J.ophthalmol.(Ukraine).2016;5:18-21.
|
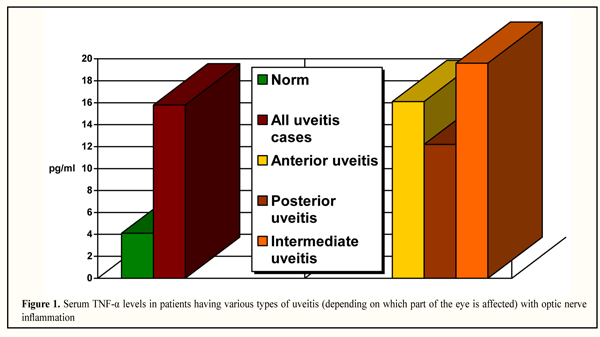
https://doi.org/10.31288/oftalmolzh201651821 Alterations in the expression of tumor necrosis factor-alpha in the uveitis with optic nerve inflammation N.V. Panchenko, Dr Sc (Med) M.N. Samofalova, DM E.N. Gonchar, DM D.O. Prikhod’ko, DM G.S. Arustamova, DM A.V. Lytvyshchenko, DM Department of Ophthalmology, Kharkiv National Medical University Kharkiv, Ukraine E-mail: panchenko0802@gmail.com Purpose: To assess serum levels of tumor necrosis factor-alpha (TNF-?) in uveitis patients with optic nerve inflammation (ONI). Materials and Methods: A retrospective evaluation of 132 patients who underwent examination and treatment for uveitis with ONI was performed. A commercially available enzyme-linked immunosorbent assay kit was used to measure serum TNF-? levels. Serum samples of 30 healthy donors were used as controls. Results: Serum TNF-? levels in uveitis patients with ONI were 3.8 times higher compared to those in healthy controls (15.8 ± 1.02 pg/mL and 4.1 ± 1.52 pg/mL, respectively, p < 0.05). The highest increase in serum TNF-? levels compared to controls was seen in intermediate uveitis. Conclusion: Serum TNF-? levels in active period of uveitis with ONI were found to be statistically significantly increased compared to those in controls. This finding provides the rationale for the use of anti-TNF-? agents for the treatment of uveitis with optic nerve inflammation. Key words: uveitis with optic nerve inflammation, tumor necrosis factor-alpha Introduction Tumor necrosis factor-alpha (TNF-?) is a proinflammatory cytokine produced by several types of cells (macrophages and activated T-cells) which can exert a tissue-dependent effect on the expression of various cytokines under pathological conditions. In addition, TNF-? plays a role in chronic inflammation and contributes to autoimmune response development [1] in non-physiological situations. It is an important mediator of intraocular tissue damage in uveitis patients as well as in different models of experimental uveitis [1, 2]. A significant role of TNF-? in the development of inflammation in the choroid has been demonstrated in animal uveitis models [3, 4]. Elevated TNF-? levels in the anterior chamber fluid [5, 6], vitreous [7], iris and ciliary body [8] of animals with experimental autoimmune uveitis have been reported. Some studies have found elevated TNF-? levels in the vitreous of patients with sarcoid uveitis [9] and endogenous uveitis in general [10]. Most of the studies have noted elevated TNF-? levels in the anterior chamber fluid of patients with uveitis [11, 12, 13], including toxoplasmic, viral, presumed tuberculous, intermediate and HLA-B27-associated uveitis, as well as patients with Beh?et disease and Vogt-Koyanagi-Harada syndrome [12, 14, 16]. In 2006, Takase et al showed that TNF-? levels in the aqueous humor in infectious uveitis are higher than those in non-infectious uveitis [17]. Abu El-Asrar et al have reported that TNF-? levels in the anterior chamber fluid correlated with clinical uveitis activity [14]. However, others reported that TNF-? was found in the anterior chamber fluid and vitreous of 85% [16] and only 26% [18], respectively, of patients presenting with uveitis, whereas Foster et al have not found TNF-? in the anterior chamber fluid and vitreous of uveitis patients [19]. Evidence have been presented on elevated serum TNF-? in uveitis patients [2, 20], including those with Beh?et disease-associated uveitis [21-23]. Serum TNF-? levels in patients with uveitis associated with active Beh?et disease have been found to be significantly higher than those in patients with inactive disease [21], and according to Mesquida et al [22], can be used as a marker of activity of Beh?et-associated uveitis. In addition, in 2001, Santos Lacomba et al reported that elevated serum TNF-? levels are associated with recurrent uveitis [2]. However, others have found that serum TNF-? levels in uveitis patients were not significantly different from those of healthy controls [9, 11], or were below detection [17, 24]. Obviously, this issue requires clarification. To the best of our knowledge, no data have been reported on serum TNF-? levels in uveitis patients with optic nerve inflammation. The purpose of the study was to assess serum levels of tumor necrosis factor-alpha (TNF-?) in uveitis patients with optic nerve inflammation (ONI). Materials and Methods A retrospective evaluation of 132 patients (53 men and 79 women; age, 18 to 74 years; duration of disease, 1 month to 14 years) who underwent examination and treatment for uveitis with ONI was performed. The standard ophthalmologic examination was performed, including ultrasound biomicroscopy (using a 50-MHz transducer) and optical coherence tomography. A commercially available enzyme-linked immunosorbent assay kit was used to measure serum TNF-? levels in uveitis patients with ONI. Serum samples of 30 healthy donors were used as controls. Statistica 6.1 software was used for the statistical analyses. Results and Discussion Serum TNF-? levels in uveitis patients with ONI were 3.8 times higher compared to those in healthy donors (15.8±1.02 pg/mL and 4.1±1.52 pg/mL, respectively), and this difference was statistically significant (p<0.05). These findings are consistent with other reports on elevated serum TNF-? levels in patients with uveitis [2, 20-23]. However, our findings differ from those of some studies [9, 11, 17, 24,, including studies conducted recently [11], that have reported no statistically significant difference in serum TNF-? levels between uveitis patients and healthy controls. The serum TNF-? levels in patients having various types of uveitis (depending on which part of the eye is affected) with ONI are shown in Fig. 1.
The highest (4.8 times) and the lowest (nearly 3 times) increase in serum TNF-? levels compared to controls were seen in intermediate uveitis and posterior uveitis, respectively. Interestingly, that the serum TNF-? levels in patients with anterior uveitis (16.18±1.09 pg/mL), posterior uveitis (12.2±1.31 pg/mL) and intermediate uveitis (19.6±1.25 pg/mL) were higher than in healthy controls (4.1±1.52 pg/mL), and each of these differences was statistically significant (p<0.05). In addition, there were statistically significant differences in serum TNF-? levels among patients with anterior uveitis, posterior uveitis and intermediate uveitis (p<0.05). Our findings on a greater increase in serum TNF-? in anterior uveitis with ONI than in posterior uveitis with ONI are indirectly confirmed by the findings of others on correlation of TNF-? levels in anterior chamber fluid [14] and sera [21, 22] with uveitis activity. The greatest increase in serum TNF-? observed in intermediate uveitis may evidence the presence of the autoimmune response, with the cytokine playing a significant role in its development [1]. Investigation of serum TNF-? in uveitis is especially promising in the light of the success of anti-TNF-? therapy for the disease. TNF-? inhibitors have been widely used in the treatment of rheumatologic diseases all over the world including the USA, and, since the first reported use in 2001 of a TNF-? inhibitor for the treatment of uveitis, several new anti-TNF-? agents have emerged for the treatment of different uveitis entities [25]. The anti-inflammatory efficacy and immune regulation role of anti-TNF-? therapy for uveitis have been confirmed in clinical trials (VISUAL I, VISUAL II) [26]. Adalimumab has recently become the first Food and Drug Administration (FDA)- and European Medicines Agency (EMA)-approved TNF-? inhibitor for the treatment of uveitis [27]. Investigations on the potential of other biological preparations for the treatment of uveitis are underway. It is noteworthy that our finding of elevated serum TNF-? in uveitis with ONI is to be considered in interrelationship with the activity of matrix metalloproteinase type 9 (MMP-9), with the latter targeting collagen IV, a major component of blood-brain barrier basal lamina [28]. In 2013, Yamada H. et al showed in their experimental study that the expression of MMP-9 increased in the presence of TNF-?, and that increased levels of MMP-9 in cells that form the blood aqueous barrier resulted in degradation of the structure and increased permeability of these cells [29]. In addition, we have previously found that increased levels of MMP-9 (gelatinase type B) in uveitis patients are associated with the development of optic nerve subatrophy [30]. Hence, the use of anti-TNF-? therapy in uveitis with optic nerve inflammation is in need not only for resolution of inflammation, but is also promising for the reduction of TNF-?-induced expression of MMP-9 [29], which we believe may contribute to reduction in the risk of developing optic nerve subatrophy. Conclusions In conclusion, serum TNF-? levels in active period of uveitis with optic nerve inflammation were found to be statistically significantly increased compared to those in controls. This finding provides the rationale for the use of anti-TNF-? agents for the treatment of uveitis with optic nerve inflammation.
References 1.Molins B, Mesquida M, Lee RW, et al. Regulatory T cell levels and cytokine production in active non-infectious uveitis: in-vitro effects of pharmacological treatment. Clin Exp Immunol. 2015 Mar;179(3):529-38 2.Santos Lacomba M, Marcos Mart?n C, Gallardo Galera JM, et al. Aqueous humor and serum tumor necrosis factor-alpha in clinical uveitis. Ophthalmic Res. 2001 Sep-Oct;33(5):251-5 3.Chang KC, Shieh B, Petrash JM. Aldose reductase mediates retinal microglia activation. Aldose reductase mediates retinal microglia activation. Biochem Biophys Res Commun. 2016 Apr 29;473(2):565-71 4.Yadav UC, Shoeb M, Srivastava SK, Ramana KV. Aldose reductase deficiency protects from autoimmune- and endotoxin-induced uveitis in mice. Invest Ophthalmol Vis Sci. 2011 Oct 17;52(11):8076-85 5.Caspi RR. Understanding autoimmune uveitis through animal models. The Friedenwald Lecture. Invest Ophthalmol Vis Sci. 2011;52(3): 1872–9 6.Trinh L, Brignole-Baudouin F, Pauly A, et al. Th1- and Th2-related chemokine and chemokine receptor expression on the ocular surface in endotoxin-induced uveitis. Mol Vis. 2008; 14: 2428–34 7.Turgut B, Gul FC, Dagli F, et al. Impact of ghrelin on vitreous cytokine levels in an experimental uveitis model. Drug Des Devel Ther. 2013 9;7:19-24 8.Ortencio KP, Renzo R, Sobrinho B AA, et al. Effects of morphine on the expression of cytokines and inflammatory mediators in a rabbit model of endotoxin-induced experimental uveitis. Arq Bras Oftalmol. 2015 Nov-Dec;78(6):371-5 9.Nagata K, Maruyama K, Uno K, et al. Simultaneous analysis of multiple cytokines in the vitreous of patients with sarcoid uveitis. Invest Ophthalmol Vis Sci. 2012 Jun 20;53(7):3827-33 10.Shibata M, Sato T, Taguchi M, et al. Analysis of Cytokines Related to Helper T and Regulatory T Cells in the Vitreous of Uveitis Patients. Nippon Ganka Gakkai Zasshi. 2015 Jun;119(6):395-401 11.Chen W, Zhao B, Jiang R, et al. Cytokine expression profile in aqueous humor and sera of patients with acute anterior uveitis. Curr Mol Med. 2015 ;15(6):543-9 12.Hern?ndez Garfella ML, Palomares Fort P, Rom?n Ivorra J, Cervera Taulet E. Aqueous Humor Levels of Different Interleukins 1-?, 2, 6 and 10, Tumor Necrosis Factor-? and Vascular Endothelial Growth Factor in Uveitis Treated with Adalimumab. J Ophthalmic Vis Res.2015 Jan-Mar;10(1):49-54 13.Sijssens KM, Rijkers GT, Rothova A, et al. Cytokines, chemokines and soluble adhesion molecules in aqueous humor of children with uveitis. Exp Eye Res. 2007 Oct 22;85(4):443-9 14.El-Asrar AM, Struyf S, Kangave D, et al. Cytokine and CXC chemokine expression patterns in aqueous humor of patients with presumed tuberculous uveitis. Cytokine. 2012 Aug;59(2):377-81 15.El-Asrar AM, Struyf S, Kangave D, et al. Cytokine profiles in aqueous humor of patients with different clinical entities of endogenous uveitis. Clin Immunol. 2011 May;139(2):177-84 16.Lahmar I, Abou-Bacar A, Abdelrahman T, et al. Cytokine Profiles in Toxoplasmic and Viral Uveitis. J Infect Dis. 2009;199:1239-49 17.Takase H, Futagami Y, Yoshida T, et al. Cytokine Profile in Aqueous Humor and Sera of Patients with Infectious or Noninfectious Uveitis. Invest Ophthalmol Vis Sci. 2006 Apr;47(4):1557-61 18.Franks WA, Limb GA, Stanford MR, et al. Cytokines in human intraocular inflammation. Curr EyeRes. 1992; 11(Suppl):187–91 19.Foster CS, Tufail F, Waheed NK, et al. Efficacy of etanercept in preventing relapse of uveitis controlled by methotrexate. Arch Ophthalmol. 2003;121(4):437-40 20.Cordero-Coma M, Calleja S, Llorente M, et al. Serum cytokine profile in adalimumab-treated refractory uveitis patients: decreased IL-22 correlates with clinical responses. Ocul Immunol Inflamm. 2013 Jun;21(3):212-9 21.Evereklioglu C, Er H, Turkoz Y, Cekmen M. Serum levels of TNF-alpha, sIL-2R, IL-6, and IL-8 are increased and associated with elevated lipid peroxidation in patients with Beh?et's disease. Mediators Inflamm. 2002 Apr;11(2):87-93 22.Mesquida M, Molins B, Llorens V, et al. Proinflammatory cytokines and C-reactive protein in uveitis associated with Behcet's disease [Electronic resource]. Mediators Inflamm. 2014. Retrieved from: http:/dx.doi.org/10.1155/2014/396204 23.T?rkc? FM, ?ahin A, Cing? AK, et al. Serum omentin, resistin and tumour necrosis factor-? levels in Behcet patients with and without ocular involvement. Graefes Arch Clin Exp Ophthalmol. 2015 Sep;253(9):1565-8 24.Curnow SJ, Falciani F, Durrani OM, et al. Multiplex Bead Immunoassay Analysis of Aqueous Humor Reveals Distinct Cytokine Profiles In Uveitis. Invest Ophthalmol Vis Sci. 2005 Nov;46(11):4251-9 25.Cordero-Coma M, Sobrin L. Anti-tumor necrosis factor-? therapy in uveitis. Surv Ophthalmol. 2015 Nov-Dec;60(6):575-89 26.Jaffe GL, Thorne JE, Scales D, et al. SAT0523 Adalimumab in Patients with Active, Non-Infectious Uveitis Requiring High-Dose Corticosteroids: the Visual-1 Trial. Ann Rheum Dis. 2015;74:849-50 27.Brooks M. FDA Clears Adalimumab (Humira) for Uveitis [Electronic resource] / M. Brooks // Medscape. – 2016. – Retrieved from: http://www.medscape.com/viewarticle/865654 28.Khovalyg NM, Fadeeva NI, Korenovskiy YuV. [Determination of matrix metalloproteinase type 9 in the plasma of premature neonates for the prognosis of perinatal damage to the CNS of premature neonates]. In: [Proceedings of the 8th International Congress on Health and Education in the 21st Century: Concepts of Diseases of Civilization]. Health and Education in the 21st Century Journal. 2007;9(4):334. Russian 29.Yamada H, Yoneda M, Inaguma S, et al. Infliximab counteracts tumor necrosis factor-?-enhanced induction of matrix metalloproteinases that degrade claudin and occludin in non-pigmented ciliary epithelium. Biochem Pharmacol. 2013 Jun 15;85(12):1770-82 30.Panchenko NV, Samofalova MN, Friantseva MV. [Levels of matrix metalloproteinase type 9 in different outcomes of uveitis with optic nerve inflammation]. Oftalmologiia. Vostochnaia Evropa. 2016;6(2):210-6. Russian
|