J.ophthalmol.(Ukraine).2015;6:64-67.
|
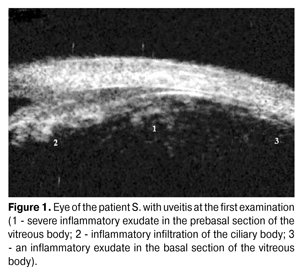
https://doi.org/10.31288/oftalmolzh201566467 Changes in the basis of vitreous body in case of uveitis treated by adalimumab N.V. Panchenko, Doctor of Medical Sciences, prof., T.A. Khramova, PhD in Medical Sciences, A.I. Litvishchenko, MD, G.S. Sarkisian, MD, M.N. Samofalova, MD, E.N. Gonchar, PhD student, M.V. Friantseva Kharkov National Medical University Kharkov(Ukraine) Keywords: uveitis, Adalimumab, changes in the basis of vitreous body Objective of the research is to study the dynamics of changes in the basis of vitreous body in case of uveitis treated by Adalimumab. Material and methods. 5 year old patient S. with recurrent anterior uveitis on the background of juvenile arthritis was observed. Results. After 4 months of treatment by Adalimumab (20 mg 1 time every 2 weeks combined with methotrexate 10 mg 1 time a week) an exudate has reabsorbed in the prebasal sections of the vitreous body, and after seven months - in the basal ones. During the year no uveitis exacerbations were checked. Conclusions. When uveitis is treated by Adalimumab the exudate is reabsorbed more slowly in basal sections of the vitreous body. Usage of Adalimumab in the treatment of uveitis is effective and in combination with methotrexate helps to prevent relapses. Introduction According to modern concepts, tumor necrosis factor - alpha (TNF-?) plays an important role in the pathogenesis of uveitis. Investigations have found elevated levels of TNF-? both in the blood and in the anterior chamber liquid [1, 9, 14] in patients with uveitis, and usage of TNF-? blockers is one of the most promising directions in the treatment of uveitis. Adalimumab is a fully humanized recombinant monoclonal antibody to TNF-?, which correspond in structure to the human immunoglobulin G1, which determines its low immunogenicity and reduces the frequency of allergic reactions. This structure allows counting on good tolerability of the drug. Analysis of the world literature concerning the treatment by Adalimumab of the patients with uveitis suggests that today it is fairly common alternative drug for treatment uveitis which is refractory to standard treatment in adults [8] and children [4, 7, 15]. In ophthalmic Ukrainian literature there are no data about particularities of usage of Adalimumab in patients with uveitis. We have not found any studies of the dynamics of changes in the basal cells of the vitreous body with uveitis during the treatment by Adalimumab in the available literature. The objective of this work was to study the dynamics of changes in the basis of vitreous body with uveitis, treatment by Adalimumab. Material and methods We observed the patient S. 5 years old (at the moment of the first inspection) with recurrent anterior uveitis on the background of juvenile arthritis (JA). Juvenile arthritis was diagnosed at the age of two years, uveitis was diagnosed at the age of four years, and the disease was complicated by the presence of partial cataract. The patient was examined using conventional clinical and ophthalmological methods. Ultrasound biomicroscopy was performed using the machine "VuMax II" (Sonomed Inc., USA) sensor with a frequency of 50 MHz. According to the FDA (Food and Drug Administration), the recommended dose of Adalimumab (Humira, “Abbott Laboratories”) for children from 4 years is determined by body weight: 15 to 30 kg – 20 mg 1 time in two weeks, subcutaneously is prescribed; body weight is 30 kg or more - 40 mg 1 time in two weeks. Our patient was prescribed Adalimumab 20 mg 1 time in 2 weeks subcutaneously (in the course of the treatment with methotrexate 10 mg 1 time per week) [16]. Results and discussion The diagnosis of JA in our patient was made in 2010. Uveitis firstly occurred in April 2012, at the age of 4 years, which is consistent with the literature that the major risk factor for uveitis on the background of JA is the age under 7 years [12] and in the infancy of JA uveitis may be asymptomatic [4]. At the same time approximately in 12-38% of patients with JA uveitis occurs within 7 years after beginning of arthritis [18]. During this period, there was a unilateral uveitis of the eyes in the patient S., which is not very typical for uveitis with JA, since, according to the available data, in most cases it is a bilateral process [4, 19]. Progression of uveitis with a lesion of contralateral eye is often noted during the first 12 months [23], contrary to the case which we observed. According to the literature in most cases uveitis with the SA is anterior [19], which was observed in our patient. The clinical picture of uveitis in the patient S. was characterized by the presence of circumcorneal flush, which is often expressed in children with uveitis on the background of JA, by swelling of the iris, precipitates on endothelium of the cornea, "soft" iris adhesions, frequently observed at this disease [11] and by the reduced visual acuity. Development of such complications of the disease as glaucoma and keratopathy was not observed in our patient. During the first examination (before prescription of methotrexate), according to the UBM (Fig. 1) there was a severe inflammatory exudate in the projection of the vitreous body in prebasal and basal sections, inflammatory infiltration of the ciliary body. Starting from the second month of anti-inflammatory therapy and the use of topical steroids, methotrexate 10 mg 1 time per week was added.
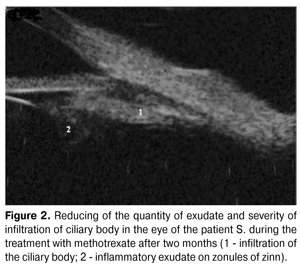
Two months later, on the background of the treatment with methotrexate (Fig. 2) the quantity of inflammatory exudate and severity of infiltration of the ciliary body have decreased, but there was moderate accumulation of fine divided inflammatory suspended matter in the basal sections of the vitreous body and some exudate which persisted on zonule of zinn. At this a complete remission of uveitis has not been reached. According to the data described by Chylack LT [5], the lack of effect of topical steroids is recorded within 6 months from the beginning of their use in almost 1/3 of the patients, which is evidenced in our clinical case. Reports about methotrexate suggest that its prescription does not provide complete control of inflammation; it does not reduce the need for systemic and topical steroids, and does not reduce the frequency of relapses of uveitis in about a half of patients with uveitis on the background of JA [10].
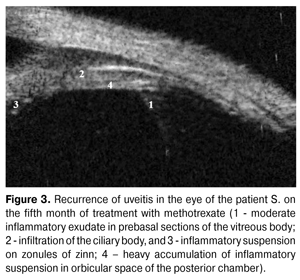
During the fifth month of our treatment (NSAIDs, topical steroids and methotrexate) according to clinical manifestations and results of UBM there was aggravation of uveitis, which is confirmed by the literature about recurrent or chronic nature of inflammatory process in JA [5] and lack of effectiveness of the applied treatment. At the same time, according to UBM, the inflammatory exudate appeared in prebasal and basal sections of the vitreous body (Fig. 3). Recurrence of uveitis was complicated by formation of partial posterior subcapsular cataract.
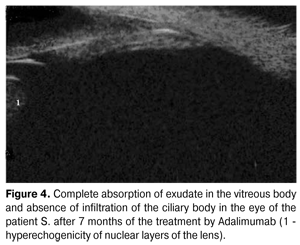
Considering the presence of relapse during the treatment with methotrexate, in five months Adalimumab 20 mg 1 time in two weeks subcutaneously was prescribed additionally. The patient S. already on the second week of treatment showed clinical improvement: morning stiffness has disappeared, range of motion in the joints significantly increased. During the control ophthalmological study there was noted disappearance of the circumcorneal flush and photophobia, precipitates on endothelium of the cornea have reabsorbed. According to UBM in 4 months exudate in prebasal sections of the vitreous body has reabsorbed and its quantity in basal sections has decreased. Against the background of this therapy a complete relief of inflammatory process and significant improvement in visual acuity has been achieved. After 7 months of the usage of Adalimumab an exudate in basal and prebasal sections of the vitreous body has reabsorbed completely (Fig. 4), inflammatory infiltration of the ciliary body was not observed.
Our results confirm the opinion to the researchers about good tolerability and efficacy of treatment by Adalimumab in patients who do not respond to standard therapy including nonsteroidal anti-inflammatory agents, systemic steroids and/or methotrexate, including patients in early childhood [15]. According to Vazques-Cobian LB et al. (2006) [22], Adalimumab reduced the severity of inflammation in 80.8% of cases, and according to Beister S et al. (2007) [3] – in 88% of cases in children with uveitis on the background of JA, according to other researchers on the background of the treatment by Adalimumab reduced activity of uveitis was noted in 35-57% of eyes [7, 13, 21], at the absence of serious side effects. Negative dynamics of the inflammatory process during the treatment by Adalimumab was observed in 5-20% of eyes [7, 13, 21]. Small number of studies is dedicated to the combined application of Adalimumab with methotrexate [13, 17]. Researchers have noted that usage of Adalimumab in monotherapy leads to increased formation of antibodies to the drug (25.6%) and significant reduction of its efficiency, in contrast to the combination of Adalimumab and methotrexate (5.9%) [17]. During the supervision of up to one year no exacerbations of uveitis were observed in our patient. Lack of uveitis relapse during the treatment by Adalimumab is consistent with the data of Simonini G et al. (2011) [20] about the longer periods of remission of uveitis during the treatment by Adalimumab. At the same time we cannot confirm the opinion of Foster CS et al. (2003) [6] that additional prescription of TNF-? blockers does not affect the frequency of relapses of uveitis treated with methotrexate. Conclusions Our observations confirm the data that treatment by Adalimumab has a positive effect on the quality of life of patients with uveitis and juvenile arthritis, improves physical activity and emotional state. Study of the dynamics of changes in the basis of vitreous body during the treatment of uveitis with Adalimumab showed that exudate retains longer in the basal sections of the vitreous body. It was found that the use of TNF-? blocker Adalimumab is effective in the treatment of uveitis, and in combination with methotrexate helps to prevent the relapse of the disease.
References
|