J.ophthalmol.(Ukraine).2016;6:24-28.
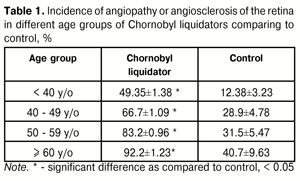
| https://doi.org/10.31288/oftalmolzh201662428 Patterns of development of retinal vascular pathology at remote time period after radiation exposure Introduction Chornobyl disaster in 1986 affected nearly 5 million people. Only in our country, over 2 thousands of towns and villages with population about 2.6 million were contaminated with radionuclides. Large groups of Ukraine’s populations involved in the liquidation of the Chernobyl NPP accident consequences were exposed to ionizing radiation. Radiation exposure comparable in its effect to nuclear warfare has caused stable negative future-oriented changes in population’s health. A brand new artificial geochemical province [1] has appeared with background radiation increased as compared to “prenuclear” norm, which will be affecting the health condition and, without a doubt, eye disease incidence for a long time. Besides, works are carried out at a destroyed nuclear reactor, known as the Shelter Object, to transform it into an environmentally safe system. The staff working at the Shelter Object are constantly radiation exposed. Probability of new accident environmental contamination with remained radioactive material is a factor that makes us draw a lesson from Chornobyl in details. Each physician must be prepared as far as it possible to counter negative consequences of radiation exposure. Retinal vascular system has been proved to be extremely sensitive to ionizing radiation exposure [5]. Since changes in vascular system of the eye can cause many severe diseases, vascular system of the eye in radiation exposed persons requires priority medical examination. The purpose of the present study was to analyze regularities in development of retinal vascular pathology at remote time period after radiation exposure. Material and Methods We used results of long-term follow-up of two cohorts of Chornobyl liquidators participating in 1986-1987 years. The first cohort included 5 195 participants of the liquidation of Chernobyl NPP accident consequences of those, logged in clinical and epidemiological registry of Chornobyl disaster victims, followed up in the period between 1992 and 2004 years, with mean age of (47.19±0.13) years and normal age distribution. Data on radiation dose exposed were obtained from database of clinical and epidemiological registry; absorbed excessive radiation dose ranged from 0.0001 to 3.22 Gy; mean dose was equal to 0.30±0.01Gy; patients were dose grouped using Poisson distribution (l=2.76, ??=136.66, p < 0.001). The second cohort included 2 910 radiation exposed participants of the liquidation of Chernobyl NPP accident consequences who are inhabitants of Dnipropetrovsk region. The survey had 15 stages and 26 753.33 person years. At the first examination (baseline) mean age of the patients was 35.48 ± 0.13 years with a normal age distribution. Official doses of external exposure of the whole body for all patients examined were recorded from 0.01 Gy to 0.7 Gy with mean dose of 0.21 ± 0.001Gy and normal dose distribution. Follow-up period was 13 years, from 1988 to 2001. We used external controls (2 cohorts, with a total of 1 488 persons not suffering from radiation damage) and internal control within the cohorts (groups of Chornobyl liquidators with radiation dose less than 5 cGy). Patients performed standard ophthalmic examination, biomicroscopy, reverse and direct ophthalmoscopy, calibrometry of retinal vessels as an additional method (we measured a caliber of superior temporal branch of central retinal artery and vein that have less diameter changeability and smaller diameter as compared to inferior temporal and inferior nasal branches). When performing statistical analysis we assessed such parameters as risk, mean, dispersion, standard deviation, factor score, and functional dependence coefficient; determined absolute risk of ophthalmopathology defined, parameters of prevalence and incidence, relative risks for different age and dose groups of participants of the liquidation of Chernobyl NPP accident consequences; created models of absolute, relative and attributive risk. Student Test Statistics was used for comparison of variables with 95% level of significance. Results Long-term follow-up of cohort of 5 195 Chornobyl liquidators revealed an apparent increase in retinal angiopathy prevalence which occurred every year and was significant (314.8±14.5 and 911.9±19.7 per 1 000 persons in 1993 and 2004, respectively). Its relative risk in 1988 in comparison with 1994 was 1.16 (1.1; 1.23), ?2 = 19.31 and p < 0.001. Pathological changes in retinal vessels (angiopathy or angiosclerosis) were noted more often than intact vessels when performing ophthalmoscopy in Chornobyl liquidators (Table 1). Incidence of retinal vessel pathology was high in relatively young age groups (Table 1). So, relative risk for Chornobyl liquidators aged < 39.9 years was equal to 3.98 compared to control, vs. 2.3, 2.6, and 2.26 in age groups of 40-49.9, 50-59, and 60 y/o, respectively. Thus, angiopathy incidence increased mainly due to young age groups. Such data have been obtained by other authors as well [2-4].
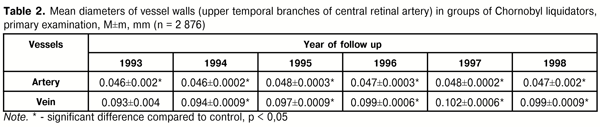
Development of vascular pathology of the eye in radiation exposed people is characterized by clinical features as follows: it starts with changes in capillary and veins, followed by changes in great diameter vessels and, finally, by organic changes in vessel walls. The initial changes in retinal vessels of Chornobyl liquidators were of distonic character with venous dilatation and vein caliber violation. Approximately in 10 % of angiopathy, we observed microaneurysm development in non-diabetic patients. Afterwards, hypertensive angiopathy prevailed among angiopathies in radiation exposed patients. Angiopathy was diagnosed with artery narrowing and venous dilatation in 52 % of cases, with artery and vein narrowing in 5%, with artery and vein dilatation in 8%, and, in the rest of cases, with vein dilatation and without significant changes in artery diameter. We also observed other variants of retinal vascular pathology: in some patient, dilatation of arteries resulted in their equaling with veins in diameter; in other cases, spasm of vessels in macular area was noted in the presence of dilatation of other retinal vessels; cases of abnormal vascular tortuosity were observed. Microaneurysms in non-diabetic patients developed approximately in 5 % of cases. Mean diameters of retinal arteries and veins (upper temporal branches) for Chornobyl liquidators according to follow-up time points are given in Table 2. In control group, including patients with arterial hypertension, mean diameter of arteries and veins averaged 0.053±0.0008, and 0.085±0.0013, respectively.
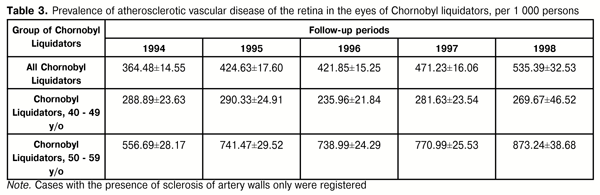
As it can be seen in data given (Table 2), artery diameter in Chornobyl liquidators was significantly smaller than that in the control group while vein diameter was significantly larger, except for patients examined in 1993. Vein diameter increase was significant within the follow-up period: mean vein diameter in Chornobyl liquidators increased in 1998 by 5.32% as compared to the year of 1994 (t=3.95, p<0.01). Thus, calibrometry of retinal vessels revealed that artery narrowing and progressive vein dilatation prevailed in the clinical picture of angiopathy in Chornobyl liquidators. The following analysis of ophthalmoscopy and calibrometry data showed that hypertensive angiopathy prevailed among other angiopathies at the baseline of our study. Angiopathy was diagnosed in the presence of artery narrowing and vein dilatation in 79% of cases, vein and artery narrowing was noted in 6%, artery and vein dilatation was in 3 %, and vein dilatation without significant changes in artery diameter was in 12%. Other variants of retinal vascular pathology were noted: in some patient, dilatation of arteries resulted in their equaling with veins in diameter; in other cases, spasm of vessels in macular area was noted in the presence of dilatation of other retinal vessels; cases of abnormal vascular tortuosity were observed. Following up the changes, we observed angiopathy transforming into angiosclerosis: thickened artery walls, more contrast reflex on them, luminal occlusion, and uneven caliber. Retinal angiosclerosis prevalence significantly increased over time at the primary examination as well, largely due to young age groups (Table 3).
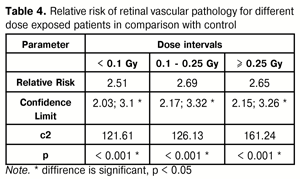
Relative risk of angiosclerosis in 1995 compared with 1994 was equal to 1.1 (confidence limit (CL) 1.01; 1.24) due to age group of 50-59 y/o, where that equaled 1.35 (1.19; 1.54). No significant changes were noted in relative risk in 1996 compared with 1995. Relative risk in 1997 compared with 1996 was again significantly higher, 1.1 (confidence limit 1.02; 1.18), ?2=5.22, p=0.02. Risk increase was by means of < 40 age group, in which it equaled 2.15 (1.05; 4.37). In 1998, risk was significant higher as compared with 1997, 1.04 (0.94; 1.16). Dose dependence analyzes revealed that relative risk (RR) of retinal angiosclerosis was significant for patients exposed to external radiation of higher doses. Thus, RR for patients exposed in a dose of 0.5 Gy and more, compared to those with 0.1 Gy dose, was equal to 1.6 (1.37; 1.88) with ?2 = 34.1 and p < 0.001. Risk of angiopathy and retinal angiosclerosis for groups with different radiation dose in comparison to control is given in the Table 4.
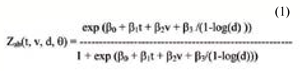
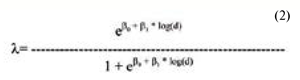
In 10 year period after radiation exposure, we observed dose dependence of angiopathy prevalence. Thus, in 1994, relative risk for patients exposed to a dose of 0.05- 0.99 Gy, compared to those exposed to 0.05 Gy dose, was equal 1.13 (CL 1.01; 1.27); RR for patients exposed in a dose of 0.1-0.249 Gy, compared to those exposed in 0.05 Gy dose, was 1.19 (CL 1.08; 1.31), p < 0.01. An adequate model of absolute risk of angiopathy in Chornobyl ligquidators group was described by equation (1):
where Zab – absolute cumulative risk; t - stay-at-risk duration; v – age at the moment of examination; d – radiation dose. Thus, retinal angiopathy prevalence depended on post-radiation stay-at-risk duration, age at the moment of examination, and radiation dose. A model of relative risk of angiopathy (an adequate model, Likelihood Ratio Statistic on 2 DF = 297.78, p < 0,001) was described by equation (2):
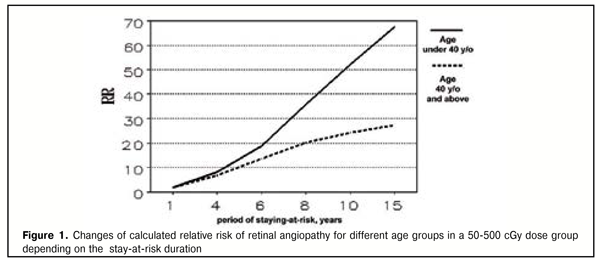
where d - dose, Gy. Angiopathy RR in a dose, calculated using the model (2), equaled 1.29 (CL 10.7; 1.56). It was shown that the main factors determining retinal angiopathy risk are age and stay-at-risk duration; radiation dose affected in a less degree. Statistically significant excess of risk of retinalvascular pathology can occur in 4-5 years, followed by the rapid increase of absolute risk between the years 5 and 6 after radiation exposure. Retinal angiopathy occurrence at the remote time period, at 15 and more years of staying-at –risk, becomes more probable for persons being exposed at a younger age. This effect is demonstrated in Figure 1 indicating changes in retinal angiopathy relative risk, calculated according to the model for different age groups in a 50-200 cGy dose group depending on the duration of stay-at-risk. RR for age groups begins to differ significantly at 4-5 years of staying-at-risk after radiation exposure.
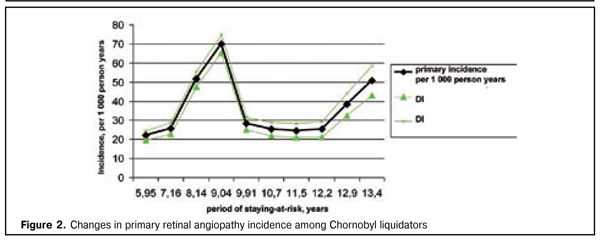
Results of studying the initial incidence of retinal angiopathy in Chornobyl liquidators in long-term follow-up of 2 892 radiation exposed persons evidenced that it increased significantly over this period (Figure 2).
Incidence increased in the period of staying-at-risk and reached its maximum at 9 years after radiation exposure, followed by a slight incidence decrease with a re-increase at 13 years after radiation damage. It was found that RR for a group exposed to a dose of 30-70 cGy, compared to those exposed to 1-30 cGy dose, equaled 1.67 (1.0; 2.79). So, a chance of retinal angiopathy development for persons exposed to a dose ? 30 Gy is 1.67 times higher than for those exposed to a dose < 30 cGy. Thus, this is the first time when a statistically significant higher level of primary retinal angiopathy incidence after radiation exposure was determined in persons exposed to a higher dose. The data obtained evidenced that changes in the vascular system of the eye n radiation exposed persons could be defined as radiation-induced effect. Conclusions 1. Pathology of retinal vessels is the most common eye disease in radiation exposed persons and can develop as early as 4-5 years after radiation exposure. 2. The main risk factors for its development in cohorts of Chornobyl liquidators are age and external radiation dose. 3. Primary angiopathy incidence reached the first maximum at 9 years with re-increase at 13 years after radiation exposure. References
|