J.ophthalmol.(Ukraine).2016;2:13-18.
|
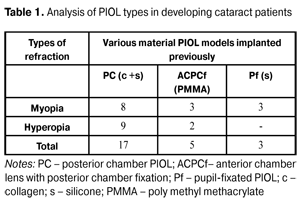
https://doi.org/10.31288/oftalmolzh201621318 Clinical and functional features of the eyes with phakic lenses before and after bilensectomy D.O. Marshava Multiprofile clinics L/J Kutaisi (Georgia) E-mail: marshava-david@mail.ru Introduction. Implantation of phakic intraocular lens (PIOL) is used for high ametropia correction. The insufficiency of PIOL implantation is the development of cataract in the remote terms after surgery due to the contact of constructive elements of PIOL to anterior and posterior eye chamber tissues. The purpose of the present paper was to study clinical and functional features of the eyes with PIOL before and after performing BEC. Material and Methods. 25 eyes of 19 patients with various PIOL models were compared before and after bilensectomy. Results. We confirmed the difference in the character of cataracts developed after implantation of pupil-fixated (Pf) and posterior chamber (PC)PIOLs from cataracts developed after implantation of anterior chamber lens with posterior chamber fixation (ACPCf). There were three degrees of eye reaction after BEC depending on the type of removed PIOL. Conclusions. The course of intra- and postoperative period in BEC depends on pre-existing alterations in the eye. Discordance between a cataract process clinical picture and a PIOL type is an indication for deep investigation of patients. Key words: cataract, phakic intraocular lenses, ultrasound biomicroscopy, bilensectomy Introduction Intraocular correction of ametropia includes two types of interventions: refractive lensectomy and implantation of phakic intraocular lenses (PIOL). Insufficiency of the latter is cataract development in the remote terms after surgery due to the contact of constructive elements of various PIOLs to anterior and posterior eye chamber tissues [1, 2, 3, 4]. It should be noted that PIOL implantation is more often used for ametropia correction in 30-40 y.o. patients [1, 5]. So, the patients, undergone PIOL implantation ametropia correction, find themselves in a state when physiological period of cataract development not only nears but is induced and accelerated by the presence of PIOL [6, 7]. In 2000, J. Colin suggested a term Bilensectomy (BEC) for simultaneous surgery of PIOL explantation, extraction of natural lens with opacity and aphakic lens implantation [8, 9]. Few papers have only reported on the fact of cataract development in PIOL eyes and the need to perform BEC without detailed analysis of intervention-associated processes. The purpose of the present paper was to study clinical and functional features of the eyes with PIOL before and after performing BEC. Material and Methods Bilensectomy was performed in 19 patients (25 eyes), including 8 women and 11 men, aged 28 to 55, which were implanted PIOL various models of collagen copolymer (c), silicone (s) and poly methyl methacrylate (PMMA). High hyperopia was corrected by PIOL implantation in 11 eyes (8 patients); and cataract development was observed at terms of 5 to 7 years after refractive surgery. High myopia was corrected by PIOL implantation in 14 eyes (11 patients); and cataract development was observed at terms of 6 to 13 years after implantation (Table 1).
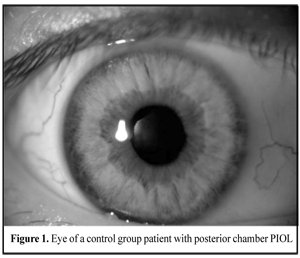
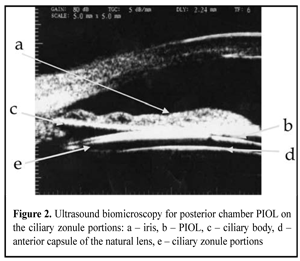
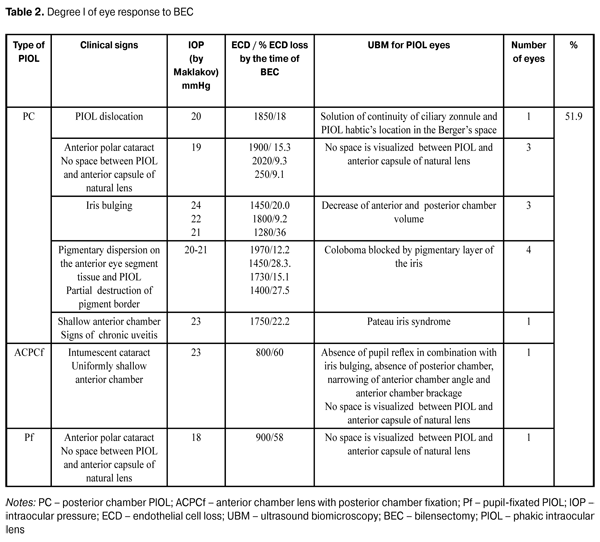
In addition to standard refractive examination, we studied the state of hydrodynamics and endothelial cell density (ECD). Ultrasound biomicroscopy (UBM) was performed in each patient. When performing UBM, we draw attention to the size and evenness of the anterior chamber (AC), PIOL location, and studied optic contact of PIOL to the natural lens anterior capsule and haptic contact to ciliary body and processes. Intensity of the eye response to BEC was scored according to three degrees as follows. I degree: the eye is clinically quiet; the cornea is transparent; pupil light response is preserved; there is no tyndallization of anterior chamber aqueous humor, exudation or reactions from posterior eye segment. II degree: moderate response of the eye, mild edema and descemetitis of the cornea are detected; light response is poor; tyndallization of anterior chamber aqueous humor (anterior chamber flare and presence of inflammatory cell elements) is noted; posterior eye segment reaction is not observed. III degree: apparent response of the eye, gross descemetitis corneal folds, corneal edema and tyndallization of anterior chamber aqueous humor are observed; pupil light response is poor; exudative reaction can be seen as well as posterior eye segment alterations as exudative fibers in the site of the pupil. To detect cataract development risk factors in the eyes with implanted PIOLs, 11 patients with various models of PIOLs without cataract development at term of 7 and more years after surgery were observed as controls. Thus, there were 7 minus PIOL including 4 posterior chamber lenses and 3 anterior chamber lenses with posterior chamber fixation and 4 plus PIOL including 3 posterior chamber lenses and 1 anterior chamber lens with posterior chamber fixation. Results and Discussion Analyzing the clinical materials we did not reveal dependence of cataract progression rate on the type of PIOL material, size of anterior-posterior axis and patient’s age. We confirmed the difference in character of cataract progression after implantation of pupil-fixated (Pf) and posterior chamber (PC) PIOL from cataracts developed after anterior chamber lens with posterior chamber fixation (ACPCf) implantation. Thus, cataract alterations were in the anterior capsule and anterior layers of the lens when Pf and PC PIOLs were used; whilst ACPCf-associated alterations were located in the posterior cortical layers [1, 10, 7]. Posterior polar cataract progression is related to trophic disturbances in the area of the ciliary body and ciliary zonule; this was confirmed by the follow up of two patients, in which posterior polar cataract had developed at time point of 10 years after PC PIOL implantation. On standard examination, PC PIOL had a correct position. On performing UBM, we observed solution of continuity of portions in ciliary zonule against upper haptic element and occasional dislocation of the latter into the Berger’s space. Clinical pictures of the eyes with and without cataract development were different. In a group of patients without cataract, all PIOL models were centered along the visual axis with quiet eyes and without inflammation signs. Space was visualized between PIOL and the anterior capsule of the lens, pupil light response was preserved; insignificant pigment dispersion on the anterior chamber tissues was noted in two cases, hydrodynamic indices were within the normal range, ECD ranged from 9 to 22%. UBM of these eyes were similar; thus, ACPCf PIOL haptic elements were placed in the ciliary sulcus and PC PIOLs were placed symmetrically on the ciliary sulcus or on the ciliary zonule portions. Herewith, gap space of more than 70 mkm was visualized between anterior capsule of the lens and phakic IOL; anterior chamber angle (ACA) was open and synechia was not detected (Fig.1, 2).
Clinical picture and UBM for cataract eyes were much variable. Best corrected visual acuity in patients before BEC varied from 0.04 to 0.5; intraocular pressure (IOL) by Maklakov was compensated and within the range of 16-23 Mmhg (local antihypertensive drug was used in 4 of 25 eyes); endotelial cell density (ECD) in the central area of the cornea ranged from 500 to 2450 kl/mm2 (at this, ECD loss rate varied from 9.1 to 60%). The technique of small and medium tunnel incision depending on PIOL type was used to perform BEC to patients with Pf and PC PIOLs. Anterior chamber intraocular lens with posterior chamber fixation (ACPCf) was preliminary screwed into the anterior chamber to make it possible to be removed through a 6 mm corneascleral incision. Intraoperative floppy iris was noted in 3 patients with Pf and PC PIOLs and instability of anterior chamber parameters was noted in 1 patient. Those features were noted in 2 eyes of a plateau iris syndrome patient and in 1 eye of a chronic uveitis patient (Fig. 1) (Table 2).
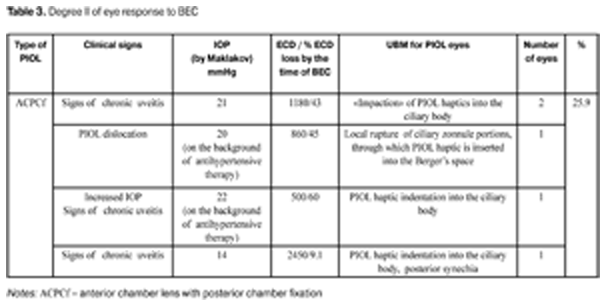
Intraoperatively, anterior chamber parameters were instable apparently in 2 cases and the iris was interposed into surgical incision in 1 case of ACPCf patients on the background of high hyperopia in combination with plateau iris and anterior position of ciliary processes. It appears that PIOL haptic indentation into the ciliary body results in reflex and chronic disorders in ciliary process microcirculation, damage in aqueous humor production, influencing both intra and post bilensectomy (degree II of postoperative reaction) (Fig. 4) (Table 3).
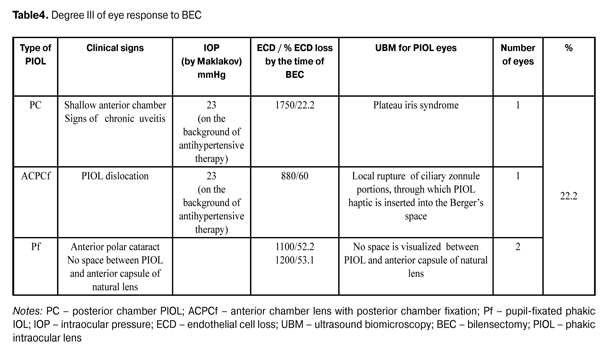
Pigmentary dispersion on the anterior eye segment tissues and PIOL was noted in 4 patients. Pigmentary dispersion was associated to partial destruction of pigmentary layer of the iris; no hydrodynamic disorders were noted both before and after BEC. However, as compared to the pair eye, asymmetry of IOP data by Makhlakov was revealed including higher level in the eyes studied in combination with increased production; this can be associated with reflex stimulation of posterior eye chamber tissues. During BEC at the stage of PIOl removal to the anterior chamber, “Spontaneous capsulorexis” in the site of complete contact between the lens and natural lens anterior capsule was noted in 3 PC PIOL patients in whom a space between PIOL and anterior capsule of the natural lens was not visualized. Intensity of BEC reaction in the operated eye achieved the maximal level in 18-24 hours after the operation. Despite the variety of UBM picture in patients with Degree II and III eye response to BEC, each case was characterized by appearance of chronic uveitis; and the most expressed reaction was noted in patients with IOP subcompensation. It can be assumed that this fact is associated with endotheliocyte hypoxia, which accompanies a surgical wound and forces long-term morphological and functional alterations in the PIOL eye. The latter can be caused by disturbance between blood-aqueous barrier receptors responsible for the volume and content of the humor. In particular, when vasoconstrictor (endothelin-1, prostaglandin F2?) effect prevails vasodepressor (nitric oxide, prostaglandin E, prostacyclin) effect, oxygen partial pressure (рО2) and oxidation substrate level in endothelial cells are decreased, followed by their dystrophy [6, 11]. It is likely that appearance of chronic uveitis and ciliary body stimulation occurred in them conditions aqueous humor outflow obstruction, followed by IOP increase, and enhances endothelium damage and corneal edema. However, one patient with chronic uveitis and endothelial cell loss of 1180 cell/mm2 had degree II of eye response to BEC; while another patient with PIOL haptics impacted into the ciliary body and endothelial cell loss of 800 cell/mm2 had degree I of eye response to BEC. In our opinion, this reflexes the individual reactivity of the human, and specification of its evidences, or criteria, will allow us to predict the course of postoperative period and patient management. Degree II of eye response to BEC was expected to appear in one patient, despite the high level of ECL, since he had nerve fiber thickening and corneal stromal degenerative process as compared to the pair eye (Fig. 5) (Table 4). Inspite of the high loss of endothelial cells, the alterations detected evidenced the corneal decompensation, and BEC was a trigger for the further development of pathological process.
It should be noted that when analyzing the dependence of postoperative eye response intensity on the PIOL model, there were always detected degree II or III after ACPCf PIOL implantation. The above analysis of outcomes of 25 surgeries show that it is relevant for a clinician to separate 3 groups of patients according to 3 degrees of postoperative response intensity as follows: patients without chronic uveitis, patients with chronic uveitis and patients with subcompensated IOP on the background of chronic uveitis. Visual functions were managed to recover after BEC in 22/25 eyes, the former were equal to those after PIOL implantation. The postoperative follow up ranged from 6 month to 3 years. Visual functions of patients remained stable. However, in a year after BEC, posterior capsule fibrosis associated YAG laser discussion of the posterior capsule was performed in 4 eyes. Afterwards, 3 of 25 patients (11.1%) underwent penetrating keratoplasty. No specific morphological clinical signs of eye response to various PIOL models were revealed. Data obtained by us prove the necessity of deep and detailed examination using up-to-date diagnostic methods for PIOL patients before BEC; thereby, it can be possible to foresee the postoperative response intensity. Conclusion 1.The course of intra- and postoperative period in BEC depends on pre-existing alterations in the eye. BEC is a trigger forcing long-term prior morphological functional changes in PIOL eyes. 2.Discordance between cataract process clinical picture and PIOL type is an indication for deep investigation of patients to make it possible to reveal extra risk factors. 3.Complete contact of posterior chamber PIOL with lens anterior capsule is a risk factor in terms of possibility of intraoperative spontaneous capsulorexis. 4.BEC response is of individual gradual character, intensity of which can be characterized by three degrees according to changes in eye chambers and hydrodynamic parameters. 5.A risk factor for pathological eye response after BEC is a long-term contact of haptic of various PIOL types with ciliary body or processes. References 1.Agafonova VV. [Correction of ametropy via intraocular phakic lens] Thesis of Doctor of Science (Med). М.;2006:204. Russian. 2.Tumanyan ER. [Clinical and functional state of the eyes after minus IOL implantation]: Thesis for Doctor of Sc. (Med). M.; 1998. 353 p. 3.Bosc J. Cataract Surgery in eyes with anterior chamber phakic intraocular lenses- Techniques and problems. ASCRS Symposium on Cataract IOL and Refractive Surgery. Preview Program. 2008. 4.Bosc J, Horodynska D, Rajerison S, Sander M. Cataract surgery in eyes with anterior chamber phakic intraocular lenses - techniques and problems. XXIV Congress of the ESCRS. Stockholm, 2007. 5.Tumanyan ER. [Surgical correction of high degree myopia by minus IOL implantation]. Thesis for Cand. of Sc. (Med). M.; 1987. 132 p. Russian. 6.Barinov EF, Agafonova VV. [Cause-and-effect approach to the study of complications after phakic intraocular ametropia correction]. Congress of ophthalmologists of Russia, the 8-th Conf.: Proceedings. M.; 2005. 243. Russian. 7.Fedorov SN, Zuev VK, Tumanyan NR, Suheil AJ. Clinical and functional follow-up of minus IOL implantation in high-grade myopia. Oftalmokhirurgiia. 1993;2:12-7. Russian. 8.Colin J., Bilensectomy: The implications of removing phakic intraocular lenses at the time of cataract extraction. J. Cataract Refract. Surg. 2000;26(1):2-3. 9.Cochener B. Implatation of Multifocal IOLs after Cataract Extraction in Highly Myopic Patients with and Without Previous Phakic IOL Removal. ASCRS Symposium on Cataract IOL and Refractive Surgery. Preview Program. 2008. 10.Al Jumaa Suheil. [Analysis of long-term clinical and functional results of minus IOL implantation in high degree myopia]. Author abstract for Cand. of Sc. (Med). M.; 1992. 21 p. Russian. 11.Almazov VA, Petrishchev NN, Shlykhto EV, Leontyeva NV. [Clinical pathological physiology]. M.; 1999. 464 p. Russian.
|