through widened retinal capillaries (MAs and arterioles); and local edema development is associated only with fluid leakage through MAs. Indeed, retinal arteriole closing can lead to formation of a big area of its nonperfusion and progression of retinal ischemia. Vision loss is a common evidence of foveal avascular zone widening >1000 µm [20]. Also, according to our data, a significant decrease of initial VA (at average, three times) is connected with the presence of detachment of neurosensory part of the macula, which is confirmed by other authors [19]. MAs in non-ischemic patients with occlusion are 1.9 times more often than those of the ischemic type, 65% vs. 35%, and 2 times more often in BRVO than in CRVO, 67% vs. 33%, which can point to etiological differences. According to Tomiyasu et al. [23], MAs are the cause of refractory ME development and laser coagulation of the retina can serve as an effective additional treatment in such patients since anti-VEGF intravitreal injections do not influence on MAs and can only prevent from them [23]. The role of MAs in ME development can be revised since multimodal angio-OCT imaging of microvascular abnormalities exceeds FFA possibilities [22]. A significant VA decrease in the patients with cystic ME is associated with the fact that edema plays a leading role in photoreceptor degeneration and nervous cell death. ME development is considered to be preceded by development of Muller cell (ganglion cell) edema, which develops even before the occurrence of extracellular edema. When ME is transformed in a cystic form, cysts, morphologically, are made of swelled and dying Muller cells. Thus, extracellular edema is preceded by intracellular edema development [20]. The relationship between the blood flow reduction in the deep retinal capillary plexus and the cystic cavities is well known. Similarity of ME development with cerebral edema development in insults makes it possible to suppose that the Muller cells, like brain astrocytes, can transport excess fluid from the retina to the vascular blood flow [21]. Despite the fact that OCT is widespread as a non-invasive method of retinal examination and the angio-OCT ha appeared, the role of FFA is very important for performing retinal LC. Some authors have reported that if a practician is guided by only OCT findings, he makes a lot of laser coagulates in the retina, and when FFA is used, the treatment is more selective and preserving with a less number of laser coagulates [12]. Thus, a treatment plan should be based on the information obtained in both methods of the retinal examination and OCT findings should be interpreted together with fundus ophthalmoscopy and FFA findings. Indeed, the nature of the same factor, "an increased ME thickness according to OCT", can be different. For instance, if a patient has pronounced symptoms of ischemia and IRH, than, more likely, the increased ME thickness according to OCT is caused by uptake of the blood and fluid in the inner retinal layers due to capillary perfusion disorders. If a patient has symptoms-markers of adaptation of the retinal vessels to altered blood circulation conditions, such as MAs and other microvascular abnormalities, than, more likely, the cause of ME in the tissues is fluid leakage from defected walls of these vessels. If a patient has vascular neoplasms and an increased number of hard exudates, than, likely, these VNs are the source of fluid uptake in the retinal layers. Apparently, treatment approaches in these various cases, which are sometimes indistinguishable in regard of ME thickness, can vary; however, this remains unknown [6, 7]. Terms and sequence of therapeutic actions performed, intake drug dosage, a number of repeat interventions, remote results of one or another RVO-associated ME treatment algorithm are still a matter of discussion today [6]. Many authors do not connect RVO-associated ME with the pathological symptoms of the ocular fundus, which, to our opinion, is a result of high variability in the individual pathomorphological picture of ME associated with RVO. The analysis of pathological symptoms and its relations with VA requires a large number of patients, which is available only in multi-center randomized investigations [6, 13]. These investigations have shown that the same symptoms are revealed in diabetic maculopathy and they are clearly associated with diabetic macular edema [17]. Conclusions When RVO-associated MA is resistant to conservative treatment, variability in the pathomorphological picture of the disease is observed. Significant heterogeneity of the cohort studied and differences in mutual correlation of the pathological symptoms point to the possibility of objective disease classification according to the pathologic symptomatology complex.
References 1. ISO 5479:1997, IDT. Statistical interpretation of data - Tests for departure from the normal distribution 2. [Protocol of medical care for patients with central retinal vein occlusion and branch retinal vein occlusion. Order of MoH of Ukraine from 15.03.2007 No 117]. 3. Rebrova ОY. [Statistical analysis of medical data. Usage of the package of application programs STATISTICA]. M.: Media Sphera. 2002:312. Russian. 4. Rodin AS. [New Clinical possibilities of optical coherence tomography. Early diagnostics of pathology of the macula in patients with high vision acuity]. Oftal’mologiya. 2004; 4:24-8. Russian. 5. Al Faran А, Mousa A., Al Shamsi H et al. Spectral domain optical coherence tomography predictors of visual outcome in diabetic cystoid macular edema after bevacizumab injection. 2014;34(6):1208-15. 6. Browning DJ. Retinal vein occlusion. Evidence-based Management. Science; 2012. 387 p. 7. Ford JA, Clar C, Lois N et al. Treatments for macular oedema following central retinal vein occlusion: systematic review. BMJ Open 2014;4:e 004120. 8. Hayreh SS, Zimmerman MB. Fundus changes in branch retinal vein occlusion. Retina. January 2015;35(1):29-42 and May 2015;35(5):1016-027. 9. Hayreh SS, Zimmerman MB, Podhajsky P.A. Retinal vein occlusion and the optic disk. Retina. 2012 Nov-Dec;32(10):2108-18. 10.Kiire CA, Chong NV. Managing retinal vein occlusion. BMJ 2012;344:e499. 11.Ko J, Kwon O, Byeon S. Optical coherence tomography predicts visual outcome in acute central retinal vein occlusion. Retina: June 2014;34(6):1132-1141. 12.Kozak I, El-Emam SY, Cheng L et al. Fluorescein angiography versus optical coherence tomography-guided planning for macular laser photocoagulation in diabetic macular edema. Retina. August 2014;34(8):1600-5. 13.Lam FC, Chia SN, Lee RM. Macular grid laser photocoagulation for branch retinal vein occlusion. Cochrane Database Syst Rev. 2015 May 11;(5):CD008732. doi: 10.1002/14651858.CD008732.pub2. 14.Lattanzio R, Torres AG, Parodi MB et al. Retinal Vein Occlusion: Current Treatment. Ophthalmologica. 2011;225:135–143. 15.McIntosh RL, Rogers SL, Lim L et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology.2010;117:1113–23. 16.Mohamed Q, McIntosh RL, Saw S et al. Interventions for central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2007;114:507–19. 17.Muraoka Y, Tsujikawa A, Yoshimura N. Association between retinal hemorrhagic pattern and macular perfusion status in eyes with acute branch retinal vein occlusion. Scientific Re-ports. 2016;6:28554. 18.Niral K. Retinal vein occlusion: pathophysiology and treatment options. Clinical Ophthalmology.2010;4:809-16. 19.Noma H, Funatsu H, Mimura T, Shimada K. Visual function and serous retinal detachment in patients with branch retinal vein occlusion and macular edema: a case series.BMC Ophthalmol. 2011;11:29. 20.Scholl S, Kirchhof J, Augustin AJ. Pathophysiology of macular edema. Ophthalmologica. 2010; 224 Suppl 1:8-15. Epub 2010 Aug. 21.Spaide RF. Retinal vascular cystoid macular edema: Review and new theory. Retina. Oct 2016;36(10):1823-42. 22.Suzuki N, Hirano Y, Yoshida M et. al. Microvascular abnormalities on optical coherence tomography angiography in macular edema associated with branch retinal vein occlusion. Am. J. Ophthalmol. Jan 2016;161;126-32. 23.Tomiyasu T, Hirano Y, Yoshida M et al. Microaneurysms cause refractory macular edema in branch retinal vein occlusion. Sci Rep. Jul 2016; 8(6):29445. 24.Yamamoto S, Saito W, Yagi F et al. Vitrectomy with or without arteriovenous adventitial sheathotomy for macular edema associated with branch retinal vein occlusion. Am. J. Ophthalmol. 2004;138(6):907-14.
|