J.ophthalmol.(Ukraine).2016;3:28-30.
|
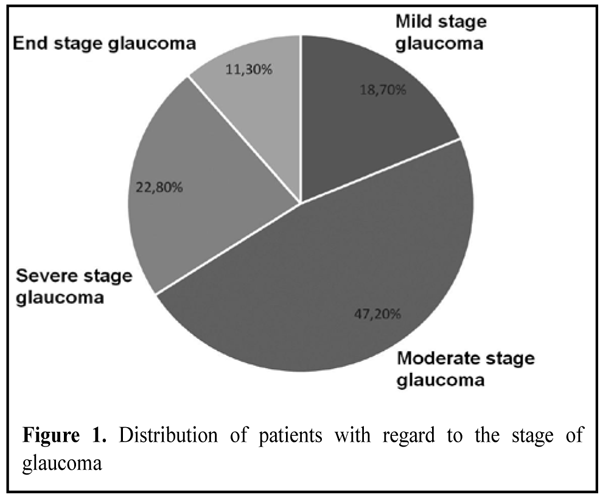
https://doi.org/10.31288/oftalmolzh201632830 Assessment of the efficacy of the combined surgical technique for primary open-angle glaucoma and age-related cataract V.O. Mel’nik,1 Cand Sc (Med), N.V. Kots-Gotlib,1 MD, R.L. Vladiuk,2 Cand Sc (Med), O.O. Hurzhii, MD 1Visiobud, Ophthalmology Department of Medbud, Medical Theoretical and Practical Association, Kyiv 2Ivano-Frankivsk National Medical University E-mail: elenahurzhii@gmail.com Purpose: To assess the efficacy of a combined surgical technique - combined phacoemulsification (phaco) with intraocular lens (IOL) implantation and modified tunnel trabeculopuncture, - in patients with primary open-angle glaucoma (POAG). Materials and Methods: Postoperative intraocular pressure, mean retinal light sensitivity and optical nerve fiber thickness were used as efficacy end points. Conclusion: The combined surgical technique is efficacious for primary open-angle glaucoma from the point of view of normalization of IOP and stabilization in the glaucoma process. Key words: primary open-angle glaucoma, phacoemulsification with tunnel trabeculopuncture, light sensitivity, optic nerve Introduction The number of people with glaucoma was estimated to be 60.5 million in the year 2010, increasing to 80 million in 2020. [1] Of these patients, 74% will have primary open-angle glaucoma (POAG), the second leading cause of blindness globally. Although a variety of medical and laser treatments for glaucoma are available, surgical treatment methods play a key role in managing this disease. [2] It is common to divide surgical interventions for glaucoma into fistulizing procedures (involving the perforation of ocular tunics) and penetrating procedures (non involving penetration of the anterior chamber of the eye). Normalization of intraocular pressure (IOP), stabilization of the glaucoma process (which some authors believe is achieved in only 60-68% of the patients operated on for glaucoma) and maximum surgical safety are considered as the basic requirements for surgical interventions for glaucoma. [3] To meet the European Glaucoma Society Guidelines, in order to achieve functional and morphological stabilization, the IOP reduction should be of 40% or more, compared with baseline. The success rate of glaucoma surgery in medically uncontrolled glaucoma has been reported to be 75%. [4] The two leading causes of inadequate IOP-lowering effect of surgical interventions for glaucoma are post-operative scarring of surgically-created outflow pathways [5] and cataract, which is a common comorbidity in glaucoma patients. Furthermore, it has been reported that (a) it is a surgical intervention for glaucoma that commonly precedes worsening of the cataract and (b) the latter not only reduces visual function but also hampers adequate and timely assessment of glaucoma progression over time [6]. Continuous advances in cataract surgical techniques have led to reduction in the rate of intra- and post-operative complications of combined surgery and improved the potential for microinvasive glaucoma procedures.[7] Although a variety of combined surgical techniques are available, there is a need for further development and improvement of efficacious surgical techniques for restoration of natural aqueous humor outflow pathways. The study purpose was to assess the efficacy of a combined surgical technique, combined phacoemulsification (phaco) with intraocular lens (IOL) implantation and modified tunnel trabeculopuncture, in patients with POAG. Patients were followed up for 3 years. Materials and Methods The study was conducted from 2013 to 2015 and involved 460 patients with POAG. Of these patients, 52.8% were women (mean age, 73.7 years) and 47.2% were men (mean age, 69.7 years). All patients underwent combined phacoemulsification (phaco) with intraocular lens (IOL) implantation and modified tunnel trabeculopuncture. In brief, the procedure involves the following steps. First, a conjunctival peritomy is performed along the limbus from the 11 o'clock to 1 o'clock positions. A one-half thickness quadrangular scleral flap is outlined and dissected. Then, a one-third thickness triangular scleral flap is outlined and dissected along with a scleral strip immediately over Schlemm’s canal. A traditional phaco with implantation of posterior chamber IOL is performed. Openings in Schlemm’s canal are created at 11 o’clock and 1 o’clock and the residual anterior lens capsule is drawn into the openings. The quadrangular scleral flap is positioned in the scleral bed and secured with interrupted sutures. Finally, conjunctiva is secured with sutures. Glaucoma severity and stages were graded by vertical cup size and number of scotomas in the central visual field. [8] Mild, moderate, severe and end-stage glaucoma were found in 86 patients (18.7%), 217 patients (47.2 %), 105 patients (22.8 %) and 52 patients (11.3 %), respectively (Fig. 1).
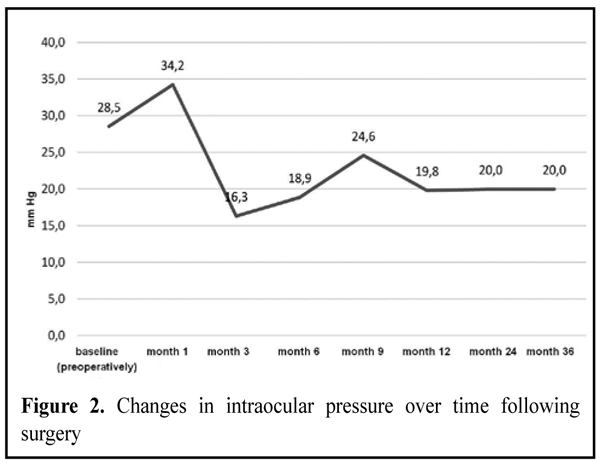
Results and Discussion All patients underwent measurements of IOP, retinal light sensitivity and nerve fiber density both preoperatively and postoperatively, at month 1, month 3, month 6, month 9, month 12, month 24 and month 36). The average IOP was 27.5±0.99 mmHg (р>0.05) preoperatively and increased at month 1. Thereafter, a steady reduction in the average IOP to normal values was observed over 12 months, and a stabilization of the average IOP levels was observed over the subsequent 24 months (Fig. 2).
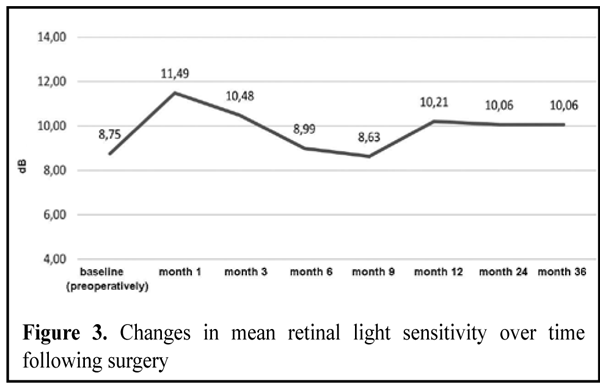
Figure 3 presents preoperative and postoperative mean retinal light sensitivity data. Postoperatively, the eyes exhibited improvement of this index over 2 months, with a subsequent restoration to baseline retinal light sensitivity levels by month 12 and a stabilization of the mean retinal light sensitivity levels over the last 24 months. In addition, compared to patients with severe glaucoma, those with mild or moderate glaucoma exhibited a more substantial and more stable improvement in the mean retinal light sensitivity levels over the first follow-up year.
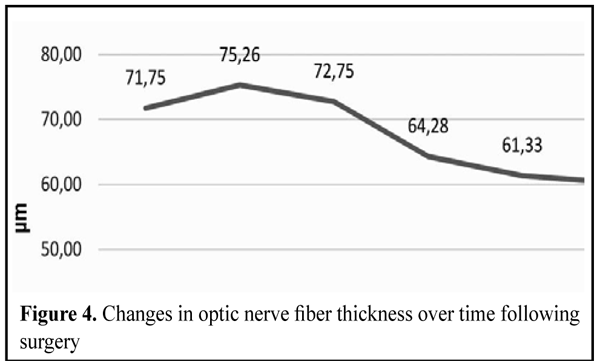
Figure 4 presents preoperative and postoperative optic nerve fiber density data. Postoperatively, the eyes exhibited a 16% reduction in this index over the first 12 months, with a subsequent stabilization of the optic nerve fiber density levels over the last 24 months of the follow-up. The amount of changes in the optic nerve fiber density levels over time was found to depend on the stage of glaucoma. Thus, compared to patients with severe glaucoma, those with mild or moderate glaucoma exhibited more substantial postoperative changes in the optic nerve fiber density levels.
Postoperatively, ocular hypotony and ciliochoroidal detachment were observed in 52 patients (11.3%) and 14 patients (3.0%), respectively. Subsequently, in these cases, hypotony was removed and ciliochoroidal reattachment was achieved with conservative treatment. The findings give evidence that this combined surgical technique is efficacious in the treatment of POAG and can be recommended as a procedure of choice for the disease. Among the positive endpoints of the combined surgical technique we would like to note the following: long-term normalization of IOP, reduction in the progression of glaucoma, stabilization of visual functions and low level of post-operative complications. It should be stressed that, although such conventional surgical interventions for glaucoma as sinus trabeculactomy and implantation of drainage devices are efficacious from the point of view of reduction in IOP, they can lead to serious complications including hypotony and corneal edema in the early postoperative period, as well as to ciliochoroidal detachment, suprachoroidal hemorrhage, diplopia and increased potential for endophthalmitis even in the late postoperative period. Conclusions In summary, the combined surgical technique is efficacious for primary open-angle glaucoma from the point of view of not only normalization of IOP, but also reduction in the progression and even stabilization in the glaucoma process. Since it is mean retinal light sensitivity and optic nerve fiber density levels that have been considered by a number of authors as the most unambiguous indices of visual function in glaucoma, our data suggests that the combined surgical technique is efficacious from the point of view of stabilization of peripheral vision and light perception. It is of note that this procedure has a lower rate of complications compared to conventional surgeries for glaucoma. References
|