J.ophthalmol.(Ukraine).2016;4:29-31.
|
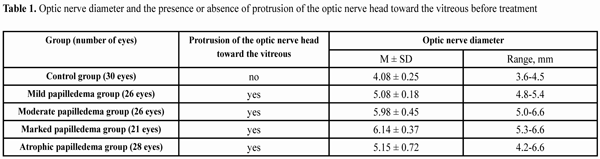
https://doi.org/10.31288/oftalmolzh201642931 Optic nerve ultrasound in idiopathic intracranial hypertension K.S. Iegorova, MD L.V. Zadoianyi, Cand Sc (Med) L.L. Marushchenko, Cand Sc (Med) Romodanov Neurosurgery Institute Kyiv, Ukraine E-mail: iegorova_katya@ukr.net Backup: Vision loss associated with secondary optic atrophy is the major complication of idiopathic intracranial hypertension (IIH). A potential for the development of severe visual impairment necessitates regular monitoring and determines the importance of ophthalmological examination in patients with this condition. Optic nerve ultrasound (ONUS) enables identification of IIH and monitoring of raised intracranial pressure (ICP) in these patients. Purpose: To investigate the diagnostic potential of ONUS. Materials and Methods: Fifty patients (100 eyes) underwent ONUS using general purpose ultrasound system Sonoline Versa Plus with 8-MHz transducer, before and after treatment for IIH. The control group included 15 healthy volunteers (30 eyes). Depending on the ophthalmoscopic changes, patient eyes were divided into four pre-treatment groups (mild papilledema, 26 eyes; moderate papilledema, 25 eyes; marked papilledema, 21 eyes and optic atrophy secondary to papilledema, 28 eyes) and two post-treatment groups (retinal angiopathy, 65 eyes; and secondary optic atrophy, 35 eyes). Results: The pre-treatment optic nerve diameter in mild, moderate, marked and atrophic papilledema eyes was found to be 5.08 ± 0.18 mm, 5.98 ± 0.45 mm, 6.14 ± 0.37 mm and 5.15 ± 0.72 mm, while that in controls was 4.08 ± 0.25 mm. Conclusion: ONUS is an accurate, fast, non-invasive and economical diagnostic technique for the detection of raised intracranial pressure in IIH. Key words: Idiopathic intracranial hypertension, papilledema, optic nerve ultrasound. Introduction Idiopathic intracranial hypertension (IIH) is a polyetiological syndrome characterized by the following signs and symptoms: symptoms of intracranial hypertension (including optic nerve (ON) swelling), raised cerebrospinal fluid (CSF) pressure (more than 200 mm H2O), no focal neurological symptoms (excepting cranial nerve VI paresis), and no magnetic resonance imaging (MRI) evidence of deformity, displacement or obstruction of the ventricular system or of other cerebral disorder (excepting the signs of raised CSF pressure) [1-3]. This condition most frequently occurs in obese women (having a body mass index of over 30 kg/m2) of 30-50 years of age with an endocrine disorder (menstrual irregularities, thyroid or adrenal gland disorder, or hypoparathyreosis) [4]. Development of papilledema secondary to raised intracranial pressure (ICP) is characteristic for IIH. Atrophy on the fundus secondary to optic nerve swelling is the main cause of incapacitation in IIH [5, 6]. A technique has been developed for ultrasound measurement of the optic nerve diameter, identification of intracranial hypertension (ICH) and monitoring of raised ICP. In 1964, Hayreh demonstrated in monkeys and in humans that the subarachnoid spaces surrounding the optic nerve communicate with the intracranial cavity. Raised CSF pressure is transmitted along the ON sheath and affects the ON, causing papilledema. Numerous investigators have proved that the diameter of the perioptic subarachnoid space in patients with ICH secondary to brain trauma or intracranial hemorrhage is elevated [7, 8]. Available invasive ICP measurement techniques (using an intraventricular catheter or probe) are prone to complications (intraventricular hemorrhage or infection or ventricular displacement), and, therefore, non-invasive ICP monitoring may be clinically relevant. The use of computed tomography (CT) or MRI for this purpose would be more expensive and would require more time. Orbit MRI as well as orbit CT is rarely performed in normal screening MRI and CT, which is an additional reason for performing optic nerve ultrasound (ONUS). According to Glaser, the most careful examination sometimes fails to reveal increased diameter of the orbital portion of the optic nerve in papilledema, which is caused by excessive CSF dynamics between the ON and the brain due to frequent eye motions and obstruction to the flow of interstitial fluid from the optic nerve disc by the cribiform plate. In the opinion of Glaser, this is the very cause of paplledema cases without signs of ICH [9]. There are no reports on the ONUS in papilledema in our country, and a few reports on this matter in the foreign literature [10, 11]. The purpose of the study was to investigate the diagnostic potential of ONUS. Materials and Methods The study involved 50 patients (50 eyes) with IIH who were treated at the Romodanov Neurosurgery Institute between 2000 and 2014. Basic ophthalmic examination included determination of visual acuity, biomicroscopy, perimetry and ophthalmoscopy. Fifty patients (100 eyes; age, 19 to 69 years; 37 women and 13 men) with IICH and 15 healthy volunteers (30 eyes; age, 20 to 40 years; 10 women and 5 men) underwent optic nerve ultrasound (ONUS) using general purpose ultrasound system Sonoline Versa Plus (Siemens AG, Munich, Germany) with 8-MHz transducer. Depending on the ophthalmoscopic changes, patient eyes were divided into four pre-treatment groups (mild papilledema, 26 eyes; moderate papilledema, 25 eyes; marked papilledema, 21 eyes and optic atrophy secondary to papilledema, 28 eyes) and two post-treatment groups (retinal angiopathy, 65 eyes; and secondary optic atrophy, 35 eyes). Standard ultrasound gel was used for all scans. Eye scans were performed with the patient supine, and with the probe placed on the upper eyelid. First, visualization of the posterior pole and orbit contents (including the optic nerve) was achieved in the grey scale mode. Protrusion assessment was considered not feasible due to instrument accuracy. The patient was asked to look straight ahead, and the optic nerve sheath diameter (ONSD; i.e., the diameter of the optic nerve taking into consideration the sheath) was measured. The data were statistically processed using Statistica 6.0 (StatSoft, Tulsa, OK). Results are presented as the mean and standard deviation (M ± SD). Mann-Whitney U test was used to determine intergroup differences, and Wilcoxon one sample test was used to compare intragroup changes over time. A P value of <0.05 was considered as statistically significant. Results and Discussion Table 1 presents pre-treatment optic nerve diameter measurements.
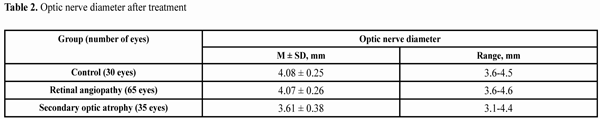
We compared the groups for the pre-treatment ONSD. The ONSD in mild, moderate, marked and atrophic papilledema eyes was found to be 5.08 ± 0.18 mm, 5.98 ± 0.45 mm, 6.14 ± 0.37 mm and 5.15 ± 0.72 mm, respectively. Protrusion of the optic nerve head toward the vitreous was found in all patients with papilledema. In control eyes, protrusion of the optic nerve head toward the vitreous was not characteristic, and the ONSD was 4.08 ± 0.25 mm (range, 3.6-4.0 mm). The difference in the optic nerve diameter between papilledema eyes and control eyes was found to be statistically significant (p < 0.05). Additionally, the ONSD was statistically significantly larger in moderate papilledema eyes than in mild papilledema eyes (p < 0.05). However, the statistically significant difference in the ONSD between eyes with different stages of papilledema was found not for all pairs of groups. We found no statistically significant difference in the ONSD between marked and moderate papilledema eyes (p > 0.05) and between atrophic and mild papilledema eyes (p > 0.05). The difference in the ONSD between atrophic and moderate papilledema eyes as well as between atrophic and marked papilledema eyes was found to be statistically significant (p < 0.05). In our study, in all cases in which papilledema was found ophthalmoscopically, the optic nerve was found to be thickened. This contradicts the findings of Glaser who believes that the enlarged diameter of the orbital portion of the optic nerve may not always be found in papilledema eye. Results on the optic nerve disc diameter in healthy volunteers reported in the literature are rather variable. Given below are the measurements of ONSD based on standard methodology (with the ONSD measured 3 mm posterior to the globe). Some of the studies have reported values as low as 3.2 mm to 3.7 mm. These values are less than those reported by Blaivas (2003; 4.42-4.8 mm), Tamburrelli (2000; 4.4-4.8 mm), Geeraets (2007; 4.6-4.8 mm), Bauerle (2012; 4.3-7.6 mm), and Maude (2013; 4.25-4.75 mm) [7, 8, 10-11], possibly because these authors determined the diameter of the optic nerve without taking into consideration the subarachnoid space. Our findings for the ONSD in healthy subjects are in agreement with those reported by Eliseeva (2009; 4.1-5.9 mm) [1] and Rykun (2006; 4.8 mm) [12]. We used ONUS images to determine the presence of (1) protrusion of the optic nerve head toward the vitreous and (2) thickened perioptic subarachnoid space in eyes of the study. No protrusion of the optic nerve head toward the vitreous and the subarachnoid space diameter of not more than 4.5 mm were found in control eyes. In papilledema eyes, protrusion as well as the increased perioptic subarachnoid space diameter (4.8-6.6 mm) was observed. There was no statistically significant difference in perioptic subarachnoid space diameter (the diameter varied from 5 mm to 6.6 mm) between mild and moderate papilledema eyes. One may suppose that finding of moderate papilledema on fundus examination is preceded by an increase in optic nerve diameter. After treatment of 50 patients (100 eyes) for intracranial hypertension, we observed changes over time in echographic characteristics of the optic nerve. Reduction in and disappearance of the protrusion of the optic nerve head toward the vitreous was found in 47 (47%) and 53 (53%), respectively, of the eyes. After treatment, the numbers of eyes experiencing a reduction, no change, and increase in the ONSD were 92 (92%), 8 (8%), and 0, respectively. Additionally, although after treating of some atrophic papilledema eyes, a reduction in swelling in them was observed based on ophthalmoscopy, no reduction in the ONSD was found based on ultrasound, evidencing a negative change in optic nerve sheath swelling, and thus requiring immediate measures to reduce ICP. Eyes were divided into post-treatment groups based on post-treatment ophthalmoscopic findings. Table 2 presents post-treatment optic nerve diameter measurements.
We compared the groups for the post-treatment diameter of subarachnoid space surrounding the optic nerve. The difference in the optic nerve diameter between atrophic and control eyes as well as between atrophic eyes and those of patients with retinal angiopathy was found to be statistically significant (p < 0.05). No statistically significant difference in the optic nerve diameter was found between the eyes of patients with retinal angiopathy and controls (р > 0.05). The results obtained provide evidence that optic nerve diameter approaches the normal range with the regression of papilledema, and decreases with the development of secondary optic atrophy, which requires for further study. Conclusions In conclusion, the optic nerve head protrudes into the vitreous and perioptic subarachnoid space increases in diameter to more than 4.8 mm based on ultrasound, with the development of papilledema secondary to IIH. The amount of increase in optic disc diameter in patients with IIH depends on the degree of optic nerve swelling. ONUS is an accurate, fast, non-invasive and economical diagnostic technique for the detection of raised intracranial pressure and provides for case monitoring in IIH.
References 1.Serova NK. [Clinical neuroophthalmology: Neurosurgical aspects]. Tver’: Triada Publishing House; 2011. 323 p. Russian 2.Monteiro MLR, Moura FC. [Ophthalmic aspects of idiopathic intracranial hypertension syndrome (pseudotumor cerebri)]. Rev Bras Oftalmol. 2008; 67(4):196-203. Portugal 3.Rosenfeld E, Kesler A. Pseudotumor Cerebri (Idiopathic Intracranial Hypertension) an Update. In: Neuroimaging – Clinical Applications. Bright P, editor. InTech, Rijeka; 2012. p. 373-400 4.Mezaal M, Saadah M. Idiopathic intracranial hypertension in Dubai: nature and prognosis. Acta Neurol Scand. 2005 Nov;112(5):298-302. 5.Tron EZh. [Visual pathway disorders]. Moscow: Medgiz; 1955. 394 p. Russian 6.Bruce BB, Preechawat P, Newman NJ, et al. Racial differences in idiopathic intracranial hypertension. Neurology. 2008 Mar 11;70(11):861-7 7.Malayeri AA, Bavarian S, Mehdizadeh M. Sonographic evaluation of optic nerve diameter in children with raised intracranial pressure. J Ultrasound Med. 2005 Feb;24(2):143-7. 8.Girisgin AS, Kalkan E, Kocak S, et al. The role of optic nerve ultrasonography in the diagnosis of elevated intracranial pressure. Emerg Med J. 2007 Apr; 24(4): 251-4. 9.Glaser JS (Ed.). Neuro-ophthalmology. 3rd ed. Philadelphia etc: Lippincott Williams and Wilkins; 1999 10.Stone MB. Ultrasound diagnosis of papilledema and increased intracranial pressure in pseudotumor cerebri. Am J Emerg Med. 2009 Mar;27(3):376. 11.Karakitsos D., Soldatos T., Gouliamos A., et al. Transorbital sonographic monitoring of optic nerve diameter in patients with severe brain injury. Transplant Proc. 2006 Dec; 38(10):3700-6. 12.Rykun VS. [Additional ultrasonographic criteria in the differential diagnosis of congestive and pseudocongestive optic disks]. Vestn Oftalmol. 2006 Jul-Aug;122(4):9-12. Russian
|