J.ophthalmol.(Ukraine).2015;6:6-12.
|
https://doi.org/10.31288/oftalmolzh20156612 Clinical efficacy of pterygium surgery technique involving use of high frequency welding of biological tissues for fixing free limbal conjunctival autograft V.Ia. Usov, Dr. Sc. (Med) E.V. Maltsev, Dr. Sc. (Med), Prof. N.I. Krytsun, Postgraduate Student Filatov Eye Disease and Tissue Therapy Institute, the NAMS of Ukraine Odessa (Ukraine) E-mail: Natalya1979@ukr.net Background: It is important to reduce the rate of early complications following pterygium surgery. Purpose: To determine whether the use of high-frequency welding of biological tissues (HFWBS) for fixing a free limbal conjunctival autograft (LCAG) improves the efficacy of surgical treatment of pterygium. Material and Methods: We retrospectively analyzed data from 73 patients (73 eyes) who underwent free LCAG surgery for different stages of pterygium. Patients were divided into the HFWBS group (34 patients; 34 eyes) and the control group (39 patients; 39 eyes). The former underwent pterygium surgery involving the use of HFWBS for fixing a free LCAG with upgraded EK-300M1 apparatus and special bipolar forceps, and the latter underwent free LCAG with sutures following pterygium excision. Efficacy was assessed in terms of clinical signs (corneal reepithelialization rate, inflammatory response intensity, corneal syndrome intensity, and corneal transparency at the site of excised pterygium) postoperatively. Results: At day 5, (a) complete corneal re-epithelialization was significantly more often found in the HFWBS group (30/34 eyes; 88.2%) than in controls (20/39 eyes; 51.3%) (?2 = 13.7; р = 0.00021), (b) patients of the former group had neither the highest nor a high score of local inflammatory vascular response, whereas 3/39 (7.6%) patients of the latter group had the highest score of local inflammatory vascular response (?2 = 237; р = 0.00003), and (c) signs of corneal syndrome were found in 1/34 eyes (2.9%) of the HFWBS group vs 39/39 eyes (100%) of controls; i.e., corneal syndrome was observed 97.1% less often in the HFWBS group than in controls. At observation time points less than 3 months, restoration of corneal transparency was observed in 33/34 eyes (97.1%) of the HFWBS group vs 12/39 eyes (30.8%) of controls (р = 0.0001). Conclusion: First, in LCAG, the use of HFWBS significantly improves the efficacy of surgical treatment of pterygium. At day 3, complete corneal re-epithelialization was significantly more often found in the HFWBS group than in controls (73.5% vs 15.4%; difference, 58.1%). At day 5, this difference remained statistically significant and was 36.9%. Second, at all observation time points, low vascular response scores were found statistically significantly more often in the HFWBS group than in the controls (Pu < 0.015). Third, LCAG with HFWBS was found advantageous over LCAG with sutures in terms of corneal syndrome, since, at day 5, practically all eyes (33/34 eyes; 97.1%) of the HFWBS group were quiet, whereas all eyes (39/39 eyes; 100%) of the controls were mildly irritated (?2 = 69.1; р = 0.00001). Finally, at month 3, restoration of corneal transparency was observed in the HFWBS group 66.3% more often than in controls (?2 = 33.8; р = 0.00001), thus supporting the advantage of HFWBS in pterygium treatment with LCAG. Key words: pterygium, sutures, electric welding, autograft
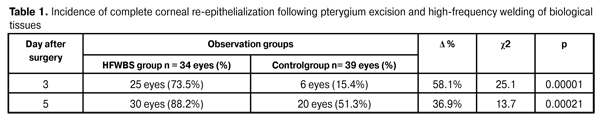
Introduction Management of pterygium has tended to be based on its surgical excision [1-6], with recurrence rates of at least 40-70% [5, 6]. Foreign comparative studies of different current methods of surgical excision of pterygium have been reported not only to demonstrate that these methods do not prevent the recurrence but also to specify the approximate time of re-development of pterygium [7]. High recurrence rates make the development of new and improvement of existing surgical procedures for pterygium treatment a high priority [8]. Currently, the most common type of fixation of LBAG is fibrin glue fixation followed by sutured fixation [9]. Another tissue joining technique is high-frequency welding of biological tissues (HFWBS) which is used in general surgery with the aid of commercial high-frequency current generator EK-300M1 and commercial surgical instruments [10]. Previously, special bipolar forceps developed by us in collaboration with the Paton Electric Welding Institute of the NationalAcademy of Science of Ukraine were successfully tested with upgraded EK-300M1 apparatus for joining the edges of a surgical conjunctival wound [10, 11]. The purpose of the study was to determine whether the use of high-frequency welding of biological tissues for fixing a free limbal conjunctival autograft (LCAG) improves the efficacy of surgical treatment of pterygium. Materials and Methods We retrospectively analyzed data from 73 patients (73 eyes) who underwent surgery for pterygium of stages 2 to 4 by the Dudinov and Tsepeniuk classification [12]. These were in-patients of Ophthalmology Department of Ivano- Frankivs’k Regional Clinical Hospital and out-patients of Ivano-Frankivs’k Regional Consulting Polyclinic (which is the clinical training center at the Ivano-Frankivs’k National Medical University) and the Filatov Institute, Corneal Department, treated during 2010-2014 [13]. Patients were divided into the HFWBS group (Group 1; 34 patients; 23 men and 11 women; mean age: 56.4 years; 34 eyes) and the control group (Group 2; 39 patients; 17 men and 22 women; mean age: 58.3 years; 39 eyes). Patients of Group1 underwent pterygium surgery with the technique proposed by us (Declarative Patient of Ukraine No. MPK А61F 9/007 12.01.2015), and those of Group 2 underwent LCAG with sutures following pterygium excision. In the HFWBS group, stage 2 pterygium was the most common (18 eyes; 52.9%), followed by stage 3 pterygium (14 eyes; 41.2%) and stage 4 pterygium (2 eyes; 5.9%). In the controls, stage 2 pterygium was the most common (20 eyes; 51.3%), followed by stage 3 pterygium (16 eyes; 41%) and stage 4 pterygium (3 eyes; 7.7%). The groups were not statistically significantly different in sex and age from each other. Additionally, they were not statistically significantly different in the pterygium stage (?2 = 0.1; р = 0.95). Each patient underwent a standard ophthalmic examination several times during follow-up to assess the influence of the use of free limbal conjunctival autograft on postoperative course. All 73 patients underwent slit lamp biomicroscopy and photography of both eyes to identify the clinical form and stage of the disease, and to assess (a) the shape of the head and body of pterygium, and (b) the state of the crescent fold and lacrimal caruncle. Inclusion criteria were primary or recurrent pterygium of stages 2 to 4 by the Dudinov and Tsepeniuk classification [12]. Exclusion criteria included a history of surgery other than limbal conjunctival autograft, presence of diabetes mellitus, impaired cardiac function, impaired renal function, etc. Biomicroscopy, fluorescein staining and ocular photography were used to investigate postoperative changes in the state of the eye. The first criterion to assess the effectiveness of surgery was corneal re-epithelialization rate at 24, 72 and 120 hours following LCAG surgery involving the use of HFWBS of the conjunctiva in the HFWBS group versus suture fixation in the control group. Fluorescein staining and ocular photography were used to assess corneal reepithelialization rate. The second criterion to evaluate the effectiveness of surgery was the degree of local inflammatory vascular response assessed by the conjunctival hyperemia score. Conjunctival hyperemia was scored as follows: 0, weak inflammatory response (pale pink conjunctiva and white sclera excepting insignificant injection at the graft site); 1, moderate pericorneal injection at the transplantation site and at the graft harvesting site (normal conjunctival and scleral color along the site of the excision); 2, marked pericorneal injection (injection of limbal vessels) at the transplantation site and at the graft harvesting site and a less pronounced injection at other sites (the graft is not elevated above surrounding tissue); 3, strong pink pericorneal injection along the site of the excision (the conjunctiva of the internal angle of the eye is hyperemic; the graft is swollen and is elevated above surrounding tissue). The third criterion - the degree of corneal syndrome (i.e., the triad of photophobia, tearing and blepharospasm) – was scored as follows: 1, quiet eye at the daylight and at the slit lamp light; 2, mildly irritated eye, mild blepharospasm, tearing and photophobia at the slit lamp light; 3, markedly irritated eye, marked blepharospasm, tearing and photophobia at the daylight. The fourth criterion of the efficacy of pterygium treatment – the level of corneal transparency at the site of excised pterygium – was scored as follows: 0, physiologically normal (the whole cornea is transparent); 1, mildly swollen cornea at the site of excised pterygium; 2, moderately swollen cornea, marked corneal edema or cloudy cornea at the site of excised pterygium. Efficacy of surgery for pterygium was assessed at predetermined observation time points (at early (days 1, 3 and 5) and late (months 1, 3 and 6) follow up). Statistical analysis was performed using nonparametric Mann-Whitney tests (including Mann-Whitney U test for independent samples). Contingency tables analysis was performed using Pearson's chi-square test. Differences were considered statistically significant when p < 0.05. Additionally, to demonstrate the level of difference in the effectiveness of pterygium treatment between the HFWBS group and controls, we used the repeated measures analysis of variance. Statistica10 and MedCal 9.2 software were used for statistical analysis of the data. Results At day 1, corneal re-epithelialization was not complete in any eye of either group. Additionally, biomicroscopy revealed that the corneal epithelium at the site of excised pterygium head was different from the rest of the cornea and was slightly opaque. At day 3, complete corneal re-epithelialization was significantly more often found in the HFWBS group (25/34 eyes; 73.5%; this fact was verified by negative fluorescein staining) than in controls (6/39 eyes; 15.4%). Therefore, the difference was 58.1%. (?2 = 25.1; р = 0.00001). At day 5, complete corneal re-epithelialization was also significantly more often found in the HFWBS group (30/34 eyes; 88.2%; corneal epithelium at the site of excised pterygium head was smooth, bright and transparent) than in controls (20/39 eyes; 51.3%). Therefore, the difference was 36.9% and it was statistically significant (?2 = 13.7; р = 0.00021).
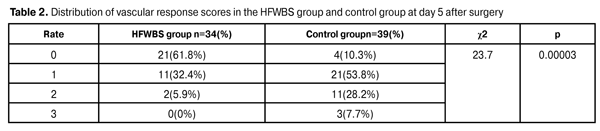
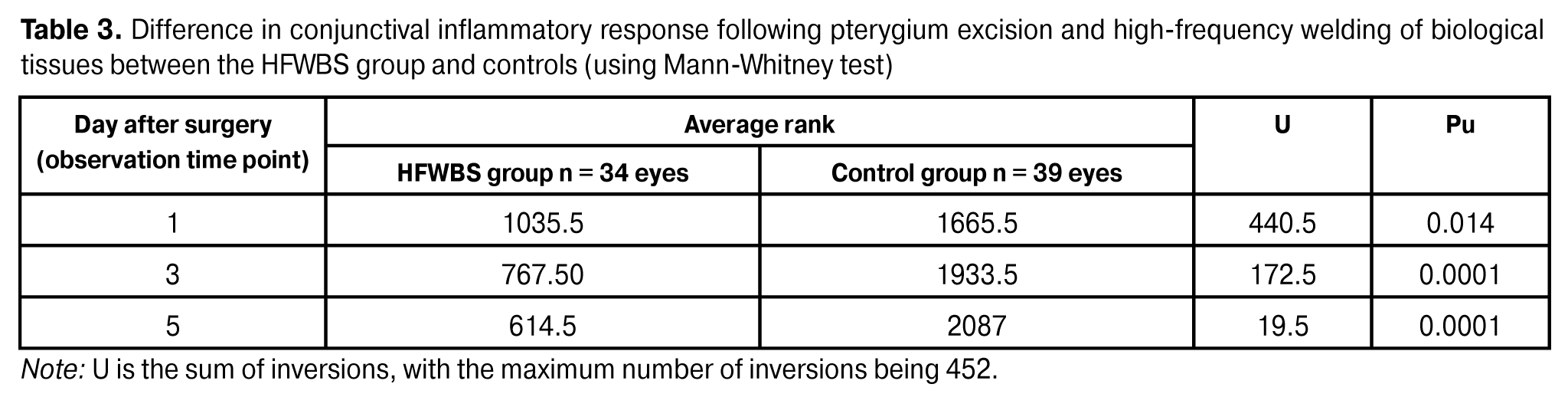
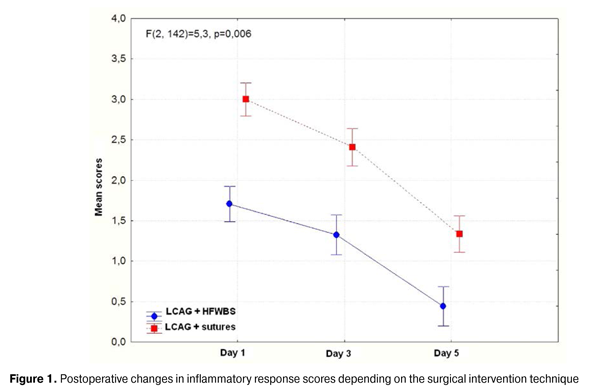
The degree of local inflammatory vascular response assessed by the conjunctival hyperemia score was different at days 1 to 5. At day 1, the conjunctival hyperemia score was 3 (strong pink pericorneal injection along the site of the excision, the conjunctiva of the internal angle of the eye is hyperemic, the graft is swollen and is elevated above surrounding tissue) in 4 eyes, 2 (marked pericorneal injection (injection of limbal vessels) at the transplantation site and at the graft harvesting site and a less pronounced injection at other sites (the graft is not elevated above surrounding tissue)) in 15 eyes, and 1 (moderate pericorneal injection at the transplantation site and at the graft harvesting site (normal conjunctival and scleral color along the site of the excision)) in 15 eyes of the HFWBS group. Additionally, a vivid local inflammatory vascular response was observed in 30/34 eyes (88.2%) of the HFWBS group versus 39/39 eyes (100%) of the controls. At day 3, the conjunctival hyperemia score was 3, 2 and 1 in 2, 7 and 25 eyes, respectively, of the HFWBS group vs 20, 13 and 6 eyes, respectively, of the controls. Therefore, a pronounced vascular response was observed in 9/34 (26.4%) eyes of the HFWBS group vs 33/39 eyes (84.6%) of the controls. The distribution of the scores of local inflammatory vascular response at day 5 is shown in Table 2. At day 5, the local inflammatory vascular response score was 3, 2, 1 and 0 in 0, 0, 11 and 21 eyes, respectively,of the HFWBS group vs 3, 20, 12 and 4 eyes, respectively, of the controls, and the difference in inflammatory response scores between the groups was statistically significant (?2 = 23.7; р = 0.00003). Additionally, firm adherence of the graft to the underlying sclera was found in all eyes of both groups, and no graft rejection was observed in any eyes of either group. It is noteworthy that weak neovascularization from near empty vessels was found at the site of graft harvesting and maintained up to 10 days following surgery. Table 3 presents the difference in conjunctival inflammatory response following pterygium excision and LCAG between the HFWBS group and controls. Therefore, in the HFWBS group, lower index values prevailed at all observation time points, which was statistically significant (Mann-Whitney test; Pu < 0.015). The repeated measures analysis of variance (Fig. 1) was used to demonstrate the difference in conjunctival inflammatory response between the HFWBS group and controls graphically, and to assess the difference in inflammatory response in either group. The diagram presents the postoperative difference in changes in inflammatory response scores between the intervention techniques. It is well seen that a significant difference in inflammatory response scores between the intervention techniques was observed as early as at the first observation time point and maintained at day 5.
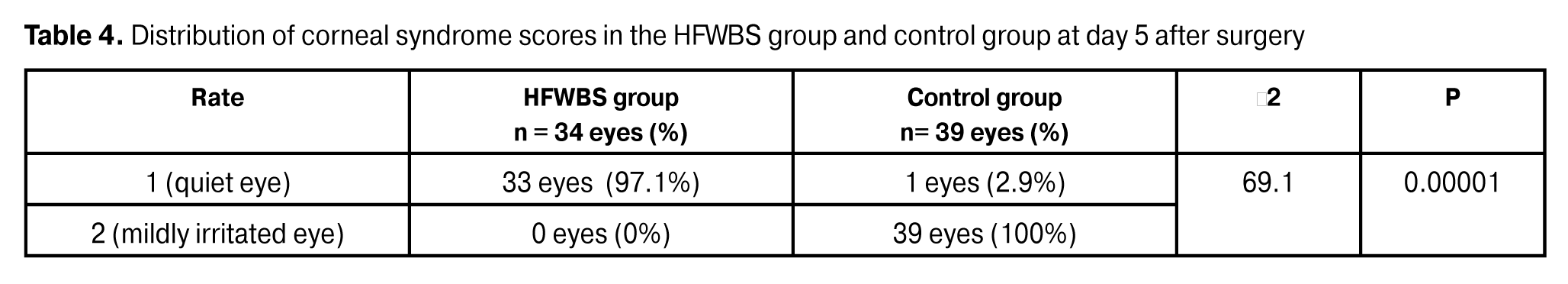
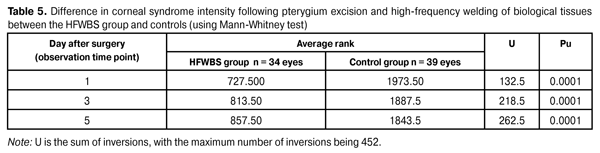
At day 1, the corneal syndrome score was 3 (i.e., markedly irritated eye, marked blepharospasm, tearing and photophobia at the daylight), 2 (i.e., mildly irritated eye, mild blepharospasm, tearing and photophobia at the slit lamp light), and 1 (i.e., quiet eye at the daylight and at the slit lamp light) in 17, 16, and 1 eyes, respectively, of the HFWBS group vs 29, 10, and 0 eyes, respectively, of the controls. At day 3, the corneal syndrome score was 3, 2, and 1 in 0, 7, and 27 eyes, respectively, of the HFWBS group vs 14, 19, and 6 eyes, respectively, of the controls. Therefore, a pronounced corneal syndrome was observed in 9/34 (26.4%) eyes of the HFWBS group vs 33/39 eyes (84.6%) of the controls.At day 5, the corneal syndrome score was 3, 2, and 1 in 0, 0, and 33 eyes, respectively, of the HFWBS group vs 0, 39, and 0 eyes, respectively, of the controls. Table 4 presents the distribution of corneal syndrome scores. At all observation time points from day 1 to day 5 postoperatively, the signs of blepharospasm, tearing and photophobia in the HFWBS group (i.e., the eyes that had undergone limbal conjunctival autograft with HFWBS) were statistically significantly less marked than in the control group (i.e., the eyes that had undergone LCAG with sutures) (?2 = 69.1; р =0.00001).
Table 5 presents the difference in corneal syndrome scores following pterygium excision and HFWBS in the HFWBS group and controls. Therefore, low index values prevailed in the HFWBS group at all observation time points, which was statistically significant (Mann- Whitney U test; Pu < 0.05).
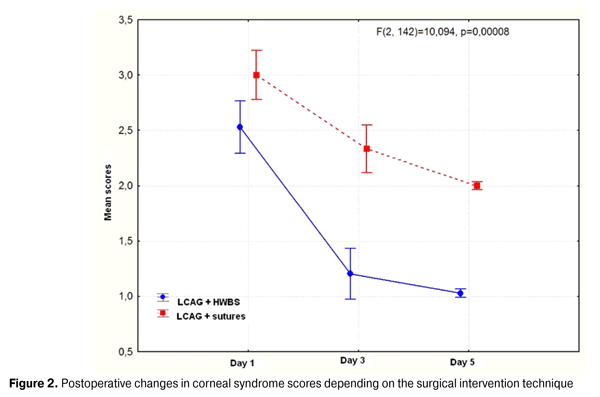
Figure 2 presents the findings of the repeated measures analysis of variance for postoperative changes in corneal syndrome scores. The diagram shows that mean corneal syndrome scores in the eyes that had undergone LCAG with HFWBS were significantly lower than in those that had undergone LCAG with sutures as early as at day 1, and this relationship maintained at day 5.
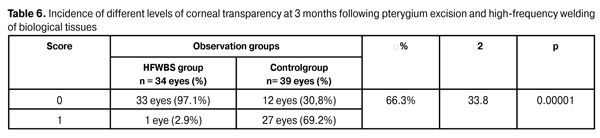
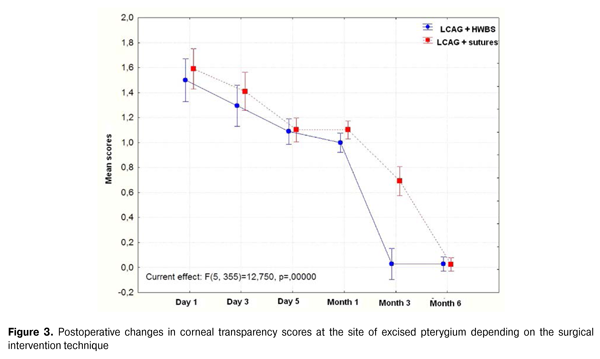
When assessing corneal transparency at the site of excised pterygium, we found that such cornealtransparency disorders as swollen cornea or corneal cloudiness can occur even a month following surgery, not to mention the early follow-up (i.e., day 1 to day 5 postoperative). At all these observation time points, the difference in corneal transparency scores was not statistically significant (р > 0.05). At month 3 postoperative, mean corneal transparency scores in the HFWBS group were better that in the controls (Table 6).
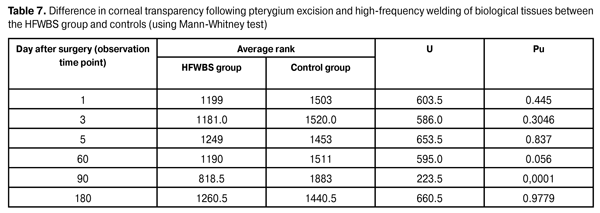
At this observation time point, the cornea was transparent in 33 eyes (97.1%) of the HFWBS group vs 12/39 eyes (30.8%) of the controls (?2 = 66.3; р = 0.00001), and only one patient of the HFWBS group exhibited mild corneal opacity. Only in one eye of the HFWBS group and in one eye of the controls, corneal cloudiness persisted for at least 6 months of the follow-up. Table 7 presents statistical differences in corneal transparency score between the HFWBS group and controls at each observation time point. The table shows that a statistically significant difference in corneal transparency score between the HFWBS group and controls was observed only at the month 3 time point (Pu < 0.05).
Figure 3 demonstrates postoperative changes in corneal transparency at the site of excised pterygium depending on the surgical intervention technique. The figure demonstrates no significant difference in corneal transparency score at the site of excised pterygium between the groups at all time points excepting the month 3 time point. Although the repeated measures analysis of variance of corneal transparency score at the site of excised pterygium (Fig. 3) demonstrates no significant difference in corneal transparency score at the early follow-up time points, the advantage of LCAG with HFWBS over LCAG with sutures at the month 3 time point is obvious.Discussion Clinical observations of this study give evidence of significantly lower clinical sign scores in eyes treated for pterygium with LCAG with HFWBS compared to those treated with LCAG with sutures in the early follow-up.
Re-epithelialization of the corneal surface was observed earlier in the HFWBS group than in the controls. Thus, corneal re-epithelialization was complete statistically significantly more often in Group 1 than in Group 2 at day 3 (25/34 eyes (73.5%) vs 6/39 eyes (15.4%); difference, 58.1%; ?2 = 25.1, р = 0.000001) and at day 5 (30/34 eyes (88.2%) vs 20/39 eyes (51.3%); difference, 36.9%; ?2 = 13.7, р=0.00021). Additionally, at day 5, patients of the HFWBS group had low scores of local inflammatory vascular response statistically significantly less often than controls (Pu < 0.015 according to Mann-Whitney test; ?2 = 23.7 and р = 0.00003 according to Pearson's chi-square test). Moreover, at day 1 to day 5, signs of corneal syndrome (photophobia, tearing and blepharospasm) were statistically significantly less marked in eyes treated with LCAG and HFWBS compared to those treated with LCAG with sutures. At day 5, 33/34 eyes (97.2%) of the HFWBS group were quiet at the daylight and at the slit lamp light, whereas 39/39 eyes (100%) of the controls were mildly irritated and exhibited mild blepharospasm, tearing and photophobia at the slit lamp light (?2 = 69,1; р =0.00001). When assessing corneal transparency at the site of excised pterygium, we found that swollen cornea or corneal cloudiness can occur even a month following surgery, not to mention the earlier follow-up. The intergroup difference was statistically insignificantduring the follow-up period (р > 0.05). Corneal transparence scores were better in the HFWBS group than in the controls only at one supervision time point (month 3). Thus, at this observation time point, the cornea was transparent in 33 eyes (97.1%) of the HFWBS group vs 12/39 eyes (30.8%) of the controls (?2 = 66.3; р=0.00001), and only one patient of the HFWBS group exhibited mild corneal opacity. Therefore, during the first three months of the follow-up, restoration of corneal transparency was observed 66.3% more often in the HFWBS group than in controls (?2 = 33.8; р = 0.00001). Based on the results presented above, we can make the following conclusions. Conclusions First, in limbal-conjunctival autograft (LCAG), the use of high-frequency welding of biological tissues (HFWBS) significantly improves the efficacy of surgical treatment of pterygium. At day 3, complete corneal reepithelialization was significantly more often found in the HFWBS group than in controls (73.5% vs 15.4%; difference, 58.1%). This difference remained statistically significant at day 5. Second, LCAG with HFWBS was found advantageous over LCAG with sutures in terms of vascular response at all observation time points. Thus, low vascular response scores were found statistically significantly more often in the HFWBS group than in the controls (Pu < 0.015). Third, LCAG with HFWBS was found advantageous over LCAG with sutures in terms of corneal syndrome. Thus, at day 5, practically all eyes (33/34 eyes (97.1%)) of the HFWBS group were quiet, whereas all eyes (39/39 eyes (100%)) of the controls were mildly irritated (?2 = 69.1; р = 0.00001). Finally, at month 3, restoration of corneal transparency was observed in the HFWBS group 66.3% more often than in controls (?2 = 33.8; р = 0.00001), thus supporting the advantage of HFWBS in terygium treatment with LCAG. References 1. Borodin IuI, Val’skii VV, Verigo EN. [Late outcomes of combination treatment of recurrent pterygium]. Oftalmologiia. 2007;3(4):29-33. Russian 2. Veselovs’ka ZF et al. [Microsurgical technique for treatment of pterygium]. In: [Proceedings of the 2nd Congress of Black Sea Ophthalmological Society]. Odessa: Filatov Institute of Eye Disease and Tissue Therapy; September 8-10, 2004. p.18-9. Ukrainian 3. Iakimenko SA. [Surgical treatment for persistent recurrent pterygium]. Zdravokhr Turkmen. 1983;11:41-2. Russian 4. Gris O, Guell JL, del Campo Z. Limbal-conjunctival autograft transplantation for the treatment of recurrent pterygium. Ophthalmology. 2000 Feb;107(2):270-3. 5. Isyaku M. Treatment of pterygium. Annals African Medicine. 2011;10(3):197-203 6. Ye J, Kook KH, Yao K. Temporary amniotic membrane patch for the treatment of primary pterygium: mechanisms of reducing the recurrence rate. Graefes Arch Clin Exp Ophthalmol. 2006 May;244(5):583-8. 7. Maltsev EV, Usov VIa, Krytsun NI. [Current techniques for treatment of pterygium]. Oftalmol Zh. 2012;3:72-80. Ukrainian 8. Bakbardina LM, Bakbardina II. [Peripheral barrier keratoplasty with biologically protected tissue bed in treatment of recurrent pterygium]. Oftalmol Zh. 2004;5:83-5. Russian 9. de Wit D, Athanasiadis I, Sharma A, Moore J. Sutureless and glue-free conjunctival autograft in pterygium surgery: a case series. Eye (Lond). 2010 Sep;24(9):1474-7. 10. Umanets NN. [High-frequency welding of biological tissues (upgraded generator EK-300M1) versus diathermocoagulation: influence on duration of hemorrhage from major retinal vessels in a rabbit model of intraocular hemorrhage]. Oftalmol Zh. 2012;4:88-91. Russian 11. Maltsev EV, Usov VIa, Krytsun NI. [Determination of optimal electric current parameters in use of highfrequency welding of biological tissues for sealing the edges of surgical wound of conjunctiva]. Oftalmol Zh. 2013;3:78-82. Ukrainian 12. Dudinov SA. [Pterygium Classification: Methodology Guide]. Moscow; 1973. p25-7. Russian 13. Usov VIa, Maltsev EV, Krytsun NI. [Pterygium surgery technique involving use of high frequency welding of biological tissues for fixing free limbal conjunctival autograft]. Oftalmol Zh. 2015;2:10-5. Ukrainian |