J.ophthalmol.(Ukraine).2016;2:44-46.
|
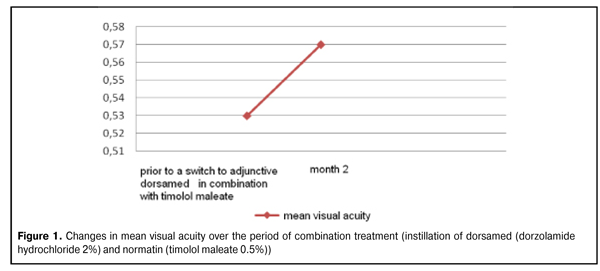
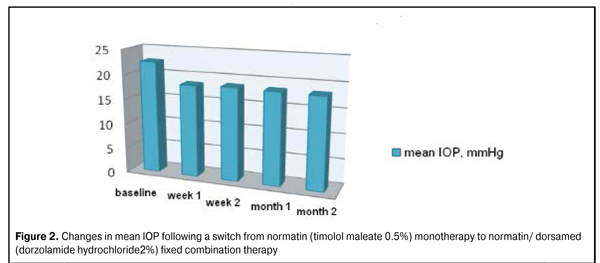
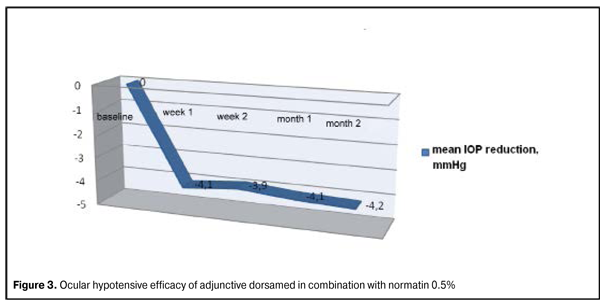
https://doi.org/10.31288/oftalmolzh201624446 Evaluation of efficacy of dorsamed in combination with timolol 0.5% in the treatment of primary open-angle glaucoma G.O. Kliuiev, Cand Sc (Med) V.V. Golovkin, Cand Sc (Med) Health Technology Ltd Odessa (Ukraine) Introduction Globally, the number of people with glaucoma is estimated to reach 79.5 million by 2020, and 74% of them are expected to have primary open-angle glaucoma (POAG). Every tenth glaucoma patient in the world today has become blind. Therefore, prevention and treatment of glaucoma is a medical and social issue of great importance. Although multiple laser and surgical techniques are available for management of POAG, these treatment measures are not always found to be effective. The conservative approach in the treatment of glaucoma is one of the most commonly used and least traumatic [1-3]. The current view is that POAG is a progressive optic neuropathy associated with a number of factors, one of the most important being elevated intraocular pressure (IOP) [4, 5]. Studies in the pathogenesis of POAG have shown that alterations in aqueous outflow and an increase in IOP to an intolerable level are essential in the development of glaucomatous optic neuropathy [5]. Carbonic anhydrase inhibitors are known to prevent formation of carbonic acid with a decrease in a production of (НСО3–) ions. Ionic (НСО3–) deficiency results in increased cationic gradient with the following reduction in aqueous secretion. Dorsamed (dorzolamide 2%) is a topical carbonic anhydrase inhibitor with good bioavailability, high selectivity and potent hypotensive effect. A need for adjunctive hypotensive medications to normalize the IOP has been reported in 27% to 33% of glaucoma and ocular hypertension patients treated monotherapeutically for this condition [6]. Combining two synergistic classes of antihypertensive drugs (which have different mechanisms of action) is the most common current approach to therapy for glaucoma. The study purpose was to assess the efficacy of dorsamed (dorzolamide hydrochloride 2%; World Medicine Ophthalmics Ltd, UK) in combination with normatin (timolol maleate 0.5%; World Medicine Ophthalmics Ltd) in the treatment of primary open-angle glaucoma. Materials and Methods The study group included POAG patients who had been using timolol maleate 0.5% only (topical instillation, two times a day) for two weeks at least. An additional inclusion criterion was IOP greater than normal (20-21 mmHg) because the above mentioned duration did not make it possible to assess tolerance to the drug’s ocular hypotensive effects. Moreover, patients enrolled had to have close IOP values at baseline to facilitate statistical significance. Patients with concomitant ocular disease were excluded. The Goldmann applanation tonometer was used to measure the true IOP (P0). At baseline, topical timolol maleate was supplemented with dorsamed (dorzolamide 2%; two times daily, in the morning and evening). IOP measurements were taken from 11 AM to 1 PM at 1 week, 2 weeks, 1 month and, finally, 2 months after baseline. At baseline, the mean P0 value was 22.5 ± 1.19 mmHg, and the mean corrected visual acuity was 0.53 ± 0.30 (range, 0.1 to 1.0). Humphrey perimetry was used to determine the stage of glaucoma. The change in visual function was determined at 2 months time point. Ocular and systemic tolerance and comfort are important points in administration of dorzolamide and timolol maleate. Ocular burning, itching, pricking and transient blurred vision after instillation have been reported to be the most frequent side effects associated with topical carbonic anhydrase inhibitors [6]. Any systemic complaints such as changes in arterial pressure, heart rate and breathing function were reported on each patient’s study form to facilitate the assessment of systemic tolerance. Glaucoma stage I was found in 19 eyes, stage II in 8 eyes, and stage III in 3 eyes. Results and Discussion Changes in mean IOP (Ро) over time At day 7 of combination treatment (twice a day instillation of normatin and dorsamed), the reduction from baseline in mean IOP was 4.1 mmHg (18.4%; from 22.5 ± 1.19 mmHg to 18.4 ± 1.07 mmHg). At week 2, month 1 and month 2 (the last time point), the reduction from baseline in mean IOP was 3.9 mmHg (17.5%), 4.1 mmHg (18%), and 4.2 mmHg (18.6%), respectively. Changes in visual function over time At month 2 of combination treatment with normatin and dorsamed, the MD (mean deviation) and pattern standard deviation (PSD), as measured by Humphrey perimetry, were somewhat improved from baseline. Over this two-month period, the mean visual acuity statistically insignificantly increased from 0.53 ± 0.30 to 0.57 ± 0.31 (Fig. 1).
Figure 2 presents changes in mean IOP following a switch from normatin (timolol maleate 0.5%) monotherapy to normatin/ dorsamed (dorzolamide hydrochloride 2%) fixed combination therapy. Figure 3 demonstrates the ocular hypotensive efficacy of adjunctive dorsamed in combination with normatin 0.5% (twice a day instillation).
A month after a switch to the combination of normatin and dorsamed, ocular discomfort was assessed based on the frequency of above mentioned side effects of administration of topical carbonic anhydrase inhibitors. No patient complained of severe or very severe ocular discomfort. Most of patients (17/22) did not complain of any discomfort following a switch to the combination therapy involving adjunctive dorsamed. Two out of 22 patients complained of appearance of systemic side effects at month 1 and of worsening of these effects at month 2. It should be noted that both these patients had a history of severe systemic disease (coronary arterial disease, cardiac infarction) which could contribute in some way to increased complaints. Conclusion First, in POAG patients with elevated IOP, a switch from monotherapy to combination therapy (normatin with adjunctive dorsamed) resulted in the 18.4% reduction from baseline in mean IOP, evidencing a potent hypotensive effect of topical dorsamed as adjunctive therapy to a beta blocker (normatin). Second, the mean deviation and pattern standard deviation, as measured by Humphrey perimetry, and the mean visual acuity somewhat improved from baseline at month 2 of combination treatment with normatin and dorsamed, this being an indicator of stabilization of glaucoma. Finally, in POAG patients, a combination of normatin and dorsamed demonstrated good ocular and systemic tolerance. References 1.Alifanova TA, Alifanov IS, Zosimova IaO et al. [Epidemiological aspects of disability due to ocular disorders in Ukraine]. In: [Proceedings of the International Conference on the 100th Anniversary of Acad. Puchkovskaya, on Current Aspects of Clinical Picture, Diagnosis and Treatment of Ocular Disease]; 2008 May 29-30; Odessa, Ukraine: Filatov Institute of Eye Disease; 2008. p.5. Ukrainian 2.Alifanova TA, Gladchenko IuIu, Chuiko OL. [Disability due to ocular disorders in Ukraine]. In: [Filatov Memorial Lectures: Proceedings of the International Ophthalmological Conference on the 75th Anniversary of the Filatov Institute]; 2011 May 26-27; Odessa, Ukraine: Filatov Institute of Eye Disease; 2011. p.340. Ukrainian 3.Zhaboedov GD. [Current aspects of the pathogenesis, clinical picture, and treatment of open-angle glaucoma]. Pharm Bull. 1999;1-2:2-7. Russian 4.Krasnov MM. [Microsurgery for glaucoma]. 2nd ed. Moscow: Meditsina; 1980. 248 p. Russian 5.Nesterov AP. [Glaucoma: pathogenesis and treatment principles]. In: [Proceedings of the 7th Russian National Ophthalmology Conference]; 2000 May 16-20; Moscow: Eye Microsurgery Federal State Institution; 2000. p.87-91. Russian 6.Khlobystov AA, Egorov EA, Stavitskaya TV. [Brinzolamide: a novel carbonic anhydrase inhibitor]. Clin Ophthalmol. 2001;2(2):51-4. Russian
|