J.ophthalmol.(Ukraine).2016;1:31-35.
|
https://doi.org/10.31288/oftalmolzh201613135 Results of research of brain-derived neurotrophic factor level (BDNF) in the vitreous body of patients with proliferative diabetic retinopathy A.A. Putienko, Doctor of Medical Sciences Elhadj Emhamed Ali E.V. Kovaleva Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: aputienko@ya.ru Introduction. Progression of the optic nerve neuropathy of diabetic genesis is currently associated with the neurotrophic factors dysfunction, in particular, brain-derived neurotrophic factor (BDNF), since it has a pronounced neuroprotective properties and plays an important role in retinal ganglion cells and their axons protection. The last studies have shown that BDNF level in blood plasma and lacrimal fluid in patients with diabetes mellitus is reduced both at non-proliferative and proliferative stages of the disease, but in the latter case, it is more expressed. The level of this factor in the vitreous body in patients with proliferative diabetic retinopathy (PDRP), who have received the intravitreal interventions, has been studied by some authors on the small number of observations. Purpose: To study the correlation between the level of BDNF in the vitreal content in PDRP-patients and certain electrophysiological indicators, characterizing the degree of the optic nerve neuropathy. Material and Methods. 70 patients with PDRP (70 eyes) were observed with positive treatment results riched after the intravitreal anatomic intervention. A haemophthalmos without epiretinal tissue was in 35 eyes (50.0%). 28 eyes (40.0%) had partial or total haemophthalmos with epiretinal membranes and traction retinal detachment. Among them, there were 38 women and 32 men. The average age of the patients was (55.7 ± 12.7). Results. The average level of the brain-derived neurotrophic factor (BDNF) in the vitreous body totalled 12.56 SD (6.32) pg/ml. BDNF content in patients with haemophthalmos was significantly higher than in patients with tractional macular detachment and traction-rhegmatogenous retinal detachment (t = 2.58, p = 0.012; t = 2.06, p = 0.045), respectively. In this, it depended on the type of diabetes, hypertensive disease, the degree of diabetes mellitus compensation and panretinal laser coagulation performance. In the study of visual evoked potentials (VEP) against flash 2 Hz and 12 Hz the latency and the amplitude of P1 prong were not reliably differing concerning the median values (> 11.42 pg/mL) BNDF level in the vitreous body. Wherein the study of VEP against patterns 1 ° and 0 ° 15 ' showed reliable reduction of the P100 wave amplitude in patients with lower BDNF (t = 2.13, p = 0.037; t = 2.97, p = 0.004). Between the level of BDNF in the vitreous body and Р100 wave amplitude against the pattern 1° (R = 0.6132, p = 0.0397) and 0° 15 ' (R =0.6724, p = 0.0232) there was found a strong direct correlation. The work also shows that the content of BDNF in the vitreous body in patients with visual acuity of 0.01-0.09 achieved after intravitreal interventions were significantly lower compared with 0.3-1.0 acuity (t = 2.13, p = 0.039). Conclusion. Thereby, with the proliferative changes progression in patients with PDRP, the level of BDNF in the vitreal cavity is reliably decreasing, which can lead to the emergence of neurodystrophic processes in the retina and the optic nerve, i.e. neuropathy. VEP pattern indicators to a certain extent reflect its content in the tissues of the eye and can be used in further research aimed to correct this compound in patients with PDRP. Key words:proliferative diabetic retinopathy, neurotrophic factor, vitreous body
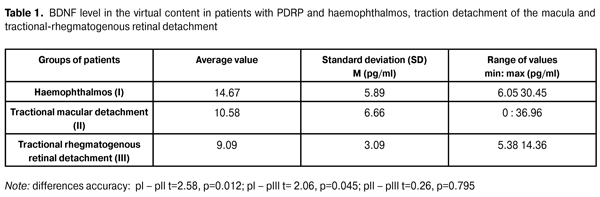
Introduction Proliferative diabetic retinopathy (PDRP) vitreal surgery has strongly entered the ophthalmic surgeons practice, providing high anatomical results of treatment up to 90% of cases [9, 11]. At the same time, the functional treatment results remain significantly low [3, 4, 9, 11]. According to B. Gupta et al. [4], visual acuity improvement after the intravitreal procedures in patients with tractional macular detachment is reached in only 70% of cases, which can be caused by the expressed source degree of neurodegenerative changes of retina and optic nerve. Progression of the optic nerve neuropathy of diabetic genesis is currently associated with the neurotrophic factors dysfunction (in particular, brain-derived neurotrophic factor –BDNF) since BDNF has a pronounced neuroprotective properties and plays an important role in retinal ganglion cells and their axons protection. BDNF is expressed in glial and neuronal cells and predominantly affects the development and functional activity of neurons in the optic path [1, 2, 5, 10]. At the present time, a number of studies on BDNF level in blood plasma and lacrimal fluid in patients with diabetes mellitus have been conducted. It has been found that its content is reduced both at non-proliferative and proliferative stages of the disease. In the latter case it is more expressed [1, 6, 7, 8]. In the literature, there are individual works based on a small number of observations and dedicated to the study of this factor level in the vitreous body of PDRP-patients, receiving intravitreal interventions [2, 5]. Its role in the optic nerve neuropathy of diabetic genesis depending on the stage of PDRP progression is of main interest. Purpose of the study. To study the correlation between the level of BDNF in the vitreal content in PDRP-patients and electrophysiological indicators, characterizing the degree of the optic nerve neuropathy. Material and Methods 70 patients with PDRP (70 eyes) were observed with positive treatment results riched after the intravitreal anatomic intervention. A haemophthalmos without epiretinal tissue was an indication for vitrectomy of 35 eyes (50.0%). 28 eyes (40.0%) partial or total haemophthalmos with epiretinal membranes and traction retinal detachment, which has extended to the macula area. 7 (10.0%) eyes tractional-rhegmatogenous retinal detachment. Among them, there were 38 women and 32 men. The average age of the patients was 55.7 SD (12.7) years. Type I diabetes was observed in 12 cases (17.1%), and type II diabetes in 58 cases (82.9%). Diabetes duration averaged 18 SD (7.4) years. At the stage of compensation, which was evaluated by the fluctuations in blood glucose levels per day, the presence or absence of glucose and protein in the urine was in 50 patients (71.4%), the stage of subcompensation – 20 patients (28.6%). 18 patients (31.4%) had hypertensive heart disease. Proliferative process duration ranged from 10 to 32 months and averaged 17.2 SD (5.8) months. Panretinal laser coagulation previously was performed for 62 (88.6%) eyes. IOP level fluctuated within normal limits in all eyes. Intravitreal interventions were performed according to conventional techniques, after performing subtotal vitrectomy, epiretinal membranes were removed as much as possible, if necessary, to unfold the retina to the eye cavity, the sterile air was injected, panretinal endodiode laser coagulation and anticoagulation of retinal tear were performed. In the group of patients with the only haemophthalmos in 8 cases (22.9%) the operation was completed by sterile air tamponade, 12 eyes (34.3%) by 10% perfluoropropene gas-air mixture tamponade and 15 eyes (42.8%) by 20% perfluoropropene gas-air mixture tamponade. In the group of patients with a tractional macular detachment in most cases, 24 eyes (85.7%) the operation was completed by 20% perfluoropropene gas-air mixture tamponade and only 4 cases (14.3%) by 10% perfluoropropene gas-air mixture tamponade. In patients with traction-rhegmatogenous retinal detachment in all cases 20% perfluoropropene gas-air mixture was used. Initial visual acuity in patients with haemophthalmos distributed from light perception to 0.05, and in most cases – 27 eyes (77.1%) – was equal 0.01. In patients with tractional macular detachment, it distributed from light perception to 0.25 with the highest occurrence frequency of 0.01-0.03 – 20 (71.4%) eyes. In patients with traction-rhegmatogenous retinal detachment, the initial visual acuity ranged from light perception to 0.35. Neuropathy degree was evaluated by visual evoked potentials level (VEP) against the flashes of 2 Hz and 12 Hz and the patterns of 1° and 0°15?. BDNF level was determined in vitreal content, which was obtained during early vitrectomy with closed irrigation, sampling 0.2-0.3 ml of research material to the container. Samples obtained were stored at -20° C prior to the research. The content of BDNF was determined by enzyme-linked immunosorbent assay using a reagent kit for its quantitative determination (manufacturer R & D SYSTEMS, USA) according to the attached instructions. Evaluation of the results was carried out photometrically with a microtiter enzyme immunoassay analyzer Stat Fax 2100. Statistical processing was performed using the application package STATISTICA v7.0. The comparison was made with Student's coefficient (t) and non-parametric criterion ?2. Spearman coefficient (R) was used in the correlation research. Critical significance level when testing statistical hypotheses was accepted equal to 0.05. Results and Discussion BDNF level in PDRP-patients' vitreal content equaled 12.56 pg/ml with a standard deviation of 6.32. The data distributed from 0 to 36.96 pg/ml. The median was 11.42 pg/ml. BDNF level study in the vitreal content of patients with diabetes types I and II did not reveal reliable differences. Thus, in patients with type I diabetes, BDNF level amounted to 10.48 pg/ml, and in patients with type II diabetes, it was 14.88 pg/ml, t = 1.78, p = 0.079. The content of BDNF also did not reliably differ depending on the presence or absence of hypertensive disease 12.64 pg/ml and 13.89 pg/ml, t = 0.69, p = 0.571 respectively. At the same time, the research of the level of this compound, depending on the duration of the proliferative process, showed that in patients with proliferative changes over 18 months, BDNF level was significantly lower and amounted to 11.02 pg/ml towards 15.01 pg/mL in patients with proliferative process in the vitreous cavity of 18 months and less t = 2.08, p = 0.041. The work also analyses the content of BDNF in the vitreous body, depending on the degree of compensation of diabetes mellitus. Thus, in patients with subcompensated diabetes BDNF content was 11.91 pg/ml, and in patients with compensation stage of diabetes – 14.64 pg/ml, the data is not reliable statistically (t = 1,28 , p = 0.237). Implementation of panretinal laser coagulation also did not significantly influence the content of this compound in the vitreous cavity t = 0.87, p = 0.377. The data on BDNF level in the virtual content in patients with PDRP and haemophthalmos, traction detachment of the macula and tractional-rhegmatogenous retinal detachment is shown in Table 1.
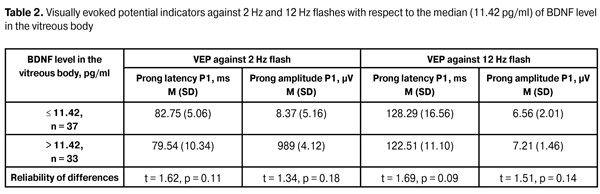
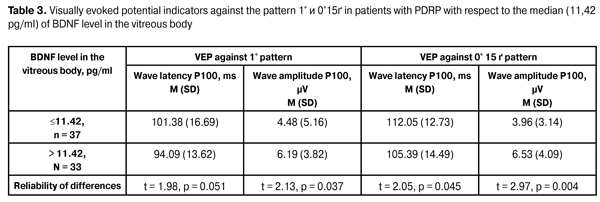
As we can see from the data in the table, the content of BDNF in the vitreous content in patients with haemophthalmos does reliably exceed the level of this compound in vitreal content in patients both with tractional retinal detachment, and tractional-rhegmatogenous. It shows that with proliferative changes progression in the retina, BNDF level in the vitreal cavity is reduced, which can contribute neurodystrophic processes in the retina and optic nerve progression. Studying the dependence between the electrophysiological indicators number, characterising optic nerve neuropathy degree in PDRP-patients, having received the intravitreal interventions, and BDNF level in the vitreous body, are presented in tables 2 and 3.
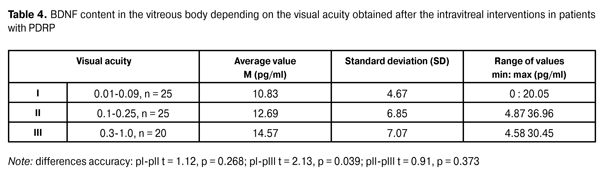
As it can be seen from the data in the table, in PDRP-patients who received intravitreal interventions, the latency and the amplitude of P1 prong during visually evoked potential researching against 2 Hz flash did not differ reliably regarding the median values (> 11.42 pg/mL) of BDNF level in the vitreous body. At that, a clear tendency towards reducing the prong amplitude P1 in patients with a lower content of BDNF can be noted. VEP indicators against 12 Hz flash showed pronounced changes in studied patients compared to the normal value both by latency and the amplitude of the prong P1. However no significant differences with respect to the median level of BDNF in the vitreous body were detected. There was registered a clear tendency towards latency prolongation and amplitude reduction of P1 prong in patients with lower BNDF content in the vitreous body during 12 Hz flash test. Thus, the results of the studies of VEP against 12 Hz showed a decrease of the response of the visual system from the retina to the visual cortex in patients with PDRP, not reflecting at the same time the level of BDNF in the vitreous body. VEP test against pattern 1° did not show the reliable differences in the latency of the wave Р100 in cases with BDNF content in the vitreous body relative to the mid-point. In this, the value of P100 wave amplitude showed a significant reduction of this indicator in patients with a lower content of BDNF. It shows that the decrease in BDNF level in the vitreous body is associated with the reduced functional activity of neurons in the retina and the entire visual system leading to the visual cortex. There also was noted a significant reduction in P100 wave amplitude against the pattern 0°15? in general in patients with PDRP, as well as in the test against the pattern 1°, revealed a significant decrease of this indicator in cases with lower studied neurotrophic factor in the vitreous body relative to the mid-point. These data indicate the pronounced response reduction in visual cortex area, responsible for the macula area. Thereby, the studies performed show that one of the mechanisms of the development of optic nerve neuropathy in patients with PDRP is the lowered BNDF level in the tissues of the eye. The research of the dependency between the level of BDNF in the vitreous body and VEP pattern indicators revealed a correlation between the amplitude of the wave Р100 against the pattern 1° (R = 0.6132, p = 0.0397) and the latency and the amplitude of the wave Р100 against the pattern 0° 15 ? (R = 0.6068, p = 0.0426 and R =0.6724, p = 0.0232). Thereby, there is a clear regularity: lower is the level of BNDF in the vitreous body, the lower is the amplitude of the P100 wave against the pattern 1 ° and the higher is the latency and the lower is P100 wave amplitude against the pattern 0 ° 15'. The dynamics of the visual acuity after the intravitreal procedures in patients with PDRP showed a significant improvement of visual functions. The number of eyes with visual acuity under 0.09 was reduced from 56 to 26 (?2 = 28,15, p = 0.000). Wherein in patients with haemophthalmos the visual acuity was significantly higher and amounted to 0.32 (0.24) against 0.1 (0.13) in patients with tractional macular detachment (t = 4.45, p = 0.001). There also was authentically registered the higher visual acuity in patients with haemophthalmos 0.32 (0.24) compared to the patients with traction-rhegmatogenous detachment of the retina 0.12 (0.07) (t = 2.25, p = 0.030). There were no reliable differences in visual acuity in patients with tractional detachment 0.1 (0.13) and traction-rhegmatogenous detachment of the retina 0.12 (0.07) registered (t = 0.35, p = 0.728). BDNF content in the vitreous body at different indicators of visual acuity, obtained after intravitreal interventions in patients with PDRP, is shown in Table 4.
The data obtained indicates on reliably lower BDNF in the vitreous body in patients with visual acuity of 0.01 - 0.09, compared with the visual acuity of 0.3 - 1.0. Thereby, BDNF low content in ocular tissues, which is one of the leading causes of optic nerve neuropathy progression, leads to reliably lower functional results of intravitreal interventions in patients with PDRP. The research conducted hereby allows us to conclude, that BNDF level in the vitreous body of PDRP-patients is 12.56 pg/ml and is decreasing with proliferative process progression. In patients with proliferative changes lasting more than 18 months, the level of this compound is significantly lower. Proliferative changes progression prior to the tractional macular detachment and traction-rhegmatogenous retinal detachment is accompanied with a reliable reduction in BNDF level in the vitreous body. Between the level of BDNF in the vitreous body and VEP pattern there is a strong correlation, indicating on that VEP pattern indicators in some degree are reflecting the content of this compound in the tissues of the eye.
References
1.Gavrilova NA, Lanevskaya NI, Bakaeva LM. [Effect of brain-derived neurotrophic factor - BDNF on the organotypic cultures of the retina]. Ofthalkhirurgiia. 2009;1:36-42. Russian.
2.Abu El-Asrar M, Dralands L, Missotten L. Expression of apoptosis markers in the retinas of human subjects with diabetes. Invest Ophthalmol and Vis Sci. 2004;45(8):2760-2766.
3.Gupta A, Bansal R, Gupta V. Six–month visual outcome after pars plana vitrectomy in proliferative diabetic retinopathy with or without a single preoperative injection of intravitreal bevacizumab. Int Ophthalmol. 2012;32(2):135–144.
Crossref Pubmed 4.Gupta B, Sivaprasad S, Wong. Visual and anatomical outcomes following vitrectomy for complications of diabetic retinopathy: the DRIVE UK study. Eye (Lond) R. 2012;26(4):510–516.
Crossref Pubmed 5.Kaviarasan K, Jithu M, Arif Mulla M. Low blood and vitreal BDNF, LXA4 and altered Th1/Th2 cytokine balance are potential risk factors for diabetic retinopathy. Metabolism. 2015;64(9):958-966.
Crossref Pubmed 6.Nakagawa T, Tsuchida A, Itakura Y. et al. Brain-derived neurotrophic factor regulates glucose metabolism by modulating energy balance in diabetic mice. Diabetes. 2000;49:436–444.
Crossref Pubmed 7.Ono M, Ichihara J, Nonomura T et al. Brain-derived neurotrophic factor reduces blood glucose level in obese diabetic mice but not in normal mice. Biochem Biophys Res Commun. 1997;238:633–637.
Crossref Pubmed 8.Parrilla–Reverter G, Agudo M, Sobrado-Calvo P. Effects of different neurotrophic factors on the survival of retinal gan glion cells after a complete intraorbital nerve crush injury: a quantitative in vivo study. Exp Eye Res. 2009;89:32– 41.
Crossref Pubmed 9.Ratnarajan G, Mellington F, Saldanha M. Long–term visual and retinopathy outcomes in a predominately type 2 diabetic patient population undergoing early vitrectomy and endolaser for severe vitreous haemorrhage. Eye (Lond). 2011;25(6):704–709.
Crossref Pubmed 10.Seki M, Tanaka T, Nawa H. et al. Involvement of brain–derived neurotrophic factor in early retinal neuropathy of streptozotocin–induced diabetes in rats: therapeutic potential of brain–derived neurotrophic factor for dopaminergic amacrine cells. Diabetes. 2004;53(9):2412-2419.
Crossref Pubmed 11.Tadera M, Kawamura H, Fujikawa M. et al. One year outcomes of pars plana vitrectomy in proliferative diabetic retinopathy. Nihon Ganka Gakkai Zasshi. 2014;118(6):502–507.
|