J.ophthalmol.(Ukraine).2016;3:19-21.
|
https://doi.org/10.31288/oftalmolzh201631921 Effect of bioflavonoid quercetin on the course of inflammatory process in herpetic keratitis patients with dry eye syndrome S. Ya. Rafalyuk Danylo Halytsky Lviv National Medical University Lviv, Ukraine E-mail: sofiyaeye@ukr.net Backup: The problem of dry eye syndrome is of great importance and significance in ophthalmology. The purpose of the present paper was to study the effect of Lipoflavon on the course of inflammatory process in herpetic keratitis (HK ) patients with dry eye syndrome (DES). Material and Methods: Clinical study was performed in 40 patients with HK (superficial dendritic keratitis) and DES; additionally, we followed up 17 patients with HK. All patients were divided into two groups: Study Group included 15 HK and DES patients receiving Lipoflavon treatment; Control Group included 25 HK and DES patients receiving traditional treatment. The state of the cornea was scored by Draize criteria. The data obtained were statistically processed using SPSS 11.0 package. Results: Assessing the data obtained in the present study, it is arguable that Lipoflavon significantly decreases clinical signs in patients with HK and DES. Conclusions: Inclusion of Lipoflavon in the complex treatment of HK patients with DES significantly increases the efficacy of therapy that is evidenced by the fact that corneal epithelization and infiltrate dispersion are accelerated, and corneal edema and epitheliopathy of the cornea and conjunctiva are less apparent after treatment of patients in Study group as compared to control. The use of quercetin has a positive effect on qualitative and quantitative characteristics of tear production in patients with HK and DES, in particular, Schirmer test values are increased, tear break-up time is increased, conjunctival fold intensity is decreased and tear meniscus height is increased. Key words: herpetic keratitis, dry eye syndrome, cornea, clinical signs, Lipoflavon
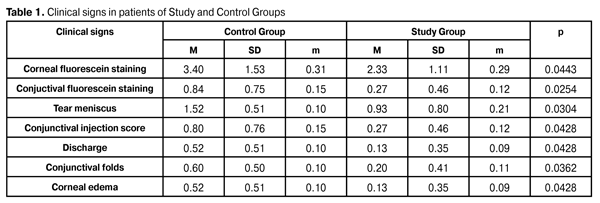
Introduction Recently, inflammatory eye diseases have been one of the main reasons of temporary disability; besides, their recurring and complications can often cause permanent disability of the patients. Herpetic keratitis is the most common corneal pathology, the cause of corneal opacity and corneal blindness. Modern methods of keratitis treatment are not always able to achieve a desired effect. Traditional medication does not always lead to patient’s cure and recurrence prevention [1]. It is difficult to use corticosteroids with an anti-inflammatory purpose in herpetic keratitis patients since these drugs are contraindicated in the presence of corneal erosion. Significant difficulties in that respect can arise when treating keratitis in patients with dry eye symptom (DES) [2, 3]. The progress in this regard can be achieved only on the basis of the advanced study of pathogenic mechanisms determining development and course of inflammatory process in the cornea and ocular surface tissues [4, 5, 6, 7, 8]. In view of the above, the use of flavanoids with anti-inflammatory purpose in patients with inflammatory disease and concomitant corneal erosion is of great importance. Previously, we have shown that bioflavonoid quercetine, a natural anti-oxidant containing in Lipoflavon drug, has a positive effect, in particular, decreases the degree of disorders in biochemical characteristics in tear fluid in herpetic keratitis (HK) patients with DES [9]. The purpose of the present paper was to study the effect of Lipoflavon on the course of inflammatory process in HK patients with DES. Material and Methods Clinical study was performed in 40 patients with HK (superficial dendritic keratitis) and DES; additionally, we followed up 17 patients with HK. All patients were divided into two groups: Study Group, HK and DES patients receiving Lipoflavon treatment, 15 patients; Control Group, HK and DES patients receiving traditional treatment, 25 patients. The state of the cornea was scored by Draize criteria (corneal fluorescein staining, conjuctival fluorescein staining, tear meniscus, conjunctival injection score, conjunctival discharge, conjunctival folds, corneal edema, corneal infiltration, Schirmer test II, and tear break-up time). Traditional therapy included anti-herpetic drugs locally and parenterally (aciclovir, valaciclovir), antiseptics and antibiotics (if indicated), non-steroid anti-inflammatory drugs, mydriatics, tear substitutes, and corticosteroids at a proper stage of the disease. The data obtained were statistically processed using SPSS 11.0 package [10].
Results and Discussion At baseline, clinical characteristics studied did not differ significantly in patients with HK and DES of Study and Control Groups. At the same time, inflammatory signs were significantly lower in HK patients without SED as compared to those in patients with HK and SED in Study and Control Groups (р<0.05). The Study Group patients received Lipoflavon in the complex of drug therapy. In these patients, epithelization of corneal dendritic erosion was noted at Day (4.7±0.4) that was significantly faster as compared to Control Group, in which corneal erosion was epithelialized at Day (6.8±0.6). Corneal infiltration was absent at Days (5.5±0.5) and (7.8±0.7), respectively, in Study and Control Groups. At Day 10 of treatment, the corneal fluorescein staining score in patients with HK and SED receiving Lipoflafon was only (2.33±0.29) as compared to control, (3.40±0.31); punctate conjuctival fluorescein staining score in Study and Control groups was (0.27±0.12) and (0.84±0.15), respectively; the height of tear meniscus in Study and Control groups equalled (0.93±0.21) and (1.52±0.10) mm, respectively; mixed conjunctival injection in HK and SED decreased to (0.27±0.12) scores after quercetin treatment vs. (0.80±0.15) scores in Control group; conjuncival discharge intensity score in Study and Control groups was (0.13±0.09) and (0.52±0.10), respectively; the presence of conjunctival folds in HK and DES and Lipoflavon treatment was (0.20±0.11) scores vs. (0.60±0.10) scores in Control group; corneal edema was less apparent in Study group as compared to controls, (0.13±0.09) and (0.52±0.10), respectively. Mann-Whitney test was used for comparative analyses between groups; the significance of differences of inflammatory signs was р<0.05 in all cases. It should be noted that tear break-up time in Control and Study groups was (5.24±0.19) s and (6.13±0.32) s, respectively, (р<0.05). Schirmer test values were (7.36±0.28) mm/5min in Control, and (10.47±0.83) mm/5min in Study group (р<0.01). Conclusions 1.Inclusion of Lipoflavon in the complex treatment of HK patients with DES significantly increases the efficacy of therapy that is evidenced by the fact that corneal epithelization and infiltrate dispersion are accelerated, and corneal edema, epitheliopathy of the cornea and conjunctiva are less apparent after treatment of patients in Study group as compared to control. 2.The use of quercetin has a positive effect on qualitative and quantitative characteristics of tear production in patients with HK and DES, in particular, Schirmer test values are increased, tear break-up time is increased, conjunctival fold intensity is decreased and tear meniscus height is increased References
|