J.ophthalmol.(Ukraine).2016;1:65-68.
|
https://doi.org/10.31288/oftalmolzh201616568 A case of combination of Eales disease and Arnold Chiari syndrome V.S. Ponomarchuk, Doctor of Sc. (Med) N.I. Naritsyna, Candidate of Sc. (Med) N.V. Konovalova, Doctor of Sc. (Med) T.M. Serebrina, Candidate of Sc. (Med) V.B. Reshetniak Filatov Institute of Eye Diseases and Tissue Therapy Odessa, Ukraine E-mail: phosphere@te.net.ua Purpose. A description of a rare combination of Arnold — Kiari syndrome and Eales Disease is given. Material and Methods. We followed up a 24 y.o. patient with Eales Disease combined with Arnold — Kiari syndrome. Results. According to clinical and functional examination data, a patient was diagnosed Ealse disease. Taking into account changes in the optic disc which are not typical for that disease, a patient was performed MRT of the head which revealed the presence of Arnold — Kiari syndrome. Conclusion. The present clinical case is evidence of combination of Arnold — Kiari syndrome and Eales Disease, thus, practical ophthalmologist should have that in mind and examine patients carefully. Key words: Eales Disease, Arnold — Kiari syndrome, diagnostics A technology level of modern medicine allows us to diagnose diseases which were not possible to diagnose during the lifetime of a patient. One of such diseases is Arnold Chiari syndrome which is developed prenatally within 2-8 weeks of pregnancy when vital organs are being formed. Incidence of Arnold Chiari syndrome development is 1-4 cases per 1 000 newborns, though these data will be revised due to the widespread use of magnetic resonance tomography (MRT) [1, 2, 3]. Risk factors for this congenital pathology are such unfavorable factors as drug-induced intoxication, diabetes mellitus, iodine deficiency, fasting, ecological disturbances, maternal infection (syphilis, Torch-infections and others) [ 4, 5, 6], which disturb the formation of foramen magnum by increasing its size. Normal longitudinal size (occipitofrontal) is 50-60 mm and lateral size (parietal) is 25-40 mm. This defect in skull development is a risk factor for central nerve system element dislocation. Inferior part of cerebellum can fall out or wedge in an increased opening that leads to development of intracranial hypertension inducing papilledema formation [7]. Previously, we have reported on a clinical case of Arnold Chiari syndrome [8], thereafter we have observed some more patients with this pathology. However, a combined case of Arnold Chiari syndrome and Eales disease is of a special interest since the latter refers to connective tissue system diseases or collagenoses and can be interesting in the context of clinical interpretation. The purpose of the present paper is to describe the clinical case of Arnold Chiari syndrome manifested in the optic nerve affection in combination with Eales disease. Materials and Methods We followed up a patient S., 24 y.o., a case-record № 589550. Admission complaints were periodical visual blurring in both eyes first noticed in summer 2014. Community based examinations including optical coherence tomography (OCT) and fluorescein angiography of the retina showed changes which were specific for Eales disease: new blood vessels and hemorrhages with vitreoretinal proliferations were observed in the retina periphery. The patient does not connect the disease to anything; hereditary background isn’t burdened. During the initial examination, floating and fixed blurrings in the vitreous were detected in both eyes of the patient, the optic disc on the eye fundus was solid pale-pink, borders were clear cut due to the proliferative changes in parapapillary area, retinal vessels were curly and had uneven caliber, reflexes in the macular were not clear, and there were multiform preretinal and retinal hemorrhages and neovascularization in the periphery in the outer quadrants against the backgrounds of vitreoretinal proliferations. The patient underwent a complex clinical functional examination of the visual analyzer. Results and Discussion According to OCT data there were a limited number of floaters in the vitreous of both eyes; detachment of posterior hyaloid membrane of the vitreous was noted in the left eye; retinal thickness was within normal range with no pathological focal changes; neuroepithelium was unevenly indurated; retinal pigment epithelium (RPE) had no distinctions. According to ultrasound scanning, moderate destruction of the vitreous was noted in the vitreal space of both eyes, the optic disc protruded into the vitreous by 0.58 high in the right eye and 0.85 mm high in the left eye; chorioretinal layer around the optic disc, especially in macula, was heterogeneous without protrusion in the vitreous. Distance visual acuity was 1.0 in both eyes; near visual acuity equaled reading font 8; visual field respond to a white object was within the normal range, whilst that to red and green colors was narrowed to 5-7°, blind spot size was increased by 2-3 cm. Phosphene threshold was 70 and 38 µA in the right and left eye, respectively, that can be recognized as asymmetry of reflection of initial depression (dystrophy) of the optic nerve of the right eye. Analysis of Retiscan complex electrophysiological study allowed to determine the character of bioelectrical activity of peripheral and central parts of visual analyzer. Bioelectrical activity response of visual cortex to F-VEP flash was normal. Bioelectrical activity response of visual cortex to 1°and 0°15' patterns by wave amplitude of P100 improved after treatment from 6.9 to 8.8 µV to 1°, while that to 0°15' remained normal; bioelectrical activity response of visual cortex in the left eye after treatment improved from 5.3 to 7.7 µV and from 4.7 to 6.1 µV to 1° and 0°15' patterns, respectively. Herewith, latency remained normal (Fig. 1A and 1B).
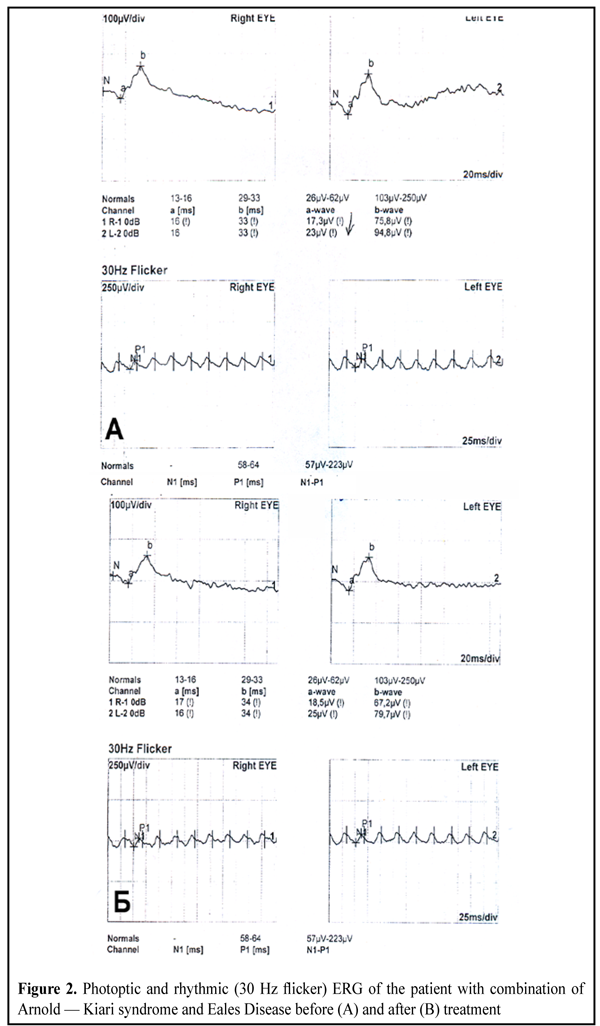
Bioelectrical activity of photoreceptor layer (cones and rods) and medium retinal layers (bipolar and Muller cells) by the periphery of the retina was normal both before and after treatment, keeping the value according to the standard electroretinogram (ERG) for wave amplitudes 154-167 µV (“a”) and 229-347 µV (“b”). Different bioelectrical activity was noted in the macular area. At wave amplitude “a” cone bioelectrical activity response before the treatment equaled 17.3 µV and 23 µV (norm is 26 µV) in the right and left eye, respectively, and after the treatment it was equal to 15.5 µV and 25 µV, respectively, whilst wave amplitude “b” or activity of medium layers of the retina remained moderate decreased (Fig. 2A and 2B).
The feature of visual analyzer bioelectrical activity response was its decrease to 1°and 0°15' patterns and depression of outer and medium retinal layers in both eyes. Taking into account atypical for Eales disease ophthlmoscopic and functional indices of the optic disc, the patient was taken to MRT of the head which revealed Arnold Chiari syndrome: MR-signs of Arnold Chiari malformation type 1 (tonsils of cerebellum are lower than the foramen magnum by 5 mm), syringomyelic cyst is at the level of cervical and thoracic part of spinal cord (С3-Th2). Brain volume changes were not detected. Visual organ had no changes: eyeballs were symmetric, optic nerves were neither thickened nor misshapen and with clear boundaries; optic chiasm was not misshapen and there were no additional masses in the retrobulbar tissue. Patient immune state study revealed lymphopenia (lymphocyte level was 1.36 х 106 l whilst the norm is 1.5-3 х 106 l), decreased level of T-suppressors (natural killers), increased level of IgA and decreased level of IgM; sensibilization to eye tissue was noted. The patient underwent the course of vasoactive, resolving, hyposensitizative and immunocorrecting therapy. On completing the treatment course the ophthamoscopy study revealed a decrease of floaters in the vitreous and improvement of retinal vessel state. Uncorrected visual acuity was 1.2 in both eyes. The rest of clinical and functional indices were not changed. 3 months later, a control examination was performed; the patient had normal visual acuity and visual field kept; according to ophthalmoscopy data, optic discs remained solid pale-pink, however, their borders became clearer cut, vessel caliber was even, there were no new changes in the retinal periphery. According to the data of the repeated electrophysiological examination, there was depression of the macular area and cortex activity decrease to the left, the rest disturbed indices were normalized. Analyzing the clinical and functional examination data raises a question whether a combination of Eales disease and Arnold Chiari syndrome is occasional or these are the links of one pathogenic chain. It is hard to say definitely. Eales disease (vasculitis, periphlebitis retinae, angiopathia retinae juvenilis) is a selective retinal vasculopathy in a form of retinal vasculitis, mainly phlebitis, characterized by recurrent retinal and vitreal hemorrhages in both eyes. The process has an autoimmune character and male predominance with age of 20-40 years old. It should be noted that the changes in the optic disc in this case were atypical for Arnold Chiari syndrome, in which, as a rule, papilledema is formed. In the patient we observed optic disc blanching and unclear boundaries due to proliferation in parapapillar area, and proliferations are one of the main signs for Eales disease. These changes are of chronic character; their formation takes certain time under the influence of long-lasting moderate expressed intracraneal hypertension. At the same time it should be noted that the optic disc remains, as a rule, intact in Eales disease. Eales disease is related to a systemic disease of connective tissue, vasculitis, which is combined with neuroophthalmological pathology. Thus, the patient may have congenital defects both facilitating anatomic disorders in CNS and spinal cord and predisposing the development of systemic diseases, in particular, vasculitis. A detection of correlation between different, at the first sight, pathologies, will allow to give a patient correct recommendations for the following observation by neuroophthalmologists as well as to develop an adequate tactic for treatment. Conclusion
Practical ophthalmologists should pay attention to the symptoms of concomitant diseases and atypical symptoms of main condition and enlarge the diagnostics not only of eye disease but general pathology that will enable to diagnose other serious pathological processes in the organism. The early diagnostics of concomitant diseases will prevent their progressing and complicating by cooperating with other specialists. Reference 1. Biran VP. [Rare syndroms and symptoms in ophthalmology]. Moscow: Meditsina; 9.87. In Russian. 2. Khoppe V. [Ophthalmology]. Moscow;2005. 309 p. In Russian. 3. Miller N., Newman N. Walsh and Hoyt’s Clinical Neuro-Ophthalmology. Baltimore, 1998. 4. Morozov, V. I., Yakovlev, A. A. (2010). [Diseases of the visual pathway]. Moscow: Meditsyna, 2010. 620 p. 5. Nikiforova A.N. et al. [Neuroophthalmology]. GEOTAR-Media; 2008. 624 p. In Russian. 6. Shpak T.N. [Clinical manifestations of the syndrome of Arnold — Kiari]. Med. Vestn.Ukrainy. 2000;39-40:5. In Russian. 7. Zhaboiedov GD. [Optic nerve diseases]. Kiev: Zdorovye;1992. 215 p. In Russian. 8. Naritsyna N. I., Konovalova N. V., Serebrina T. M., Novik A. Ya., Mikhailichenko L. A., Rybalko A. V. [Ocular manifestations of the syndrome of Arnold — Kiari]. Oftalmol Zh.2012;1:42-43. In Russian.
|