J.ophthalmol.(Ukraine).2017;2:70-73.
|
https://doi.org/10.31288/oftalmolzh201727073 A Case Report of Takayasu’s Arteritis O.O. Andrushkova T.M. Zhmud N.B. Malachkova K.Iu. Grizhimalskaia D.A. Iatsenko Pirogov Vinnytsia Medical University Vinnytsia, Ukraine E-mail: Gtatyana@email.ua
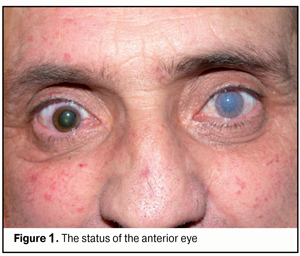
Background: Takayasu’s arteritis is a non-specific autoimmune disease affecting large-size blood vessels, with a predilection for the aorta and its major branches. The most characteristic symptoms include absence or decrease of arterial pulses in the arms and CNS-related abnormalities (arm numbness, pain and paresthesia; fatigue; dizziness; syncope; seizures; aphasia; and hemipareses). Purpose: To exemplify the ocular manifestations of Takayasu disease. Materials and Methods: The patient underwent general clinical tests, comprehensive ophthalmological examination, duplex Doppler sonography of carotid and cerebral vessels, and brain MRI. Results and Conclusion: Our case report demonstrates the severity of the course of the disease and that the prognosis for vision and life in patients with Takayasu's arteritis can be unfavorable. Takayasu's arteritis can be seen in young men, with one of the symptoms being ocular alterations (corneal edema, mydriatic pupil, cataract, changes in retinal vessel caliber, retinal edema and ischemia, and reduced blood flow velocity in the ophthalmic artery). Key words: Takayasu’s arteritis, aorto-arteritis Introduction Takayasu disease (or non-specific aorto-arteritis, or Takayasu's arteritis (TA)) is a non-specific autoimmune disease affecting large-size blood vessels, with a predilection for the aorta and its major branches. Takayasu was the first to report cases of the disease in 1908 and coined the term “non-specific aorto-arteritis”. The incidence of TA has been reported to be 2.4/million/year [1], with a predominance in women (especially under 40 years of age), and has tended to increase in recent years. The etiology of TA is still not fully understood. Previously, the disease was believed to have been caused by bacillus Kochii, and was identified in patients with different forms of tuberculosis. Subsequently, it was hypothesized that rheumatoid arthritis has a role in the development of the disease. Currently, it is believed that TA is an autoimmune disease that develops as a result of changes in the body response to different external and internal stimuli, and of contact with domestic and professional allergens, with a subsequent injury to major arteries. Panarteriitis is characterized by infiltration with dendritic cells, T cells, natural killers and macrophages. Chronic vascular inflammation leads to vessel stenosis, thrombosis and aneurysms. The late phases of the disease are characterized by intimal proliferation, and by increased risk of atherosclerosis, necrosis, focal cicatrization and adventitial fibrosis. The pathomorphological picture corresponds to that in systemic autoimmune connective tissue disorders. The morphological picture of aorto-arteritis depends on the stage of the disease (i.e., varies from acute inflammation phase to scarring). Based on the location of the involved arteries, TA is divided into Type I (involving the aortic arch and its branches), Type II (involving thoracoabdominal aorta and its branches), Type III involving the entire aorta, and Type IV involving pulmonary artery with any of the other types. Unlike the other systemic vasculitides, TA is not characterized by the development of fibrotic necrosis. Narrowing of the coronary arteries in TA usually occurs at origins, often with damage to the left major coronary artery. Stenoses develop in pulmonary arteries, and some of these vessels may show recanalization. Post-inflammatory sclerosis of the aortic intima results in the development of severe secondary atherosclerosis. Clinical picture The most characteristic symptoms include absence or decrease of arterial pulses in the arms and CNS-related abnormalities (arm numbness, pain and paresthesia; fatigue; dizziness; syncope; seizures; aphasia; hemipareses). The ocular symptoms occur when supra-aortal arteries are involved, and ocular symptomatology may be the most prominent. Patients complain of ocular pain and gradual worsening of vision. Fundus examination usually reveals uneven narrowing of the arteries, widening of the veins, retinal edema, thrombosis of individual retinal vein branches, and hemorrhages. Arterio-venous anastomosis and neovascularization are sometimes observed. The late stage is characterized by the development of proliferative retinitis. The possible alterations in the anterior eye include corneal degeneration and cataract. Narrowing of the palpebral fissure and ptosis are sometimes noted. Treatment Corticosteroids (prednisolone) are the mainstay of anti-inflammatory treatment. Patients not responding to corticosteroids can be treated with immunomodulators, including methrotrexate, cyclosporine, cyclophosphamide and azathioprine (imuran). Regular blood pressure monitoring is important since patients treated for TA are at increased risk for the development of hypertension. Prognosis The patient’s condition usually remains satisfactory for long due to the development of collateral circulation. The prognosis is worsened if, besides the aorta, the retina is also affected, and aneurysm develops. Stroke, myocardial infarction and rupture of an aortic aneurysm are the main causes of death in TA patients. To the best of our knowledge, there are few reports in the national medical literature regarding the ocular manifestations of Takayasu disease. Therefore, the aim of this case report was to exemplify the ocular manifestations of Takayasu disease. Materials and Methods Mr M, a 46-year-old man, presented at the emergency room of the Regional Ocular Trauma Center with complaints of sudden severe intolerable pain in both eyes, redness of eyes and loss of vision. Nine years before, he had been diagnosed with Takayasu disease, for which he had undergone amputation of both legs at mid-thigh. The patient underwent general clinical tests, visual acuity assessment, tonometry, ophthalmoscopy, biomicroscopy, perimetry, and anterior eye photography. In addition, he was referred to vascular surgeon, hematologist, rheumatologist, and neurologist, and underwent brain MRI and duplex Doppler sonography of carotid and cerebral vessels with APLIO 300 apparatus (Toshiba Medical Systems, Otawara, Tochigi, Japan). Results of observation Mr M, a 46-year-old man, presented at the emergency room of the Regional ocular trauma center with complaints of sudden severe intolerable pain in both eyes, redness of eyes and loss of vision. He had been diagnosed with TA, occlusion of the upper arm arteries, and right carotid artery stenosis in 2000, and underwent amputation of his legs in 2007 and in 2008. On examination, condition was fair, consciousness was disturbed, with forced body position in bed. In addition, skin was moist, and lung auscultation revealed vesicular respiration. With regard to his heart system, radial pulses were absent bilaterally, sounds were obtuse, blood pressure was 110/70 mm Hg, and diastolic murmur could be heard over aortic area. The abdomen was painless and soft on palpation. Examination of the legs revealed mid-thigh amputation stumps. Status oculorum OD: The visual acuity (VA) OD was counting fingers near face and OD intraocular pressure (IOP) was 13 mm Hg. No periorbital lesions were present, and the palpebral fissure width was normal. The bulbar conjunctival veins were dilated and tortuous and the cornea was clear. The anterior chamber was moderately deep, and was filled with clear aqueous humor. In addition, mydriatic pupil and central lens opacity were observed. Fundus examination revealed a pale optic disc with clearly defined margins, exceedingly narrow arteries and widened veins. OS: The VA OS was perception of light with inaccurate projection and OS IOP was 13 mm Hg. No periorbital lesions were present, the palpebral fissure was narrow, and injection of conjunctival vessels, injection of the eyelid and injection of the globe were observed. The cornea was edematous, dull, and had a mosaic pattern. A mydriatic pupil was noted. The fundus was not visible by ophthalmoscopy (Fig. 1).
Findings of auxiliary clinical examinations: Complete blood count and urine examination were normal. The Duke's bleeding time was normal (210 s). EEG: the principal rhythm was sinus; heart rate, 62/min; no axis deviation; left ventricular hypertrophy. Findings of duplex Doppler sonography of carotid and cerebral vessels: The blood flow velocity in ophthalmic artery was substantially reduced on both sides. In addition, the size of the common carotid arteries was within the normal range, and the sonograms of common carotid arteries showed marked thickening (due to calcification) with inhomogeneous echogenicity. Multiple atherosclerotic plaques were visible in the right common and right internal carotid arteries. The blood flow velocity in the distal portion of the right internal carotid artery was reduced (distal stenosis). The diameter of the left vertebral artery was 3.4 mm, and there was no blood flow detected in the artery. The blood flow velocity in the internal carotid artery and in the right vertebral artery was reduced. The opinion formulated based on ultrasonography was as follows: ultrasonographic evidence of atherosclerotic disease involving brachiocerebral vessels. Brain MRI findings: A series of axial, saggital and frontal brain MRI images demonstrated no displacement of midline structures, no enlargement of the ventricular system, no changes in chiasmatic-sellar region, multiple intensive periventricular and subcortical foci, no changes in craniovertebral ligaments and in orbital coni, and free paranasal sinuses. Magnetic resonance angiography (MRA) demonstrated a poor vascular pattern, markedly reduced signal from the right carotid artery, elongated vertebral arteries, and reduced signal from the vertebral and communication arteries (more substantially, on the left). The opinion formulated based on brain MRI/MRA was as follows: discirculatory encephalopathy with marked manifestations of vertebrobasilar insufficiency (Fig. 2).
Vascular surgeon’s opinion: non-specific aorto-arteritis, occlusion of the upper arm arteries, right carotid artery stenosis, and discirculatory encephalopathy. Neurologist’s opinion: chronic cerebral ischemia grade 2 and discirculatory encephalopathy grade 2. Hematologist’s opinion: there was no clinical or hematological evidence of any disorder of the blood system. The following treatment regimen was agreed with the consulting specialists and included indirect anticoagulants, anti-ischemic agents, anti-inflammatory agents, and circulation enhancers: Diclofenac Sodium, i.m., once-daily for 5 days; Actovegin, i.v., once-daily for 10 days; Trental, i.m., once-daily for 5 days; Syncumar, half a tablet, once-daily; and Aspirin Cardio, 1 tablet, once-daily. In addition, topical treatment included dexamethasone 0.4%, subconjunctival injection, 0.5 ml, once-daily; dexamethasone 0.1%, 1 drop, four-times daily (QID); Cornergel, 1 drop, QID; glucose 20%, 1 drop, QID. The treatment resulted in relief of pain, reduction in conjunctival injection, and restoration of corneal clarity. However, due to blood flow abnormalities in the left eye, VA OS remained light perception. No changes in the right eye were observed. Subsequently, there was cataract progression in the right eye. Unfortunately, at 12 months of observation, the patient died from myocardial infarction. Conclusion Takayasu's arteritis can be seen in young men, with one of the symptoms being ocular alterations (corneal edema, mydriatic pupil, cataract, changes in retinal vessel caliber, retinal edema and ischemia, and reduced blood flow velocity in the ophthalmic artery). Our case report demonstrates the severity of the course of the disease and that the prognosis for vision and life in patients with Takayasu's arteritis can be unfavorable.
References 1. Komarov FI, Nesterov AP, Margolis MG, Brovkina AF. [Ocular abnormalities in systemic disease]. Moscow: Meditsina; 1982 Russian 2. Fedorov SN, Klimova TL, Bogatyrev IuV. [Diagnostic importance of carotoid-compression tonography in occlusive processes in the carotid arteries]. Vestn Oftalmol. 1975 Mar-Apr;(2):11-6 Russian
|