J.ophthalmol.(Ukraine).2015;6:13-16.
|
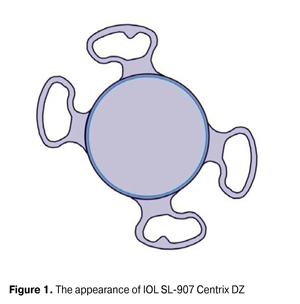
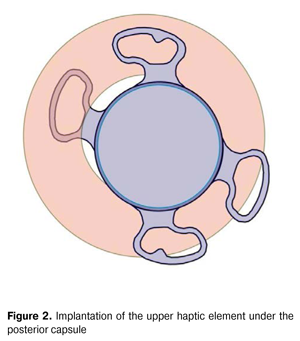
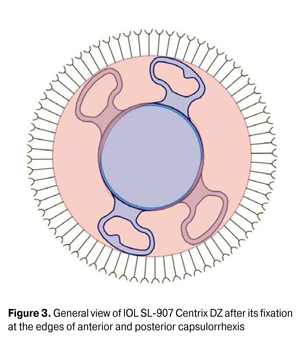
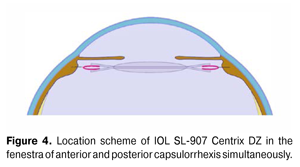
https://doi.org/10.31288/oftalmolzh201561316 Fixation of the intraocular lens SL-907 CENTRIX DZ in the lenticular sac fenestra as a result of anterior and posterior capsulorrhexis D.G. Zhaboiedov, Doctor of Medical Sciences Bogomolets National Medical University Kyiv (Ukraine) Е-mail: zhaboedov@ukr.net Key words: phacoemulsification, secondary cataract, IOL implantation, anterior and posterior capsulorrhexis, lenticular sac fenestra, IOL fixation. Introduction. Despite the considerable improvement and general practical application of high-tech techniques in cataract surgery, in the late postoperative period 4.5-20% of cases are complicated by the secondary cataract that motivates to a further search of new and more effective methods of its development preventing. Objective is to study the effectiveness of the method of IOL SL-907 Centrix DZ fixation at capsulorrhexis edges for preventing the secondary cataract development. Materials and methods. 35 patients were examined during the study. They were implanted IOL SL-907 Centrix DZ after senile cataract phacoemulsification. It was fixed at the edges of anterior and posterior capsulorrhexis so that 2 haptic elements were located at the posterior capsule edge and the other two at the anterior capsule edge. In this case, capsulorrhexis edges were located between haptic elements and the optical part was located directly above the hyaloids membrane. Results and discussion. All the patients had no complications during the postoperative period. The control examination in 6 months after the implantation showed a revealed stability of the implanted IOL in all cases. Three years after the surgery, the routine examinations showed no IOL dislocation and decentration, as well as the signs of the opacity; the vision of the patients remained stable. Visual acuity averaged 0.7±0.2. IOP indicators were within the normal range (13-17 mm Hg). Conclusions. Thus, the developed IOL SL-907 Centrix DZ fixation method at the fenestra of anterior and posterior capsulorrhexis has proved to be effective as in terms of fixation reliability, as in terms of prevention of secondary cataract development. Introduction Modern micro-invasive and high-tech methods of cataract phacoemulsification (CPE) with the implantation of the latest models of intraocular lenses (IOL) in the vast majority of cases provide a restoration of the vision lost due to the cataract almost immediately after the surgery. However, despite the significant improvement and widespread introduction of the latest technologies into the cataract surgery clinical practice, the formation of secondary cataract (SC) still remains a specific complication of its distant postoperative period. Posterior capsular opacification of the crystalline lens (PCOCL) is diagnosed in 4,5-20% of cases and tends to increase with the passage of time after the surgery, and almost every fourth and fifth patient requires further laser discission to restore the visual functions [3, 6]. Secondary cataract progressing is caused by the inevitable post-operative proliferation and migration of the epithelial cells from the equatorial to the central optical zone, as well as the regular fibrous metaplasia of the posterior capsule. However, these cells (socalled Adamenko Elschnig cell-balls) are defective functionally and structurally, shaped irregularly, nontransparent, therefore, at the moment of their migration o the central optical zone the membrane opacification is formed, which reduces the visual acuity (sometimes very significantly). The terms of formation of secondary cataract express manifestation vary from a few months to several years [1, 5]. Until the present time, the preferred method of choice of the secondary cataract treatment remains YAG laser capsulotomy. According to the literature, the frequency of PCOCL, requiring YAG laser discission in the first two years after the surgery, is between 10 and 50%. However, even the performance of strictly power dosed laser discission is associated with the risk of development of such complications as: reactive intraocular pressure increase - according to a number of authors may reach 20 - 43% of cases; intraocular lens (IOL) damage - an average of 20 %; epithelial-endothelial dystrophy -between 2.1 and 7.3%; retina ruptures and detachment - between 0.08 and 2.0 % of cases; macular edema on average develops in 0.9% of patients [1,3]. Currently, the intensive search for new possibilities of solving the secondary cataract problem is performed. The questions about their efficiency and expediency continue to be discussed that confirms the relevance of PCOCL development prevention. Secondary cataract prevention methods include such distinguished surgical techniques, as mechanical and vacuum posterior capsule hydro-treating, cortical separating hydrodissection, special intracapsular ring administration into the lenticular sac, primary posterior continuouscapsulorrhexis performance, as well as creation of special design IOL features, including the search of thematerial it is made of, and specific lens design selection and creation. From the point of view of the most of researchers, a significant role in the development of the secondary cataracts is played by the tightness of back IOL surface and the crystalline lens capsule abutment, as well as a special protective axial edge availability over the entire circumference of its optical part [4, 7, 8]. In addition, numerous researches have been conducted over the past years to prevent SC development and capsular sac cells regeneration reduction by blocking the growth of the equatorial zone cells, posterior capsulorrhexis performance and new IOL models and their fixation methods development. One of the ways of solving this problem is an innovative method of IOL implantation with its fixation by the anterior and posterior capsulorrhexis, as evidenced by successful results of many years of research by Professor Marie- Jose Tassignon [2, 9, 10]. However, Tassignon lens was primarily developed for its use in the pediatrics practice, and in addition its provision on the Ukrainian market is limited. Such a fact has prompted us to start searching for the domestic IOL model, suitable to be fixed at the capsulorrhexis edges. Such lens proved to be our IOL SL-907 Centrix DZ lens, developed by us earlier. It can be fixed both traditionally in the capsule sac, and in case of its defectiveness, can be fixed suturally to the iris and the sclera of the eyeball. In addition, IOL SL- 907 Centrix DZ has the design features that prevent proliferation of the epithelium of the posterior capsule, providing an insurmountable barrier to the migration cells into the optical center, namely, a special uniform rim on the posterior surface of the IOL, optic and the haptic parts have a rectangular strengthened edge. Its haptic elements are located at an angle of 5° to the optical part of IOL that makes an impasse for epithelial cells migration. The objective is to examine the effectiveness of IOL SL-907 Centrix DZ fixation method at the capsulorrhexis edges in order to prevent the secondary cataract development. Material and methods The work was performed on the bases of Bogomolets NMU department of ophthalmology in the period from 2011 to 2013. 35 patients were examined during the study. All the patients were implanted IOL SL-907 Centrix DZ (Fig.1) by a surgeon using the same procedure. Cataract phacoemulsification was performed following the conventional method. After that, IOL was administered into the anterior chamber and under the protection of viscoelastic the posterior capsulorrhexis was performed. Then the upper IOL haptic element was implanted under the posterior capsule (Fig. 2) and furthers the lower one, disposed diagonally, was implanted too, whereby both of the haptic elements were under the edge of the posterior capsule and the remaining two were over the anterior capsule (Fig. 3). In this case, the anterior and posterior edges of capsulorrhexis were placed between the haptic elements and the optical part of the lens was directly above the hyaloid membrane of the vitreous body (Fig. 4).Results and discussion.
The postoperative period of all the patients proceeded without complications. At the second day after the surgery the eyes were calm. Under the biomicroscopy the optical media of the eyes remained transparent, resulting in clear fundus details visibility. There were no pathological changes found. The control examination in 6 months after the implantation showed a revealed stability of the implantedIOL in all cases. Visual acuity averaged 0.7±0.2. There were no complaints of the patients on the visual discomfort, no signs of turbidity, no illuminated optical phenomena such as strobing, glares of the pupil and halo. Refraction of the operated eyes, as well as the indicators of the visual acuity during the entire observation period remained fairly stable. Such regularity has revealed to be characteristic for the spherical component, but more variable for toric component (cylindrical), although the limits of the indicators werechanging in the range of ±0.5 diopters in the vertical meridian predominantly. We explain this fact with the influence of the emerging corneal scars on the refraction at the location of the portal incisions through which the clouded lens has been removed and the implantation of IOL was made. Such an opinion is confirmed by the refraction dynamics, which was stabilized already in the first period of the remote observation (6 months), as well as the degree of astigmatism within ± 0.5 diopters, making it possible to maintain a high eye visual acuity, but did not alter the refraction spherical component, which, as is known, depends largely on the anterior-posterior IOL displacement in the eye. IOL SL-907 Centrix DZ implantation into the capsulorrhexis fenestra retains all the advantages of IOL administration into the cavity of the crystalline lens sac. Three years after the surgery, the routine examinations showed no IOL dislocation and decentration, as well as the signs of the opacity, the vision of the patients remained stable. Visual acuity averaged 0.7±0.2. IOP was within the normal range (13 – 17 mm hg). It convinced us in the feasibility and clinical use safety of the developed IOL SL-907 Centrix DZ fixation method at the fenestra of anterior and posterior capsulorrhexis. Thus, the developed IOL SL-907 Centrix DZ fixation method at the fenestra of anterior and posterior capsulorrhexis has proved to be effective both in fixation reliability, and in prevention of secondary cataract development. The lens is convenient on the design features and can be an affordable alternative when selecting intraocular lens in order to ensure the patients with highly technological method of rehabilitation in cataract extraction. The implantation method is simple and does not require additional special devices for its implementation, and is a reliable reserve in cases of nonstandard situations occurrence during the performance of routine phacoemulsification with IOL implantation due to the fact that the surgeon has the possibility to use the remained fenestra after the extraction of the clouded crystalline lens of the anterior and posterior capsulorrhexis. Conclusions Thus, the developed method of IOL SL-907 Centrix DZ fixation at the lenticular sac fenestra at the anterior and posterior capsulorrhexis has proved to be effective both in fixation reliability, and in prevention of secondary cataract development. The implementation of this method is simple and requires no additional devices, which ensures the availability of highly technological vision rehabilitation for our patients, since the effect of IOL fixation is safe and reliable. References 1. Belyy Yu.A., Tereshchenko A.V., Fedotova M.V. The prevention of posterior capsule opacification after cataract surgery. Review. Refraktsionnaia khirurgiia i oftalmologiia. 2009;3:4-9. In Russian. 2. Bobrova N.F., Tassignon M.J., Lorenz B., Dembovetskaya A.N. et al. Implantation of IOL with new type of fixing “bagin-the-lens” at phacoaspiration of congenital cataracts in children. Oftalmol Zh. 2009;6:9-16. In Russian. 3. Malyugin B.E. Cataract surgery and intraocular correction: results and prospects. IX Congress of Ophthalmologists of Russia; 16-18 June; Moscow; 2010. P. 192-195. In Russian. 4. Minakova S.E., Dmitriev S.K. Improved method of primary posterior continuous capsulorrhexis. Oftalmol Zh. 2009;5:87-88. In Russian. 5. Pozniak S.P., Marchenko L.N., Pozniak N.I. et al. Reasons of lens posterior capsule opacification after phacoemulsification. Fedorovskie Readings – 2007, Jubilee Scientific Conference, dedicated to 80 ann. Of S. Fedorov; 14-15 June; Moscow; 2007. P.72. In Russian. 6. Sorokoletov G.V., Zuyev V.K., Tumanyan E.R., Bessarabov A.N., Vescikova V.N. Frequency of secondary cataract development in pseudophakic eyes with posterior chamber IOL of current designs in case of axial myopia. 7. Oftalmokhirurgiia. 2013;3:28-32. In Russian. 7. Cheng J.W., Wey R.L., Cai J.P. et al. Efficacy of different intraocular lens materials and optic lens designs in preventing posterior capsular opacification: a metaanalysis. Am. J. Ophthalmol. 2007;143(3):428-436. 8. Peng Q., Visessook N., Apple D. Et al. Surgical prevention of posterior capsule opacification. Part 3: intraocular burrier lens effect as a second line of defense. J. Cataract. Refract. Surg. 2000;26:198-213. 9. Tassignon M.J., Groot V. De, Vrensen G.F. Bag-inthe-lens implantation of intraocular lenses. J. Cataract. Refract. Surg. 2002;28:1182-1188. 10. Tassignon M.J., Dhubhghaill S.N. Bean-shaped ring segments for capsule stretching and centration of bagin- the-lens cataract surgery. J. Cataract. Refract. Surg. 2014;40:8-12.
|