J.ophthalmol.(Ukraine).2015;5:72-76.
|
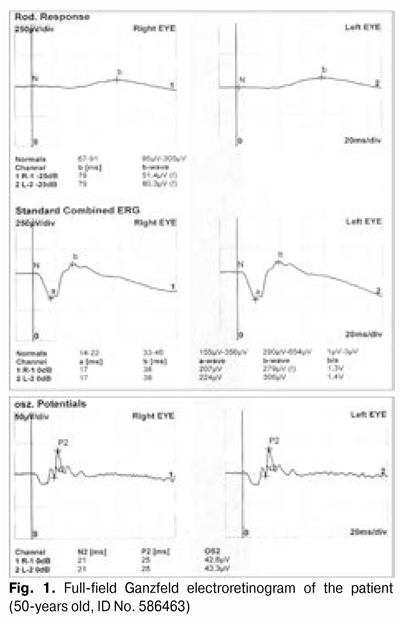
https://doi.org/10.31288/oftalmolzh201557276 Diagnosis and treatment of normal tension glaucoma: a case report VS Ponomarchuk, Dr. Sc. (Med), Prof., N.V. Konovalova, Dr. Sc. (Med), N.I. Khramenko, Cand. Sc. (Med), O.A. Peretiagin, Cand. Sc. (Med), Ie.V. Ivanitskaia, Cand. Sc. (Med), N.I. Naritsyna, Cand. Sc. (Med) Filatov Institute of Eye Diseases & Tissue Therapy of the NAMS of Ukraine (Odessa) E-mail: khramenkon@gmail.com Background: Normal tension glaucoma (NTG) is the form of the disease in which damage to the optic nerve occurs at normal intraocular pressure levels. According to Levene, four times as many patients in the over 40 age group have NTG as have high tension glaucoma, accounting for 2% of the Japanese population. Purpose: To present a clinical case exemplifying the diagnosis and treatment of NTG. Materials and Methods: The patient underwent assessment of the level of visual acuity, ophthalmoscopy, intraocular pressure and visual field examination, and optical coherent tomography (OCT). Results: The patient was diagnosed with NTG. The clinical diagnosis was confirmed by examinations performed (i.e., ophthalmic rheography, OCT, visual field perimetry and ocular tonography). Keywords: normal tension glaucoma Introduction Recently, the concept of glaucoma has changed tremendously. Currently, glaucoma includes a group of diseases accompanied by characteristic changes in the visual field and optic disc, although until recently, the main criterion for the disease was increased intraocular pressure (IOP). It has been established that when IOP increases to about 30 mm Hg, a vascular tone disorder occurs, resulting in optic nerve hypoperfusion. At the same time, glaucoma can develop when untreated IOP is within a statistically normal range (i.e., average daytime IOP is equal to or less than 21 mm Hg). Normal tension glaucoma (NTG) is primary open-angle glaucoma with glaucomatous optic disc excavation and visual field defects, however, with a normal IOP. According to Levene (1980), four times as many patients in the over 40 age group have NTG as have high tension glaucoma (HTG), accounting for 2% of the Japanese population [1]. The reasons for the development of NTG are still being studied; some patients are genetically predisposed to optic nerve damage even at normal IOP. Evidence has been reported that the individual IOP tolerance of the optic disc may result from the individual architectonic features of the lamina cribrosa. Abnormal blood flow in the vessels supplying the optic nerve is one of a number of factors resulting in such a course of glaucoma [1,2]. It has been supposed that abnormal blood flow in the optic disc is one of the major causes for NTG. In the opinion of a number of authors, this results from the imbalance in the nitric oxide-endothelin-1 (ET-1) system. Elevated ET-1 plasma levels have been revealed in some NTG patients without the presence of any systemic vascular pathology or systemic blood circulation disorders [1]. Arterial blood flow abnormalities due to stenosis of or atherosclerotic alterations in major cranial arteries reduce the tolerance of the optic nerve to raised IOP. Arterial blood pressure (ABP) levels have been found to be reduced apparently at night compared with day, and diastolic blood pressure levels have been found to be reduced in a number of NTG cases. Additionally, POAG and NTG patients with arterial hypertension undergoing hypotensive therapy have been found to have a tendency for visual field reduction and disease progression, with apparent reduction in systolic blood pressure at night [1]. Risk factors for NTG include hemodynamic crises (episodes of massive blood loss or hypotensive shock), alterations in blood rheology, elevated blood and plasma viscosity, and a tendency for hypercoagulation. Spasms in the vessels supplying the optic nerve are important, resulting in its ischemia and reduction in its resistance to raised IOP. Convincing associations have been drawn between NTG and Raynaud’s phenomenon [1]. In NTG patients, episodes of headache – often migrainous – as well as decreased finger capillary flow in response to cold tend to occur more frequently. Apparent neuroretinal rim loss and increased peripapillary atrophy are characteristic for NTG. This is probably due to a relatively late diagnosis for this form of glaucoma, since it is often diagnosed only after the occurrence of central scotoma. Optic nerve head hemorrhages are more common in NTG patients, and hemorrhages have been found to have a prognostic value for them. Geijssen and Greve (1995) believe that NTG patients can be divided into three distinct groups according to their optic disc appearance—focal ischemic, senile sclerotic, and myopic. Excavation of the optic disc is an optic disc pit associated with a partial loss of nerve fibers and IOP-induced deformation of the lamina cribrosa. The extent of disc cupping in NTG is often greater than would be expected from the size and depth of the visual field defect present. Additionally, a very deep excavation and grey color of the optic nerve disc (a cupped appearance of the optic nerve) in NTG patients should raise suspicion of stenosis in major cranial arteries. Visual field defects in these cases often approach the fixation point, sometimes with no significant change in the size of peripheral temporal visual field. It has been found that NTG patients exhibit a more apparent and sudden decrease in light sensitivity, with visual field defects located closer to the fixation point, compared with HTG patients. These differences appear to be associated with differences in age and IOP between NTG and HTG patients, since, e.g., more diffuse visual field defects are characteristic for younger age groups and patients with higher IOP [3]. In NTG, deterioration of the visual field usually occurs gradually, whereas in HTG, loss of visual functions may occur early (in acute attack, within a few hours). Lowering IOP by 25% to 30% reduces NTG progression. The purpose of the study was to present a clinical case exemplifying the diagnosis and treatment of normal tension glaucoma. Materials and Methods A 50-year old man (ID 586463) presented to us in the Inflammatory Ocular Pathology Department of the Institute with complaints of a long history of progressive visual acuity loss in the August of 2014. He had a five year history of treated hypertony (Prestarium, Servier, France; 5 mg a day). He had been seeking medical advice from local ophthalmologists and complaining for visual acuity and field loss for three years prior to the presentation to us, but no cause for his progressive optic nerve atrophy could be established. A local doctor diagnosed him with “optic nerve atrophy and hypermetropia”, and the patient received some treatment for his disease, however, without any success. His vision continued to decrease and this was accompanied by progressive alterations in visual field and optic disc. He sought medical advice at our institute. At out institution, the patient underwent assessment of the level of visual acuity; ophthalmoscopy; IOP measurements in the early morning hours while he was still lying on his back in bed; ocular tonography with the TNC-100 (Samara Electromechanical Factory, Russia) electronic tonograph; visual field perimetry with the projection perimeter; spectral-domain optic coherent tomography (SD-OCT) with the Spectralis (Heidelberg Engineering, Dossenheim, Germany); ophthalmic rheography; and complex electrophysiological examination with mfERG (RETIscan, Roland Consult, Wiesbaden, Germany). On examination, both eyes had clear, spherical corneas, initial lens opacities, and vitreal floaters. Additionally, both optic discs had diffuse pallor and were excavated, with vascular trunk displacement, narrowed arteries, full veins and the retinal artery to vein (A : V) caliber ratio of 1:4. Gonioscopy revealed open drainage angles in both eyes. The patient’s uncorrected visual acuity (UCVA) was 0.04 OD and 0.02 OS, and the best corrected visual acuity (BCVA) was 0.1 with 3.0 D sph OD and 0.12 with 3.0 D sph OS. The right eye visual field was reduced by 20 degrees superiorly, 30 degrees inferiorly, 45 degrees temporally and 35 degrees nasally. The left eye visual field was reduced by 25 degrees superiorly, 30 degrees inferiorly, 40 degrees temporally and 35 degrees nasally. IOP OD was 19.0 mmHg, and IOP OS was 20.0 mmHg, when measured with Maklakov applanation tonometer. The ocular tonography measurements were as follows: theoretical IOP (P0), 20.0 mm Hg (OD) and 20.0 mm Hg (OS); aqueous outflow easiness coefficient (C), 0.16 mm3 (OD) and 0.41 mm3 (OS); Becker’s coefficient (P0/C), 140 mm Hg/ mm3 (OD), 167 mm Hg/ mm3 (OS); and aqueous humor production (F), 1.53 mm3/min (OD); 1.53 mm3/min (OS). The indices of the full-field Ganzfeld electroretinogram (gERG) related to the peripheral retina were not different significantly from those of normal individuals of the patient’s age (Fig. 1).
The photopic gERG demonstrated that the level of activity of inner macular layers was adequate, whereas that of photoreceptor layer was significantly (two times) lower than normal (Fig. 2).
The 2-Hz and 12-Hz flash-elicited visual evoked potentials (VEP) demonstrated the following: N1-P1 amplitudes for the right visual cortex and left visual cortex were five times and three times, respectively, higher than normal values, whereas N1-P1 implicit time was 11% to 53% increased compared with normal values (Fig. 3).
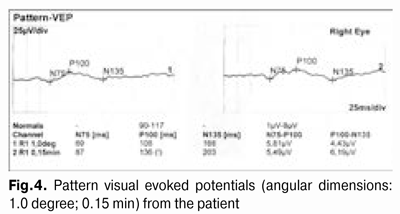
In the patient’s pattern VEP (angular dimensions: 1.0 degree; 0.15 min), P100 amplitudes for the right visual cortex and left visual cortex were two times lower than normal values, whereas the implicit time was 19% to 40% increased compared to normal values (Fig. 4).
Ophthalmic rheography showed that the pulsatile blood flow (rheographic coefficient RQ) in the right eye and left eye was decreased by 30% (RQ=1.9‰) (Fig.5 a) and by 25% (RQ=2.7‰) (Fig.5 b), respectively, compared to normal values, with apparently increased vascular tone of arteries in both eyes (alpha1 percentage index was 25% higher than normal values). SD-OCT showed no evidence of focal retinal macular changes in both eyes; however, the foveal surface appeared relatively smooth due to thinned inner retinal layers. The right and left vertical cup-disc ratios were 0.64 and 0.86, respectively. The thickness of retinal peripapillary nerve fibers in the temporal quadrant was decreased as compared to normal values, which was more apparent in the left eye. Enhanced depth imaging (EDI) SD-OCT found the patient’s subfoveal choroidal thickness to be 218.4 ?m (OD) and 207.8 ?m (OS) (as compared to the mean normal value of 291±66 ?m reported by Korol et al [4]). These findings confirm the occurrence of initial optic nerve atrophy in both eyes, with the involvement of the axial bundle and macular photoreceptor complex (macular retinopathy) in the presence of reduced blood flow and vascular tone abnormalities in both eyes. Interestingly, that if OCT-based morphology fails to reveal thinning of outer retinal layers (mostly, that of the outer nuclear retinal layer), the significant decrease in bioelectric activity of the photoreceptor layer revealed by the analysis of gERG may indicate severe metabolic alterations in the posterior eye associated with blood flow disorder, the latter being a possible manifestation of the choroidal thinning in both eyes. Based on the data above, the patient was diagnosed with primary open-angle (normal tension) glaucoma, partial optic nerve atrophy, and moderate hypermetropy. He received an in-patient course of neuroprotective therapy including vitamins of the B group, retinal protective and angioprotective agents. Currently, he receives a drop of Taflotan two times a day. The right eye visual field was reduced by 20 degrees superiorly, 30 degrees inferiorly, 45 degrees temporally and 25 degrees nasally. The left eye visual field was reduced by 25 degrees superiorly, 30 degrees inferiorly, 20 degrees temporally and 40 degrees nasally. The OCT showed that the right and left vertical cup-disc ratios were 0.62 and 0.47, respectively. IOP OD was 17.0 mmHg, and IOP OS was 18.0 mmHg, when measured with Maklakov applanation tonometer. The ocular tonography measurements were as follows: theoretical IOP (P0), 16.9 mm Hg (OD) and 16.2 mm Hg (OS); aqueous outflow easiness coefficient (C), 0.22 mm3 (OD) and 0.21 mm3 (OS); Becker’s coefficient (P0/C), 79 mm Hg/ mm3 (OD), 76 mm Hg/ mm3 (OS); aqueous humor production (F), 1.61 mm3/min OD; 1.23 mm3/min OS. Therefore, the clinical diagnosis was confirmed by examinations performed (i.e., ophthalmic rheography, OCT, visual field perimetry and ocular tonography). Conclusion The case presented is an example of correct diagnosis and treatment of normal tension glaucoma. At follow-up visits during 9 months after in-patient treatment, no further deterioration in the patient’s vision functions was found. We found evidence of stabilization of all the following indices: visual acuity, visual field, and OCT, ocular tonography, and ophthalmic rheography indices. Achieving a 25%-30% reduction in IOP reduces progression of normal tension glaucoma. We hypothesize that if OCT-based morphology fails to reveal thinning of outer retinal layers (mostly, that of the outer nuclear retinal layer), the significant decrease in bioelectric activity of the photoreceptor layer revealed by the analysis of gERG may indicate severe metabolic alterations in the posterior eye associated with ocular blood flow disorder, the latter being a possible manifestation of the choroidal thinning in both eyes. References 1. Kamal D, Hitchings R. Normal tension glaucoma – a practical approach. Br. J. Ophthalmol. 1998;82 (7):835-40. 2. Nesterov AP. [Main principles of diagnosis of primary open-angle glaucoma]. Vestn Oftalmol. 1998 Mar-Apr;114(2):3-6. Russian. 3. Egorov EA, Alyab'eva ZhYu. [Normal Tension Glaucoma: Pathogenesis, Clinical and Treatment Features]. In: [Proceeding of the Conference Glaucoma: Outcomes and Prospects at the Turn of the Millennium]; 1999 Nov 22-24; Moscow (Russia): Helmholz Moscow Research Institute of Eye Diseases; 2006. p.123. Russian. 4. Korol AR, Khramenko NI, Zadorozhnyi OS, Kustrin TB. [Choroidal thickness and blood supply in patients with age-related macular degeneration]. Oftalmol Zh. 2013;3:23-27. Russian.
|