J.ophthalmol.(Ukraine).2015;6:50-53.
|
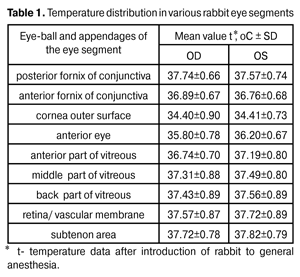
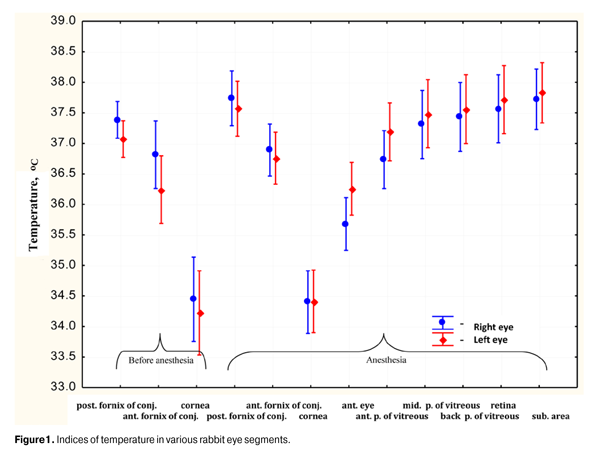
https://doi.org/10.31288/oftalmolzh201565053 Original device and approaches to the study of temperature distribution in various eye segments (experimental study) L.I. Anatychuk 1, Academician NAS and MES of Ukraine N.V. Pasyechnikova 2, Doctor of Medical Sciences, Professor, Associate Member of NAMS of Ukraine O.S. Zadorozhnyy 2, PhD in Medical Sciences, R.E. Nazaretyan 1, ophthalmologist, V.V. Myrnenko 2, Head of Organizational and Methodological Department, R.R. Kobylyanskyi 2, PhD in Physical and Mathematical Sciences, N.V. Gavrilyuk 2 1 Institute of Thermoelectricity of National Academy of Sciences and Ministry of Education and Science of Ukraine, Chernovtsy, Ukraine 2 SI “The Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”, Odessa, Ukraine. E-mail: rudolph84@mail.ru Keywords: thermoelectric device, temperature, thermocouple, rabbit eye. Introduction. Today the question of temperature distribution in various eye segments of human and animals remains understudied. Objective. To design the device for measuring intraocular temperature and to study in the experiment the principle of temperature distribution in various segments of rabbit eye. Material and methods. Experiment was carried out on 11 rabbits (22 eyes). For temperature measurement the thermoelectric device was designed, which consists of temperature registration module, measure probes of 0.7 mm in diameter and computer with software. Results. Under ambient temperature 23.8°C, the temperature of various eye segments was the following: posterior fornix of conjunctiva ? 37.41°C; anterior fornix of conjunctiva ? 36.82оС; cornea surface ? 34.41оС; ocular anterior chamber ? 35.97оС; anterior part of vitreous ? 36.96оС; of middle part of vitreous ? 37.40оС; back part of vitreous ? 37.50оС; of retina/ vascular membrane ? 37.64оС; subtenon area ? 37.78оС. Temperature difference of cornea external surface and ocular anterior chamber was 1.56оС, and of cornea external surface and retina was 3.23оС. Conclusion. Thermoelectric device, which helps to make measurements in various eye segments, was designed. Due to this device the temperature distribution in rabbit eye was studied in vivo. Relevance In literature there are data on dynamics of biochemical processes, and haemo- and hydrodynamic indices of healthy eye under the influence of high and low temperatures on the eye [1, 2, 3]. But until now the question of temperature distribution in various segments of eyes of animals and human remains understudied. For measurement of eye temperature noncontact and contact methods were used. Noncontact methods (for example, infrared thermography) allowed estimating only the temperature of outer surface of the eye [4]. For measurements of intraocular temperature contact invasive methods were used, a number of devices and measure probes were designed [5, 6, 7]. However proposed devises and measurement methods had major deficiencies, as measure probes were made of material with high thermal conduction, which led to errors in temperature measurements, and surgical exposure methods considerably influenced to registered data [8]. Hence, development of new measuring devices with taking into consideration known deficiencies, and optimization of surgical exposure methods at temperature measurement in various eye segments will allow increasing the accuracy of registered intraocular temperatures. Knowing the principles of intraocular temperature distribution of outer and inner eye segments in different environmental conditions, in norm and in pathology, with exposure of physical factors to the eye, will allow the development of mathematical model of intraocular temperature distribution. Developed computer model will be possible to use as an alternative method of intraocular temperature estimation, for example, in modeling of thermal processes in the eye under the influence of different physical factors. Objective. To design the device for measuring intraocular temperature and to study in the experiment the principle of temperature distribution in various segments of rabbit eye. Material and methods Experiment was carried out together with the Institute of Thermoelectricity of National Academy of Sciences and Ministry of Education and Science of Ukraine and SI “The Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”. For temperature measurement the thermoelectric device was designed, which consists of microprocessing temperature registration module, thermocouple measuring microprobes, attaching device and computer with software for visualization and registration of temperature indices in real-time operation mode. Microprobes temperature sensors are made on the basis of L-type thermocouples (chromel-copel). Sensor probe was located in the shell of standard polytetrafluorethylene cannula of 0.7 mm in diameter. Thermocouple seam was welded to the thermoconcentrator made of medical stainless steel and fastened on the edge of cannula needle. Cable and cannula seam was hermetically sealed with the medical silicone sealer, which was chemically neutral and was appropriate for thermal or chemical sterilization of the item (as ordinary medical device). Docking device was equipped with copper thermoconcentrator in which there was a precision temperature sensor (platinum resistance thermometer). The temperature of “cold” edges of thermocouples - reference temperature was measured. Microprocessing temperature registration module was made on the basis if Triton-9004T device, which has 8-channel 24-bit analog-digital converter. Designed device allows making measurements (with regularity of 4 seconds) within temperature range from 10°С to +120°С with deviation ± 0.08°С. Biomicroscopy and ophthalmoscopy was made for all experimental animals. During surgical interference general anesthesia by intramuscular injections of 10% solution of thiopental sodium in dosage 1.0 ml for 1 kg of animal weight were used. On surgical interference preparation step and during surgery the instillation of 0.5% solution of proxymetacaine hydrochloride to both eyes with regularity of 20 minutes was made. According to aseptic and antiseptic rules rabbits were given instillations of 20% solution of sulfacyl sodium and 0.3% of ofloxacin after surgical interference. In vivo experiment on 11 rabbits (22 eyes) of Chinchilla breed (age – 1 year, weight – 3.5-4 kg) after epibulbar anesthesia temperature measurements of outer surface of cornea by direct contact with probe end were made. Temperature registration was carried out in real-time operation mode in 4 seconds not less than five measurements in each segment. Further, the temperature was registered by placing measure probe in posterior fornix of conjunctiva, and then in anterior fornix of conjunctiva. After rabbit introduction to general anesthesia the temperature was measured in outer surface of cornea and in conjunctival fornix and then after forming of surgical access, the temperature was measured in anterior eye, in anterior, middle and back part of vitreous, in retina/ vascular membrane, in subtenon area. Measure probe was injected in anterior eye through tunnel paracentesis of 0,7 mm, in vitreous body – through sclerotomy of 0,6mm in diameter in view of ciliary apparatus plateau in 2-3 mm from limb. The probe was injected in subtenon area through conjunctival cut in upper inner quadrant. Rabbit rectal temperature, temperature and humidity level of air in the room were also measured. Experimental study was carried out at ambient temperature on the average 23.8±0.6оС, at relevant air humidity on the average 80.7±1.6%, at average rectal temperature of rabbit – 38.73±0.94оС. Activities with experimental animals were carried our according to European Convention for the Protection of Vertebrate Animals Used for Experimental and other Scientific Purposes (Strasburg, 1986) and Law of Ukraine “On Protection of animals from cruelty” (2006). The software Statistica 10.0 was used for study processing. Results The temperature of various eye segments, registered in the experiment, is shown in the Table 1.
Significant differences in temperature values of left and right eye of experimental animals in analysis of obtained results were not found. This concerns either to outer eye segments, in which measurements were made (posterior fornix of conjunctiva, anterior fornix of conjunctiva, outer surface) or inner rabbit eye segment (anterior eye, different parts of vitreous, retina/ vascular membrane, subtenon area). Temperature difference in eye segments was verified in the experiment. So, as expected, the lowest temperature was on cornea outer surface. The temperature of cornea outer surface, measured after introduction of animals to general anesthesia, at the average was 34.41±0.80оС, and was considerably lower than the temperature of posterior and anterior fornix of conjunctiva (р<0.0001). After introduction of animals to general anesthesia the temperature of posterior fornix of conjunctiva was 37.65±0.70оС and was considerably higher than the temperature of anterior fornix of conjunctiva – 36.82±0.66оС (р<0.0001). The temperature of anterior rabbit eye was higher than the temperature of cornea outer surface and at average was determines on the level 35.97±0.73оС (р<0.0001). Therefore the temperature difference between cornea outer surface and anterior eye was 1.56оС. The temperature of anterior part of vitreous was higher relative to anterior eye for 36.96±0.77оС (р<0.0001), and of middle part of vitreous at average for 37.40±0.87оС (р<0.0001). Temperature gradient between anterior eye and middle part of vitreous was 1.43оС. Maximum intraocular temperature was fixed in contact of measure probe with retina and was in average 37.64±0.87оС. The temperature of subtenon area was 37.78±0.77оС, and was considerably higher than the temperature of retina (р=0.65). Thus, the temperature gradient in outer surface of cornea and retina was 3.23 оС, and in outer surface of cornea and subtenon area was 3.37оС. During the experiment there were registered two cases of perioperative accidents, such as incomplete hemophthalmia during forming of surgical access, and one case of retinal separation in postoperative period. Discussion In 1962 V. Schwartz and M. R. Feller issued their project about temperature measurement of various eye segments of white New Zeeland rabbits. The authors used the device on the basis of termistor and several modified measure probes for measuring the intraocular temperature. As a probe for intraocular temperature registration a metal needle of 7.62 cm long and 0.7 mm in diameter was used. Measures in various eye segments were carried out by step-by-step injection of the probe along the axis of the eye through cornea, eye-lens, vitreous body and retina to the eye socket. The ambient temperature was in the range of 22 to 24оС, relative air humidity was 33-53%. Rectal temperature of seven experimental animals after introduction of animals to general anesthesia on the average was 39.13оС. The following average data was obtained as the result of measurements: the temperature of cornea outer surface – 32.30±0.49оС, of posterior conjunctival sac – 38.74±0.54оС, of anterior chamber – 32.98±0.74оС, of eye-lens 35.42±1.0оС, of middle part of vitreous – 36.56±0.9оС, of retina/ vascular membrane – 37.03±0.86оС, of eye socket – 37.68±0.71оС. Besides, authors did not fix considerable temperature differences in left and right eye of animals in all segments excluding cornea outer surface [7]. In 1083 D. R. May with co-authors determined the influence of perfusion of anterior chamber by irrigating solutions of different temperatures on the changes of the temperature in eye segments of Holland rabbits. In the project the thermometer, made on the basis of thermocouple, which was a metal probe with blunt head of 0.64 mm in diameter and 2.5 sm long. Measurement deviation of the thermometer was ±1°C. Air temperature was 25оС. Rectal temperature after introduction of experimental animals to general anesthesia was in average 39,4оС. The authors gave the following average initial indices of the temperature of various eye segments: anterior chamber – 32.5оС, anterior of vitreous body – 35.0оС, back of vitreous body – 36.6оС, retina – 36.8оС [5]. It is necessary to note, that metal probes with high thermal conduction were used in these projects. Besides, in the project of D. R. May with co-authors for irrigation/aspiration of anterior chamber before temperature measurements two holes of cornea with metal needles of 0.7 and 0.8 mm in diameter were made, and then one of the holes was spread with the metal scissors up to 3 mm. According to the data of experimental (in vitro) and theoretical investigations, which were carried out by I. Fatt and J. F. Forester in 1972, it was well known that the temperature indices of eye tissues, registered with metal probes, as compared with temperature indices, registered with probes with low thermal conduction can be lower for several degrees [8]. In our project the temperature, registered in anterior eye chamber was 35.97оС and turned to be higher as compared with data issued before (32.5оС in D. R. May project and 33оС in B. Schwartz project) approximately for 3-3.5оС. Appreciable differences in temperature indices, registered in anterior eye chamber were probably connected with small moisture amount in anterior rabbit eye chamber, which was 0.25–0.3 ml, and with direct contact of cornea with environment. That was why insertion of metal tool into anterior chamber for forming of surgical access and metal measure probe led to considerable heat loss and resulted lower temperature registration. In our project measure probe was made of polytetrafluorethylene with low thermal conduction, and a minimum surgical access, needed only for thermoprobe insertion was formed, which resulted to reduction of heat loss on the moment of temperature measurement and registration of higher indices. In a smaller degree heat loss was noticeable in temperature measurement in vitreous body of rabbit, as its volume was 1-1.5 ml and there was no direct contact of vitreous body with environment. In our project the temperature in middle part of vitreous was 37.4оС and in less degree differed from the data of abovementioned authors (35.5 and 36.56оС). Hence, the volume of surgical intervention while forming of access to various eye segments and surgical tools made of material with high thermal conduction considerably influenced to registered intraocular temperature indices. The material of probe for intraocular temperature measurements also considerably influenced to registered data. Conclusions 1. Thermoelectric device with software for measuring of temperature in various eye segments with high accuracy in real-time operation mode was designed. 2. Thermoelectric measure probe made of the material with low thermal conduction, which increases the measurement accuracy by reducing the heat loss during the registration of intraocular temperature, was designed. 3. In vivo experiment using designed device the principles of temperature distribution of various eye segments were studied. Thus, at ambient temperature 23.8оС, the temperature difference of outer and inner cornea surface and rabbit eye retina was 3.23оС.
References
|