J.ophthalmol.(Ukraine).2017;2:12-17.
|
https://doi.org/10.31288/oftalmolzh201721217 Phenotypic markers of syndrome of unspecified connective tissue dysplasia in children with acquired myopia
T.E. Tsybulskaya, Cand Sc (Med) N.E. Zavgorodnyaya, Dr Sc (Med), Prof. E.E. Pashkova, Dr Sc (Med) Zaporizhzhia State Medical University Zaporizhzhia, Ukraine E-mail: tamila.72@mail.ru
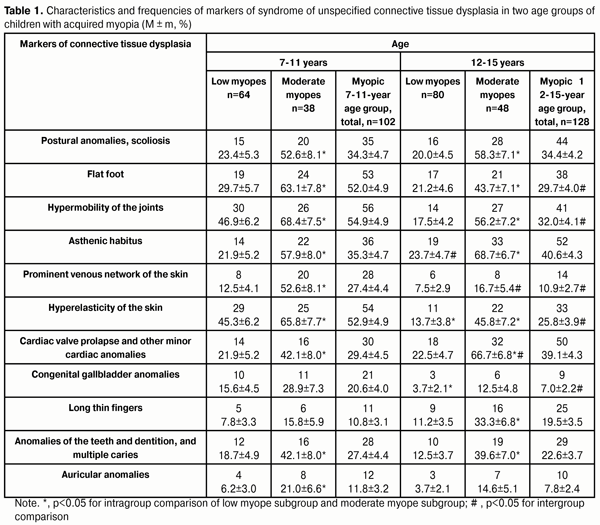
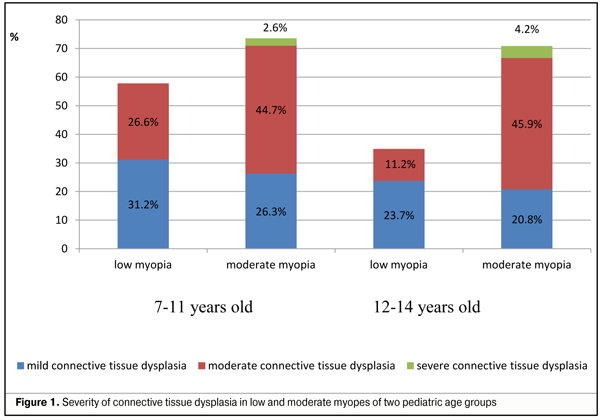
Background: Myopia can be caused by structural and functional alterations in the connective tissue. Purpose: To evaluate the phenotypic markers of the syndrome of unspecified connective tissue dysplasia (SUCTD) in a cohort of children with acquired myopia. Materials and Methods: Two hundred and thirty 7-15-year-old children with acquired myopia of low or moderate degree were involved in the study. They were divided into two age groups, junior (7-11 years; 102 individuals) and senior school children (12-15 years; 128 individuals). Odds ratios (OR) and 95% confidence intervals (CI) were used to assess the risk of myopia progression. Results: The major phenotypic risk factors for developing moderate myopia in children of 7-11 years were prominent venous network of the skin (OR, 7.8; 95% CI, 2.9-20.7; p < 0.05), asthenic habitus (OR, 4.9; 95% CI, 2.1-11.8; p < 0.05), and flat foot (OR, 4.0; 95% CI, 1.7-9.5; p < 0.05), whereas in children of 12-15 years, these factors were moderate or severe connective tissue dysplasia (OR, 7.9; 95% CI, 3.2-19.3; p < 0.05), asthenic habitus (OR, 7.1; 95% CI, 3.2-15.7), cardiac valve prolapse and other minor cardiac anomalies (OR, 6.9; 95% CI, 3.1-15.3; p < 0.05), hypermobility of the joints (OR, 6.1; 95% CI, 2.7-13.6; p < 0.05), postural anomalies and scoliosis (OR, 5.6; 95% CI, 2.5-12.4; p < 0.05), and hyperelasticity of the skin (OR, 5.3; 95% CI, 2.3-12.5; p < 0.05). Conclusions: Low myopic children with a moderate or severe connective tissue dysplasia are at risk for developing moderate myopia. The major SUCTD-related risk factors for developing moderate myopia in children of 7-11 years were prominent venous network of the skin, asthenic habitus, and flat foot, whereas in children of 12-15 years, these factors were asthenic habitus, cardiac valve prolapse and other minor cardiac anomalies, hypermobility of the joints, postural anomalies and scoliosis, and hyperelasticity of the skin. Key words: children, myopia, connective tissue dysplasia Introduction Myopia is one of the most common ocular disorders in pediatric population. Although multiple myopia studies have been performed, the disease is still an important subject for research by practitioners. The progressive course of the disease leads to the development of fundus complications and visual incapacitation in young adults, and is a matter of special concern for ophthalmologists [1-3]. Recently, myopia has been increasingly considered as an interdisciplinary and multifactorial disease, with optimum management requiring the input of several medical specialties (first and foremost, pediatrics) [2, 4, 6]. Therefore, longitudinal monitoring of pediatric myopia progression not only should include assessment of visual and optical functions of the eye, but it should take into consideration the premorbid somatic status of the child. Studies of the pathogenesis of myopia have provided evidence that changes in the sclera, a connective tissue that forms the outer coat of the eye, are often a major contributor to the progression of the disease [1, 2]. In the pediatric patient, these changes can be caused by structural and functional alterations in the connective tissue. According to epidemiological data, 13% to 53% of the pediatric population of Ukraine has phenotypic signs of connective tissue weakness which cannot be categorized as phenotypic manifestations of any of the specified syndromes and should be categorized as manifestations of the syndrome of unspecified connective tissue dysplasia (SUCTD) [7]. It has been reported in recent years that SUCTD is a potential risk factor for developing various diseases, including myopia [4, 6, 7]. Given the high prevalence of myopia and the growing incidence of pediatric myopia worldwide, the issue requires a thorough analysis. The purpose of the study was to evaluate the phenotypic markers of unspecified connective tissue dysplasia in children with acquired myopia and their role in the progression of the disease. Materials and Methods Two hundred and thirty 7-15-year-old children with acquired myopia of low or moderate degree (as per the classification of Avetisov (1968)) were involved into the study. They were divided into two age groups, junior (7-11 years; 102 individuals) and senior school children (12-15 years; 128 individuals), as per the modified age-period classification of Mazurin and Vorontsov (1999). The phenotypic markers of SUCTD were identified through history, medical records and physical examination, and based on specialty opinion (from pediatrics, orthopedics, otorhinolaryngology, and neuropathology). The severity of SUCTD was graded as per the grading system proposed by Milkovska-Dimitrova and Karkashev [3, 8, 9]. The major criteria (hypermobility of the joints, hyperelasticity of the skin, chest and spinal deformities, ocular disorder, high palate, long thin fingers, flat foot and prominent venous network of the skin) and minor criteria (anomalies of the auricles, teeth, dentition, intermittent joint pain, joint dislocation, joint subluxation, webbing between fingers, etc) were used for grading. The severity of SUCTD was graded as mild (Grade I) if two of the major criteria were present, moderate (Grade II) if either 3 of the major criteria and 2-3 of the minor criteria, or 3-4 of the major criteria and 2-3 of the minor criteria were present, and severe (Grade III) if 5 of the major criteria and 3 of the minor criteria were present. Pediatric patients underwent ophthalmological examination including visual acuity, biomicroscopy, ophthalmoscopy and axial eye measurements. In addition, autorefractometry and keratometry were performed under cycloplegia. Statistical analysis was performed using Microsoft Excel and STATISTICA 10.0 software. Mean (M), root-mean-square deviation (?), and mean error (m) values were calculated. Student’s t test was used to assess intergroup differences. Differences were considered significant at the level of p < 0.05. Odds ratios (OR) and 95% confidence intervals (CI) were used to evaluate the risk of developing moderate myopia. The factors with OR greater than 1.0 were selected as meaningful indicators. Results and Discussion The phenotypic markers of SUCTD were identified in 127 (55.2±3.3%) out of 230 study children examined. In particular, they were identified in 65 (63.7%; 37 low myopes (57±6.1%) and 28 moderate myopes (43±6.1%)) out of 102 junior school children and in 62 (48.4%; 28 low myopes (45.2±6.3%) and 34 moderate myopes (54.8±6.3%)) out of 128 senior school children examined. Table 1 shows the most commonly identified phenotypic markers of SUCTD. As can be seen from the data presented in the table, the two age groups were somewhat different from one another in terms of the frequency and nature of manifestations of these markers. In both groups, locomotion alterations (postural anomalies, scoliosis, flat foot and joint hypermobility) were the most commonly identified phenotypic manifestations of SUCTD. However, postural anomalies and scoliosis were found at the same frequency in junior and senior children, whereas flat foot and joint hypermobility were found 1.7-fold more often in the former children (p < 0.05). Prominent venous network and hyperelasticity of the skin were 4.8-fold and 2.0-fold, respectively, more common among junior children than senior children (p < 0.05). Visceral manifestations of SUCTD (such as congenital gallbladder anomalies in the form of folded or strangulated gallbladder) were found 2.9-fold more often in junior than in senior children (20.6 ± 4.0% vs 7.0±2.2%, p < 0.05). At the same time, asthenic habitus, long and thin fingers, cardiac valve prolapse and other minor cardiac anomalies were more common among senior children; however, this difference was not statistically significant. Such phenotypic markers as anomalies of the teeth, dentition, and multiple caries, and auricular anomalies, were equally distributed among both age groups. Of note is that the markers of SUCTD were most common in children with moderate myopia. Interestingly that moderate SUCTD was found 2.4-fold more often in junior children with low myopia than in senior children with low myopia (26.6±5.5% vs 11.2±3.5%; p < 0.05); this can be considered as an evidence of the progression of myopia with age in children with SUCTD (Fig. 1). Therefore, subsequently, we analyzed the frequency of the phenotypic markers of SUCTD in children of both age groups depending on the severity of myopia (Table 1).
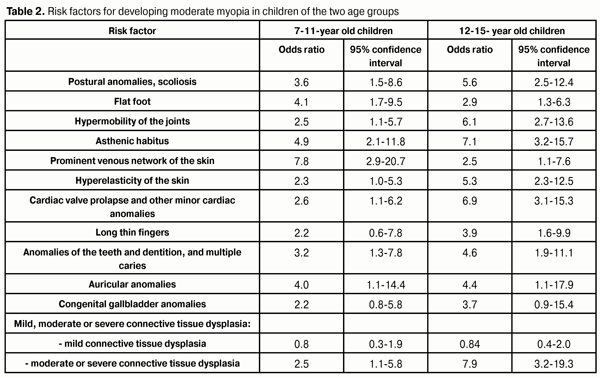
In junior moderate myopes, dysplasia of the skeleton, skin and cardiovascular system were more common than in junior low myopes (p < 0.05). A similar relationship was noted for the senior schoolchildren group. However, there were differences among moderate myopes of the age groups for the rates of cardiac manifestations of connective tissue dysplasia. Thus, prominent venous network of the skin was 3.1-fold more common among junior moderate myopes than among older moderate myopes, whereas cardiac valve prolapse and other minor cardiac anomalies were statistically significantly more common among the latter than among the former (66.7±6.8% vs 42.1±8.0%; p < 0.05). Current biochemical and molecular genetic analysis techniques allow investigators to assess individuals for their connective tissue status, to prognose the course of their disease, and to develop treatment techniques for the disease. Although oxoproline and glycosaminoglycan levels in daily urine, and lysine, proline, and oxoproline levels in plasma are informative for this purpose [3], many investigators note that such assays are labor intensive, require expensive equipment, and take much time. Therefore, clinical-and-anamnestic as well as functional examination approaches are the best available option [3, 8, 9]. They are acceptable for the ophthalmologist; in addition, they allow him or her to diagnose SUCTD in time and to develop treatment measures as early as at the physical examination phase of pediatric patient assessment. In this connection, we analyzed the risk of developing moderate myopia in children depending on phenotypic manifestations of SUCTD and on age (Table 2). The major risk factors for developing moderate myopia in children of 7-11 years were prominent venous network of the skin (OR, 7.8; 95% CI, 2.9-20.7; p < 0.05), asthenic habitus (OR, 4.9; 95% CI, 2.1-11.8; p < 0.05), and flat foot (OR, 4.0; 95% CI, 1.7-9.5; p < 0.05). Postural anomalies in scoliosis (OR, 3.6; 95% CI, 1.,5-8.6; p < 0.05) and anomalies of the teeth, dentition, and multiple caries (OR, 3.2; 95% CI, 1.3-7.8; p < 0.05) were less important contributors to the risk for developing moderate myopia in children of this age. Minor cardiac anomalies, hypermobility of the joints, hyperelasticity of the skin, long thin fingers, congenital gallbladder anomalies, and presence of moderate or severe connective tissue dysplasia were only minor contributors to the risk.
At the same time, the presence of moderate or severe connective tissue dysplasia (OR, 7.9; 95% CI, 3.2-19.3; p < 0.05) was highly informative for the risk of developing moderate myopia in children of 12-15 years. Other important risk factors of note were asthenic habitus (OR, 7.1; 95% CI, 3.2-15.7), cardiac valve prolapse and other minor cardiac anomalies (OR, 6.9; 95% CI, 3.1-15.3; p < 0.05), hypermobility of the joints (OR, 6.1; 95% CI, 2.7-13.6; p < 0.05), postural anomalies and scoliosis (OR, 5.6; 95% CI, 2.5-12.4; p < 0.05), and hyperelasticity of the skin (OR, 5.3; 95% CI, 2.3-12.5; p < 0.05). Anomalies of the teeth, dentition and multiple caries (OR, 4.6; 95% CI, 1.9-11.1; p < 0.05), auricular anomalies (OR, 4.4; 95% CI, 1.1-17.9; p < 0.05), long thin fingers (OR, 3.9; 95% CI, 1.6-9.9; p < 0.05) and congenital gallbladder anomalies (OR, 3.7; 95% CI, 0.9-15.4; p < 0.05) also contributed to the risk of developing moderate myopia in senior school children. Contributions of flat foot (OR, 2.9; 95% CI, 1.3-6.3; p < 0.05) and prominent venous network of the skin (OR, 2.5; 95% CI, 1.1-7.6; p < 0.05) to the risk of developing moderate myopia in senior school children were minor and less than those to the risk of developing moderate myopia in junior school children. There was a significant percentage (55.2±3.3%) of individuals with phenotypic manifestations of SUCTD, and we identified a variety of phenotypic markers of SUCTD in the pediatric population under study. Therefore, the presence of myopia in the child should indicate the need for screening for these markers during annual ophthalmological examinations. Even junior children with low myopia were found to have a variety of phenotypic markers of SUCTD, which can have a negative impact on the progression of myopia and result in the development of high refractive errors. Thus, history analysis revealed that 82 ± 8.2% of senior schoolchildren with moderate myopia had initial manifestations of the disease at the age of 7-9 years, whereas 76.2±9.2 % of senior schoolchildren with low myopia had these manifestations at the age of 12-13 years. The presence of moderate or severe connective tissue dysplasia in the low myopic pediatric patient contributes to the increased risk of developing moderate myopia, which this should be taken into consideration when examining such patients. Conclusions First, flat foot, hypermobility of the joints, hyperelasticity of the skin, postural anomalies and scoliosis, and asthenic habitus were the most common phenotypic markers of SUCTD in 7-11-year-old patients with acquired myopia. Second, asthenic habitus, cardiac valve prolapse and other minor cardiac anomalies, and postural anomalies and scoliosis were the most common phenotypic markers of SUCTD in 12-15-year-old patients with acquired myopia. Third, children with moderate or severe connective tissue dysplasia are at risk for the development of moderate myopia, which should be taken into consideration when initially examining a pediatric patient. Finally, prominent venous network of the skin, asthenic habitus and flat foot are the main risk factors for the development of moderate myopia associated with connective tissue dysplasia in 7-11-year-old patients with acquired myopia, whereas asthenic habitus, cardiac valve prolapse and other minor cardiac anomalies, hypermobility of the joints, postural anomalies and scoliosis, and hyperelasticity of the skin are the main risk factors for the development of the disease in 12-15-year-old patients with acquired myopia. The visual system features and prognosing the developmental time course of myopic refraction error in the children with phenotypic markers of SUCTD will be subjects of further investigations. Another subject will be whether it is reasonable to include the treatment measures with consideration of connective tissue status in the treatment schedule of this category of patients.
References 1. Avetisov SE. [Myopia]. Moscow: Meditsina; 2002 Russian 2. Bushueva NN. [Current aspects of the pathogenesis and treatment of progressive myopia]. In: [Proceedings of the Ukrainian National Conference of Pediatric Ophthalmology]. 4-5 October, 2012, Sevastopol. p.281-91 3. Pasyechnikova NV, Rykov SA, Naumenko Liu, Kryzhanovskaia TV. [Prevention of Blindness and Visual Impairment in Ukraine: Current Status and Issues]. In: [Proceedings of the 12th Ukrainian National Congress of Ophthalmology]. 26-28 October, 2010, Odesa. p.303-4 4. Kadurina TI, Gorbunova VN, editors. [Displasia of the Connective Tissue]. St Petersburg: ELBI; 2009 Russian 5. Kadurina TI, Abbakumova LN. [Assessment of the severity of unspecified dysplasia of the connective tissue in children]. Med Vestnik Severnogo Kavkaza. 2008 May; 2:15-21 Russian 6. Chetyz RR. [Role of extraocular pathology in the pathogenesis of myopia in children and irs complex treatment]. [Cand Sc (Med) Thesis]. Moscow: Helmholtz Research Institute for Eye Diseases; 2007. 25 p. Russian 7. Lezhenko GO, Volosovets OP, Kryvopustov SP, et al. [Syndrome of unspecified dysplasia of the connective tissue in children (prevalence, diagnostic features and treatment)]. Zaporizhzhia: Zaporizhzhia State Medical University; 2006 Ukrainian 8. Ul’ianova NA. [High axial myopia: pathogenesis, diagnostics, prevention]. [Dr Sc (Med) Dissertation Abstract]. Odesa: Filatov Institute of Eye Disease; 2015. 32 p. Ukrainian 9. Carter C, Wilkinson J. Persistent joint laxity and congenital dislocation of the hip. J Bone Joint Surg Br. 1964 Feb;46:40-5
|