J.ophthalmol.(Ukraine).2016;3:15-18.
|
https://doi.org/10.31288/oftalmolzh201631518 Technological characteristics of cataract surgery in eyes with posterior chamber phakic intraocular lens implanted previously D.O. Marshava1 Iu.M. Lazar, Cand. Of Sc. (Med.) 2 1Multiprofile clinics L/J Kutaisi (Georgia) 2Fiatov Eye Diseases and Tissue Therapy Institute Odessa, Ukraine E-mail: marshava-david@mail.ru Key words: cataract, phakic intraocular lens, bilensectomy Introduction. Implantation of phakic intraocular lenses (PIOL) is used for the correction of high myopia. The problem of PIOL implantation is that cataract may develop in a long-term period after surgery due to the contact of constructive PIOL elements to anterior and posterior chamber tissues. So, the development of advanced surgical techniques enabling to perform bilensectomy as safely and quickly as possible is of a great importance. The purpose of the present study was to improve the technique for cataract extraction in patients with posterior chamber PIOLs implanted previously. Material and Methods. A total of 19 cases of cataract extraction in 11 patients with plus and minus models of posterior chamber PIOLs were studied. 12 of explanted PIOLs were made of collagen copolymer and 7 of them were of silicone. Results. Endothelial cell loss (ECL) after bilensectomy averaged 9.1% in a study group. ECL increased after cataract phaco emulsification to 11% in 11 eyes at time point of 6 months after surgery and to 12.2% in 5 eyes with five-year follow-up. There was noted a tendency of a more rapid visual function recovery (on the average, at Day 5 after surgery) and less endothelial cell loss when using the bilensectomy techniques improved. Conclusion. The improved bilensectomy technique enabled to perform effectively and safely the rehabilitation of patients with cataract with implanted PIOLs.
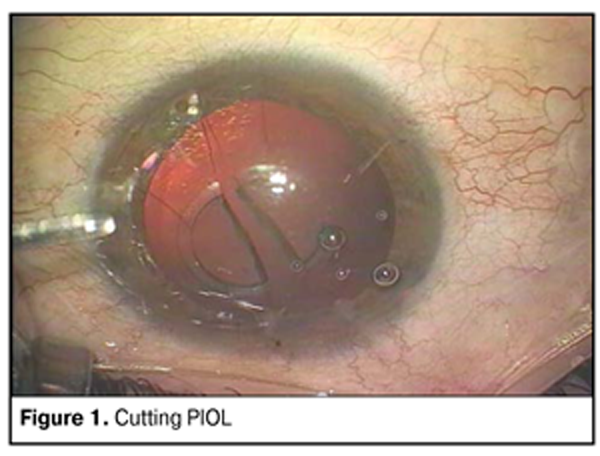
Background The use of phakic intraocular lenses (PIOL) has been becoming more popular for the correction of high myopia. The most common PIOL types are posterior chamber PIOLs of collagen copolymer and silicone. At the present time, approximately 1 to 3 thousand PIOLs of various types are implanted every year [1, 2, 3, 4, 5]. Despite the little proportion in the refractive surgery, PIOLs occupy their niche in correction of myopia more than 15.0 D and hyperopia between 5 and 13 D, including those in children and adolescents [6, 7, 8]. However, with collection of data on long-term outcome of PIOL implantation in myopia and hyperopia, in literature have appeared papers on different complications at different time terms after surgery [9]. The papers have brought out clearly that cataract development in the eyes with various PIOL types is caused and associated pathogenetically with the characteristics of contact of PIOL constructive elements to tissues of anterior and posterior chamber of the eye [10]. Thus, patients who underwent ametropia correction with PIOL implantation, on the one hand, age the period when cataract develops in the eye’s natural lens and, on the other hand, this process is induced and accelerated by the presence of PIOL in the eye. So, the development of advanced surgical techniques enabling to perform bilensectomy as safely and quickly as possible is of a great importance [11]. The purpose of the present study was to improve the technique for cataract extraction in patients with posterior chamber PIOLs implanted previously. Material and Methods A total of 19 cases of cataract extraction in 11 patients with plus and minus models of posterior chamber PIOLs were studied. Among them, 12 and 7 removed PIOLs were of collagen copolymer and silicone, respectively. Each patient underwent ultrasound biomicroscopy in addition to obligate clinical and functional investigations. We determined the density of endothelial cells, performed histological examination of the anterior capsule of the lens and studied the surface of PIOLs removed. Preoperative preparation included drug therapy decreasing immune response degree and strengthening vessel walls (corticosteroids, vasoprotectors, and adaptogens). When selecting the optic power of aphakic IOL, the patient was informed of impossibility to achieve simultaneous good outcome for both distance and near vision. That’s why monovision correction was suggested in case of bilateral cataracts. Two techniques were used to perform bilensectomy. A classic technique for PIOL removal was used in 7 of 19 cases. The classic surgical technique included two stages: stage 1, placing corrective lens into the anterior chamber of the eye; stage 2, removing phakic IOL. The former procedure was performed in a “closed” eye through two parentheses, as a rule at 10 and 2 o’clock position. Mydriatic was administered into the anterior chamber (AC); afterwards, AC was filled in with viscoelastic. Removal of posterior chamber (PC) PIOL into the anterior chamber was performed with a spatula bringing from the haptic part of the lens toward the center of the optic in the smallest part of IOL by its dislocation. On completion of PIOL removal into the anterior chamber, PIOL was cut and explanted by parts through 3.5-4-mm corneal tunnel incision (Fig. 1).
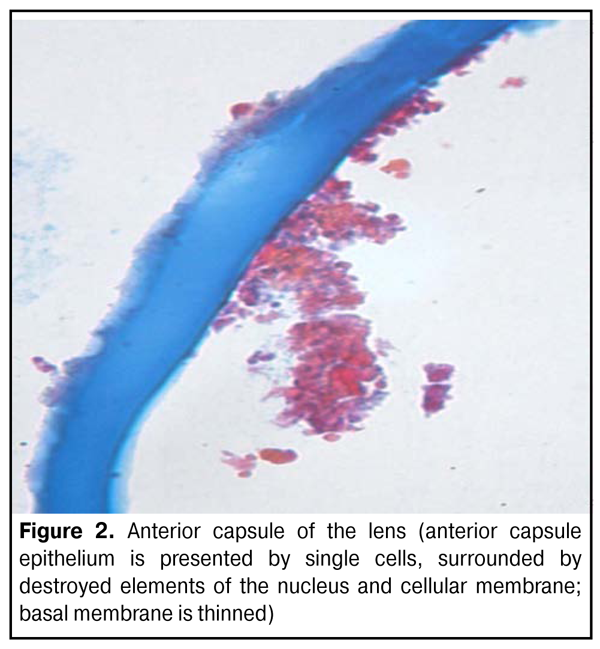
It should be noted that, in three cases of PC PIOL removal, the integrity of anterior capsule of the lens was broken since PIOL was fitting closely to the anterior capsule and the space between the capsule and the lens was filled in with fibrous cells. The presence of fibrous cells was evidenced by further histological and electron microscopic tests (Fig. 2).
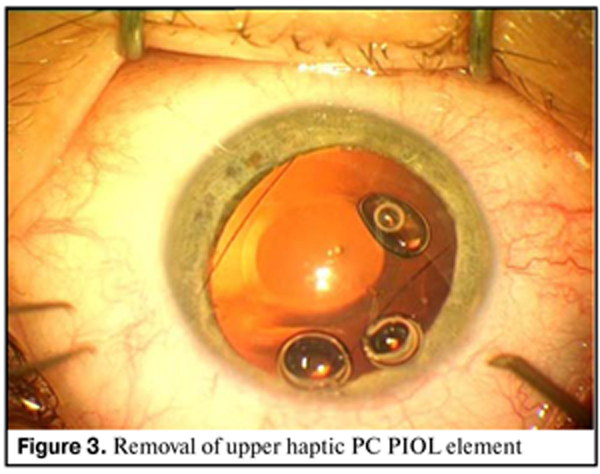
Through the opening obtained, the lens bag content was washed and, afterwards, posterior model of aphakic IOL was implanted. Differential characteristic of cataract developed in the eyes with PIOLs implanted previously is the first degree of lens nucleus density that made it possible not to use ultrasound to destroy it. We developed a three-stage surgical technique which was performed in twelve eyes of 7 patients with PC PIOLs. As opposed to the classic technique, we used more drugs for pain control: muscle relaxants, vasoprotectors, and tranquilizers (taking into account the reintervention). Strong preoperative drug therapy was combined with common local anaesthesia in 10 cases (perilimbal and eye drop anaesthesia in 7 and 3 cases, respectively). Dislocating an upper haptic element of PIOL into the anterior chamber of the eye was the first stage (Fig. 3). The procedure was performed through two paracenteses, as a rule, at 10 and 14 o’clock position on the background of maximal mydriasis and on viscoelastic filling the anterior chamber as aforesaid. Removal of upper haptic element of PC PIOL into the anterior chamber was performed with a spatula bringing from the haptic part of the lens toward the center of the optic in the smallest part of IOL by its dislocation.
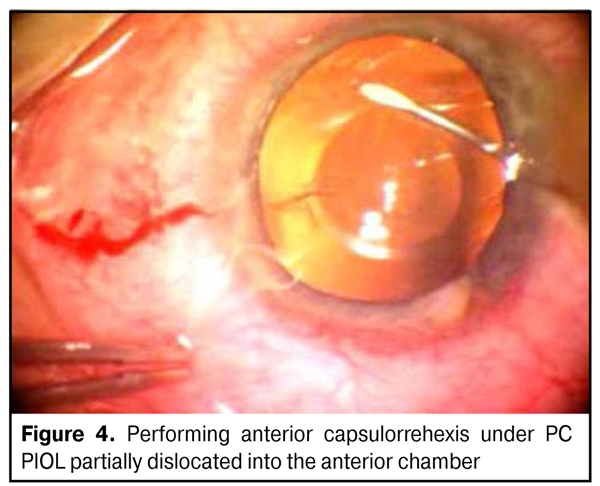
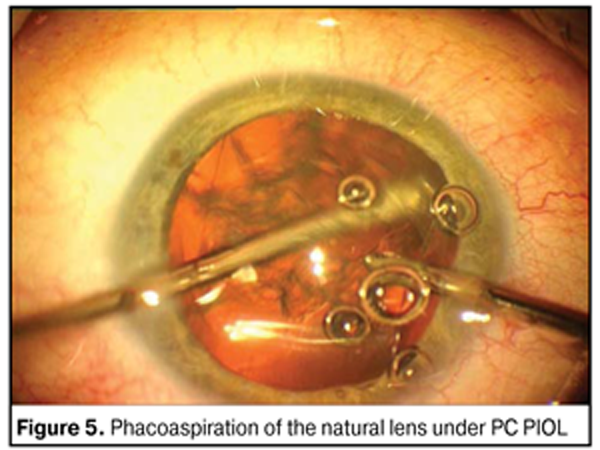
Afterwards, we performed capsulorrhexis under the non-remote PIOL (Fig. 4) and washed cataract-modified lens masses using bimanual handpieces (stage 2) (Fig. 5).
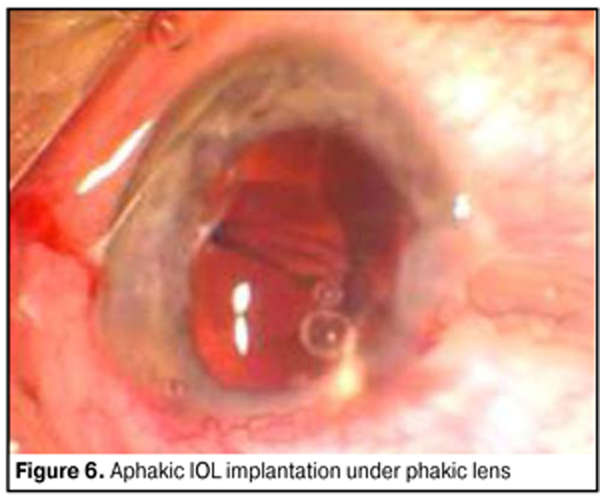
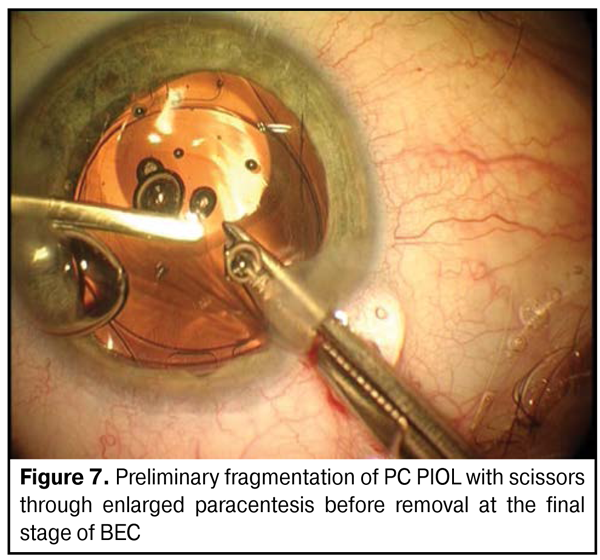
At this stage, procedures under PIOL provide additional protection of endothelium against the background of heavy viscoelastics and decrease traumatization of the eye operated previously by creating two independent boundaries of fluid flow: above and under PIOL. Herewith, boundary volume above PIOL (viscoelastic volume) remains stable that has been proved by a number of experimental studies. The presence of PIOL does not influence the quality of procedures performed at the stage. Afterwards, we enlarged one of the paracenteses to 2.75 mm and implanted aphakic elastic IOL through an injector (Fig. 6) and, thereafter, removed PIOL out of the eye using a thin forceps (Fig. 7).
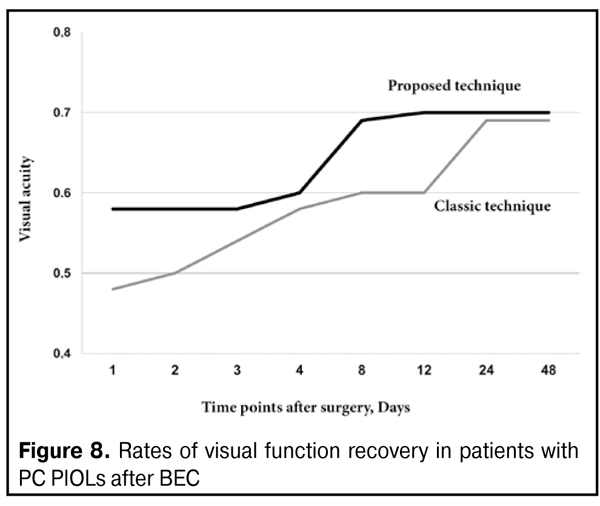
During the postoperative period, each patient was provided anti-inflammatory and vasoprotective, general and local therapy. Results and Discussion All 11 patients (19 eyes) after three-stage surgery had maximum possible visual acuity (from 0.4 to 1.0) which was equal to that after primary correcting PIOL implantation. In general, recovery of visual function was achieved earlier after the three-stage technique as compared to the classic technique. The slowest recovery of maximal visual functions was noted in three eyes of 2 patients (at the end of the third and the beginning of the fourth weeks after surgery) despite the absence of changes in anterior and posterior segments of the eye. Postoperative follow-up of patients ranged from 6 months to 5 years. The state of visual functions was stable during the whole follow-up period. In two years after surgery, YAG laser discission of posterior capsule was performed in 3 of 19 eyes. Endothelial cell loss after bilensectomy in followed up patients averaged 9.1% at time point of two months after surgery. Endothelial cell loss was 11% in 14 eyes at time point of 6 months and increased to 12.2% in 5 eyes at time point of 5 years. There was noted a tendency of a more rapid visual function recovery (on the average, at Day 5 after surgery) (Fig. 8).
All patients were satisfied by results obtained; maximum possible visual functions similar to those after PIOL implantation were achieved in all cases. Conclusions 1.The improved technique for cataract extraction in eyes with PC PIOLs implanted previously is characterized by high functional results and rapid rehabilitation of myopia and hyperopia patients. 2.The technique developed enabled to achieve more rapid recovery of visual functions (on the average at Day 5 after surgery) as compared to the formerly known technique of bilensectomy. References 1.Agafonova VV. [Correction of ametropy via intraocular phakic lens] Thesis of Doctor of Science (Med). М.;2006:354. Russian. 2.Dvali ML. [Intraocular correction of high myopia]. Vestn Oftalmol. 1986 Nov-Dec;102(6):29-31. Russian. 3.Zuev V.K, [Modern aspects of surgical correction of high myopia]. Doctor of Medicine Thesis. Moscow, 1995. 40 p. Russian. 4.Tumanyan ER. [Surgical correction of high degree myopia by minus IOL implantation]. Thesis for Dr. of Sc. (Med). M.; 1998. 353 p. Russian. 5.Caramello G, Di Fortunato R. Three years experience of ICL implantation in high myopia. Congress of the ESCRS, 16th: Abstracts; Nice. 1998. 6.Maliugin BE, Uzunyan DG, Pokrovskiy DF. [Our experience of PIOL Staar for high myopia correction]. Modern Technologies of cataract and refractive surgery – 2008: Paper Collection. M.: 2006; 177-181. Russian. 7.Sorokoletov G.V., Zuyev V.K., Tumanyan E.R., Veshchikova V.N. The first experience of posterior chamber phakic intraocular lens “pIOL-3” in high myopia. Oftalmokhirurgiia. 2013;4:25. Russian. 8.Davidorf JM, Zaldivar R, Oscherow S. Posterior chamber phakic intraocular lens for hyperopia of +4 to +11 diopters. J. Refract. Surg. 1998;14(3):306-11. 9.Dejaco-Ruhswurm I, Scholz U, Pieh S et al. Long-term endothelial changes in phakic eyes with posterior chamber intraocular lenses. J. Cataract Refract. Surg. 2002;28(9):1589-93. 10.Barinov EF, Agafonova VV. [Cause-and-effect approach to the study of complications after phakic intraocular ametropia correction]. Congress of ophthalmologists of Russia, the 8-th Conf.: Proceedings. M.; 2005. 243. Russian. 11.Cоolin J. Bilensectomy: the implication of removing phakic intraocular lenses at the time of cataract extraction. J. Cataract Refract. Surg. 2000; 26(1): 2-3.
|