J.ophthalmol.(Ukraine).2016;1:24-26.
|
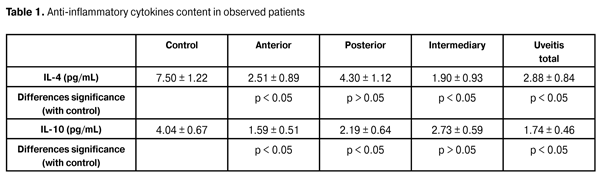
https://doi.org/10.31288/oftalmolzh201612426 Anti-inflammatory cytokines content in different clinical uveitis course complicated by the optic nerve inflammation N.V. Panchenko, Doctor of Medical Sciences M.N. Samofalova M.V. Friantseva Kharkov National Medical University Kharkov (Ukraine) E-mail: panchenko0802@gmail.com The purpose of this work was to study the content of anti-inflammatory cytokines interleukin-4 (IL-4) and interleukin-10 (IL-10) in different clinical uveitis course complicated by the optic nerve inflammation. Material and Methods. 132 patients with uveitis complicated by the optic nerve inflammation in the active stage were examined and treated. Anti-inflammatory cytokines (IL-4, IL-10) were determined in the blood serum of all the patients by immunoenzyme method. Results. It was found that the content of interleukin-4 in uveitis complicated by the inflammation of the optic nerve was 2.3 times and interleukin-10 - 2.6 times lower in comparison with control group, respectively (p <0.05). We found that the lower concentration of interleukin-10 in the blood serum correlates with the recurrent uveitis complicated by the inflammation of the optic nerve, as evidenced by the revealed strong inverse correlation (r = -0,7327; p <0,05). Conclusions. It was found, that in the active phase of uveitis complicated by the inflammation of the optic nerve, there was a significant reduction in the content of anti-inflammatory cytokines in the blood compared with the control group: interleukin-4 and interleukin-10. Lower concentration of IL-10 in the blood serum correlates with recurrent disease course. Key words: uveitis complicated by the inflammation of the optic nerve, interleukin-4, interleukin-10 Introduction Complicated uveitis forms and its outcomes remain a topical ophthalmological problem not only in Ukraine but all over the world, primarily due to reduced life quality and increased disability in patients. Being an intraocular inflammatory process, uveitis often leads to the involvement of an optic nerve, which may result in the irreversible visual impairment. In certain cases, different autoimmune diseases, infections, and adverse medications effects may cause uveitis, but in most cases, uveitis is idiopathic and its etiology remains unknown [9, 12, 13]. The social significance of uveitis consists in the fact the disease is disseminated among young and working age people. According to U. Pleyer et al., about 2.4 million people in the world suffer from uveitis [12]. According to C. Foster, the number of patients with uveitis in the United States annually increases by 280,000 people [10]. According to the literature, uveitis is the fourth most common cause of blindness in the working-age population in the developed world, although its economic and social implications are not yet fully evaluated [16]. Wherein, the blindness due to uveitis in both eyes reaches 10% [9], and vision disability is about 30% [2]. An important role in the pathogenesis of uveitis is of cytokines [4, 5, 6, 8, 11]. Although, in the available literature we have not found any works on the study of cytokine status characteristics in uveitis, complicated by the optic nerve inflammation. Objective of this work was to study the content of anti-inflammatory cytokines interleukin-4 (IL-4) and interleukin-10 (IL-10) in different clinical uveitis course complicated by the optic nerve inflammation. Material and methods 132 patients with uveitis complicated by the optic nerve inflammation in the active stage were examined and treated. The group of study consisted of 79 women and 53 men. The age of the surveyed persons ranged from 18 to 74 years. Duration of the disease ranged from one month to 14 years. Anterior uveitis was diagnosed in 45 individuals, posterior – 43, intermediate uveitis – 29, general – 15 patients. The nature of the disease course (without specific anti-treatment) within the periods of observation for at least two years and uveitis relapses complicated by the inflammation of the optic nerve presence was studied in 82 people. Among them, relapses occurred in 32 patients (39%) within the specified period. All patients were examined by conventional methods of ophthalmological survey, including ultrasound biomicroscopy (sensor with frequency 50 MHz) and optical coherence tomography. Anti-inflammatory cytokines (IL-4, IL-10) were determined in the blood serum of all the patients by immunoenzyme method with a standard set of reagents [1]. Control blood serum was taken of 30 healthy donors. Statistical data processing was performed using Statistica Ver. 6.1 software, with the calculation of Student coefficient and nonparametric Spearman rank correlation coefficient. Results and Discussion After the researches, it was found that patients with the active stage of uveitis complicated by the inflammation of the optic nerve had significantly reduced anti-inflammatory cytokines content in the blood in comparison with healthy donors (p <0.05). In this, the content of interleukin-4 in uveitis complicated by the inflammation of the optic nerve was 2.3 times lower than in control group (2.88 ± 0.84) pg/ml and (1.22 ± 7,50) pg/ml, respectively (p <0.05), and interleukin-10 - 2.6 times lower in comparison with control group (1.74 ± 0.46) pg/ml and (4.04 ± 0.67) pg/ml, respectively (p <0.05). The data obtained is consistent with the results of Takase H. et al. researches [8] on low (or lower than detection level) content of interleukin-4 and interleukin-10 in the blood serum in infectious and non-infectious uveitis and Drozdova EA. et. al. data [1] on lowering the content of interleukin-4 in the blood serum of patients with uveitis on the background of ankylosing spondylitis. Upon that, our results differ from those reported by other authors, according to which the content of interleukin-4 [3, 6, 14, 15] and interleukin-10 [6] in the blood serum is not reliably differing from the control group. The divergence of our findings with M. Cordero-Coma et al. data on the increase of IL-10 [5] in the blood serum of patients with chronic refractory uveitis, in our opinion, may be due to the fact that the cytokine profile was studied by these authors after conducting a systemic therapy, which was used in refractory uveitis and usually included steroids and/or cytostatics. Anti-inflammatory cytokines content, depending on uveitis localization complicated by the inflammation of the optic nerve, according to our data, is shown in Table 1.
It was found that the most pronounced decrease of interleukin-4 is observed in intermediary uveitis (almost 4 times compared to control group) and the least pronounced in posterior uveitis (1.7 times compared with the control group). Interleukin-10 content was reduced to a greater extent in anterior uveitis (2.5 times in comparison with the control group) and to a lesser extent in intermediary uveitis (1.5 times compared to the control group). We also studied the concentration of pro-inflammatory cytokines in the blood serum of the observed patients, depending on the presence or absence of the relapses of uveitis complicated by the inflammation of the optic nerve. After the researches, it was found that in the acute stage of the disease among the observed patients within two years there occurred uveitis relapses complicated by the inflammation of the optic nerve. Lower content of interleukin-4 was found in the blood serum (3.11 ± 0.91) pg/ml than in patients with a relapse-free course of uveitis (3.96 ± 1.05 pg/ml), although the differences were basically the trend (p> 0.05). The content of interleukin-10 in the blood of patients, who had during the observation period (up to two years) uveitis relapses with the inflammation of the optic nerve aggravation, was significantly lower (0.96 ± 0.53 pg/ml; p <0.05), in comparison with patients without relapses of inflammation in the uveal tract and the optic nerve (3.31 ± 0.61 pg/ml). Upon that, the confidence interval (with a probability of p <0.05) of the concentration of interleukin-10 in the blood serum in patients with recurrent disease course was within the interval of 0 pg/ml –2.02 pg/ml. In terms of the discussion of the results obtained, it should be noted that during the experimental autoimmune uveitis development, IL-10 is determined only in the end of the disease [7] and, according to L. Tian et al. data, combined virus-2 adenoassociated subretinal delivery of IL-4 helps to suppress experimental uveoretinitis [4]. Wherein the production of IL-4 and IL-10 correlates with the "remission" of experimental autoimmune uveitis, which may indicate their role in "spontaneous" termination of the inflammatory process in the vascular tract in the experiment [17], which indirectly is consistent with our results. We found that the lower concentration of interleukin-10 in the blood serum correlates with the recurrent uveitis complicated by the inflammation of the optic nerve, as evidenced by the revealed strong inverse correlation (r = -0.7327; p <0.05) between the concentrations of interleukin-10 in the blood serum and the relapse occurrence and the onset uveitis with an aggravation of inflammation of the optic nerve. This conclusion is indirectly confirmed by the results of U. Kaufmann et al. that had established the increase of the number of intraocular t-lymphocytes, expressing interleukin-10 under single phase experimental autoimmune uveitis in rats compared with recurrent experimental autoimmune uveitis [11]. On the ground of our findings the method is offered to predict the course of uveitis complicated by the inflammation of the optic nerve (Patent of Ukraine UА 84280 U) by determining the concentration of interleukin-10 in the blood serum in acute period of the disease, at which 2.02 pg/mL and below values forecast the relapsing disease course. The researches conducted make it possible not only to predict the course of uveitis complicated by the inflammation of the optic nerve but also to become a basis for the development of new methods to prevent the inflammatory process recurrence in the uveal tract and optic nerve. Conclusions 1. It was found, that in the active phase of uveitis complicated by the inflammation of the optic nerve, there was a significant reduction in the content of anti-inflammatory cytokines in the blood compared with the control group: interleukin-4 and interleukin-10. 2. There was developed a method of predicting the recurrent course of uveitis complicated by the inflammation of the optic nerve, based on determining the concentration of interleukin-10 in the blood serum of these patients. Low concentration of interleukin-10 (<2.02 pg/ml) in the blood of patients with uveitis indicates its relapsing course (Patent of Ukraine UA 84280 U). References 1. Drozdova EA, Tarasova LN, Teplova SN, Alekhina TV. [Immunological characteristics of uveitis in case of systemic diseases]. Vestnik oftalmologii. 2004;120(4):24-26. Russian. 2. Katargina LA, Khvatova AV. [Endogenous uveitis in children and adolescents]. Meditsina. 2000:320. Russian. 3. Lacomba MC, Martin CM, Chamond RR et al. Aqueous and serum interferon gamma, interleukin (IL) 2, IL-4, and IL-10 in patients with uveitis. Arch. Ophthalmol. 2000;118:768-772. 4. Tian L, Lei B, Shao J. et al. AAV2-mediated combined subretinal delivery of IFN-?and IL-4 reduces the severity of experimental autoimmune uveoretinitis. PLoS. One. 2012;7(6):e37995.doi:10.1371/journal.pone.0037995. 5. Cordero-Coma M, Calleja S. Serum cytokine profile in adalimumab-treated refractory uveitis patients: decreased IL-22 correlates with clinical responses. Ocul. Immunol. Inflamm. 2013;21,(3):212-219. 6. Chen W., Zhao B., Jiang R et al. Cytokine expression profile in aqueous humor and sera of patients with acute anterior uveitis. Curr. Mol. Med. 2015;15:511-518. 7. Li Q., Sun B., Matteson DM et al. Cytokines and apoptotic molecules in experimental melanin-protein induced uveitis (EMIU) and experimental autoimmune uveoretinitis (EAU). Autoimmunity. 1999;30:171-182. 8. Takase H., Futagami Y., Yoshida T. et al. Cytokine Profile in Aqueous Humor and Sera of Patients with Infectious or Noninfectious Uveitis. Invest. Ophthalmol. Vis. Sci. 2006:47(4):1557-1561. 9. Rupesh V., Somasheila M., Virender I. Current approach in diagnosis and management of anterior uveitis. Indian. J. Ophthalmol. 2010;58(1):11-19. 10. Foster C. Uveitis: A Guide for Teachers and Parents. The Ocular Immunology and Uveitis Foundation. Cambridge, USA. 2004:5-89. 11. Kaufmann U., Diedrichs-M?hring M., Wildner G. Dynamics of intraocular IFN-?, IL-17 and IL-10-producing cell populations during relapsing and monophasic rat experimental autoimmune uveitis. PLoS. One. 2012;7(11):e49008. doi: 10.1371/journal.pone.0049008. 12. Pleyer U, Mondino B. Uveitis and immunological disorders (Essentials in Ophthalmology). Pleyer U.New York. 2005:126-127. 13. De Groot-Mijnes J., Rothova A., Van Loon A. et al. Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am. J. Ophthalmol. 2006;141:313-318. 14. Gratacos J, Collado A., Filella X. et al. Serum cytokines (IL-6, TNF-alpha, IL-1 beta and IFN-gamma) in ankylosing spondylitis: a close correlation between serum IL-6 and disease activity and severity. Rheumatol BrJ. 1994;33:927-931. 15. Damico FM, Cunha-Neto E, Goldberg AC. et al. T-cell recognition and cytokine profile induced by melanocyte epitopes in patients with HLA-DRB1*0405-positive and -negative Vogt-Koyanagi-Harada uveitis. Invest. Ophthalmol. Vis. Sci. 2005;46:2465-2471. 16. Smet M., Taylor S, Bodaghi B. et al. Understanding uveitis: The impact of research on visual outcomes. Prog. Retin. Eye. Res. 2011;30:452-470. 17. Xu H, Rizzo LV, Silver PB, Caspi RR. Uveitogenicity is associated with a Th1-like lymphokine profile: cytokine-dependent modulation of early and committed effector T cells in experimental autoimmune uveitis. Cell. Immunol. 1997;178:69-78.
|