J.ophthalmol.(Ukraine).2015;4:55-59.
|
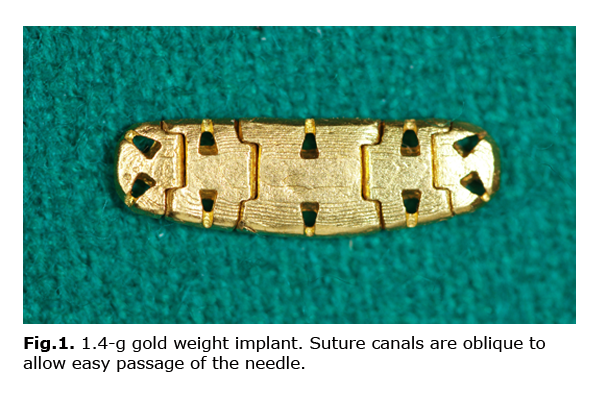
https://doi.org/10.31288/oftalmolzh201545559 Modern Methods of Repair of Paralytic Lagophthalmos Ia.O. Grusha1,2, N.S. Iskusnykh1 1RAMS Research Institute of Eye Diseases, 2I.M. Sechenov First Moscow State Medical University E-mail: grusha-y@mail.ru Keywords: paralytic lagophthalmos, facial nerve palsy, gold implant, lower lid ectropion correction, tarsorrhaphy. Paralytic lagophthalmos (PL) is a rather common pathology dealt by ophthalmologists, neurologists, maxillofacial, and, certainly, ophthalmic plastic surgeons. This specific disease occurs in patients who underwent neurosurgery or complicated midface surgery, and in those with many other conditions [1]. PL management is based on obtaining improved eyelid closure with cosmetically acceptable narrowing of the palpebral fissure and “a stable cornea”. In this review we hope to share our knowledge of a variety of details involved in planning and implementation of the surgical treatment of PL [2]. Lubrication with tear drops and other cornea wetting agents (during the day) and ointment (at night) is a cornerstone of treatment for patients with PL. The lower eyelid is elevated with plaster, if required. Since the n. petrosus superficialis major is responsible for secretory innervation of the lacrimal gland, any involvement of this nerve will drastically reduce tear production and may require temporary or permanent punctal occlusion or tarsorrhaphy. Soft contact lenses may be used for PL treatment and prevention, but due to poor lens retention and special care requirements, most patients refrain from wearing them. In severe corneal damage, moisture chambers are applied for ocular surface protection. External eyelid weights offer some convenience to the patient and can be placed by him for a short time or for a day. The weight can be secured to the upper eyelid skin with a double-sided plaster, and its front surface can be painted with the color matching the patient’s skin tone [3]. A known method for temporary eye protection is injecting botulinum toxin type A (BTX-A) into the lavator palpebrae superioris muscle. The technique aims to induce protective upper eyelid ptosis; however, giving a prognosis for the palpebral fissure size at the outset is deemed impossible [4, 5, 6]. In acute facial paralysis, use of hyaluronic acid gel has been proposed for temporary correction of lagophthalmos [7]. Unlike the injection of BTX-A, the injection of this gel provides a fast dose-dependent and more durable effect (typically, up to 6 months). The gel is beneficial for the patients with corneal involvement [7, 8]. Surgical procedures for the management of facial paralysis may be classified as either dynamic or static. Although the former are promising to recover facial muscle functions and symmetry, the evidence supporting these interventions for the repair of lagophthalmos is still to be determined. According to the Burdenko Neurosurgery Institute authors, only 2 out of 28 patients showed improvement in eyelid closure 28 months following facial nerve re-innervation by the descending branch or trunk of hypoglossal nerve [9]. A cross-facial nerve graft from the contralateral facial nerve appears preferable to other dynamic methods that have evolved over the last decade. It should, however, be noted that most elder patients with compromised somatic state are poor candidates for dynamic procedures. A substantial disadvantage of these procedures is that their final outcomes have to be waited for at least 12 months of the potential gradual improvement. Fifth cranial nerve involvement in facial paralysis often prevents maintenance of normal palpebral fissure width due to damage to or loss of protective mechanisms. Neuroparalytic corneal ulcers may either aggravate or alleviate the problem of impaired eyelid closure. According to Kasparov and colleagues, in such eyes, therapeutic keratoplasty does not prevent recurrence of exposure and/or neurotrophic ulcers, and the most effective approach to correction is to combine autoconjunctival grafting with a simultaneous eyelid plasty [10]. Tarsorrhaphy is a commonly used method to correct PL on a temporary or permanent basis, and should be considered as a procedure of choice in cases with corneal involvement, including those waiting for upper eyelid implantation, dynamic procedures or the outcomes of the latter [1, 3, 11, 12, 13]. The suture tarsorrhaphy may be done in patients with gradual deterioration of the corneal state, poor general condition (e.g., following neurosurgery or trauma), inadequate behavior, or when the midface lift is unavailable to the patient. A minimal 4-mm external tarsorrhaphy has been shown to result in a 25% improvement in the rate of corneal involvement in lagophthalmos patients with facial paralysis [1]. External tarsorrhaphy is used in patients with keratopathy or small corneal erosions, whereas a complete “bloody” tarsorrhaphy with the lids sutured together for a period of up to a year is recommended and generally provides a complete corneal epithelialization in persistent corneal erosions or ulcers. If a chance to restore the cornea has been preserved, central tarsorrhaphy is appropriate, and allows examining the corneal state and saving a part of the visual field. It should be noted that it is crucial to perform suture tarsorrhaphypromptly after neurosurgery complicated by impaired eyelid closure. It is important to correct the lower eyelid malposition. In elder patients, the stretched lower lid generally requires for tarsal strip horizontal eyelid shortening, elevated fixation to the periosteum or to the bone of the lateral orbital wall. In young patients, the lower eyelid usually remains adapted to the eye, but becomes a bit sunken. Therefore, in such patients with high esthetic requirements, placement of lower eyelid spacers is advised. In some cases, medial cantorraphy is preferred as the first stage of correction. Further correction(exterior tarsopexy and external tarsorrhaphy) may facilitate lower eyelid lifting and achieving near-normal eyelid position with respect to the limbus. Although this approach is accompanied by horizontal palpebral fissure shortening, it provides very good cosmetic results in some cases. In high-grade prosoplegia, the above-mentioned lower lid lifting, however, may become ineffective. A solution is to perform facelift surgery [14]. The patient’s transportability, distance from the clinic, and the availability of treatment are factors to consider in treatment planning. If the indices of these factors are poor in the patient with PL, one should use proper approaches for the reliable prevention of corneal complications. Radial sutures (allotendinous or synthetic) are advised for palpebral fissure narrowing. This approach generally results in a better cosmetic outcome than does external tarsorrhaphy alone. However, with the use of radial sutures, complete elimination of lagophthalmos is unlikely. Sutures cancut through the soft ocular tissues and eyelid skin when overtightened, typically at medial canthus (a kind of locus minoris) [15]. In some countries, eyelid palpebral springs are used for PL management. Although their use does provide some significant advantages, spring displacement and exposure through the skin are still very often observed [16]. Placement of various grafts (auricular cartilage, allocartilage, etc.) into the upper eyelid is a still commonly used surgical approach to correcting lagophthalmos [17]. However, the upper eyelid implant prominence, if severe, may cause substantial esthetic defects. Moreover, as the cartilage resorbs, the amount of postoperative lagophthalmos increases, whereas the defects do not improve. It is generally agreed that currently, the gold standard for treating PL is the noble metal eyelid implantation. The beneficial effect of gravity on the patient with metal weight implant occurs only when he is in the vertical position. In 2009, such an implant was developed by the authors at the Research Institute of Eye Diseases (manufacturer, OJSC SIC Supermetal, Russia). The implant is made of 99.99% gold and represents a flexible chain composed of several interconnected links with holes (Fig. 1). One can vary the weight of the implant to be assembled from 0.6 to 2.0 g by varying the number of links and the weight of the link used. The optimal implant weight for the patient is selected preoperatively on an individual basis. Metal weight implantation is predictable, easy to perform, and generally advantageous for cosmetic reasons. The implant is placed on the tarsal plate of the upper eyelid and each link is fixed to the underlying tissues. The eyelid tissues are then closed in layers [18].
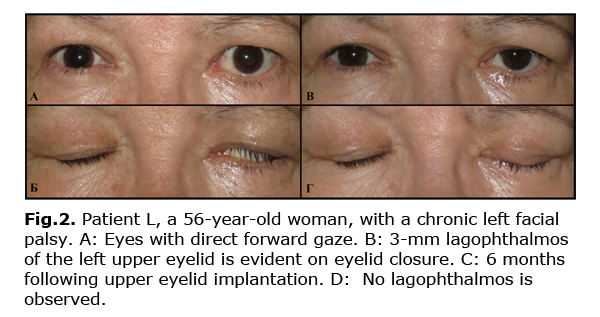
Over the last decade, we have operated on about 400 patients with PL at the Research Institute of Eye Diseases. At the beginning of that period, we used different tarsorrhaphy techniques combined with ectropion repair or radial suture passage, or upper eyelid retraction repair. Additionally, some patients underwent suture midface lift. In more recent years, gold weight implantation has become our procedure of choice for managing PL. Thus, in 60 patients, the implantation of the gold weight developed by the authors was the only method used for the correction of PL. At the 6 month follow-up, the lagophthalmos and palpebral fissure narrowing in down gaze in these patients were found to be significantly (p<0.05) reduced from 5.44±2.62 mm to 0.24±0.71 mm, and from 4.57 mm to 1.39 mm, respectively, with the mean decrease in upper eyelid position of 1.88 mm (Fig. 2). Therefore, gold weight implantation provided reduction in or elimination of lagophthalmos, improvement in the biomechanics of the upper eyelid, and had a low complication rate.
Although the approaches to the PL management have been modified significantly, the primary treatment goal is still the same: to prevent corneal involvement. We have to note that, whether the dynamic methods are really effective for correction of PL is still to be determined, and little is known about their long-term outcomes. The neuroplastic or myoplastic approaches used by maxillofacial surgeons are justified for rehabilitation of the facial nerve. Methods of static correction for PL are, however, more reliable and predictable than dynamic ones. In PL, various approaches may be used to narrow the palpebral fissure. Modern approaches envisage not only modeling of the palpebral fissure with account of the state of the eye and the features of its adnexa, but also influencing biomechanics of paralyzed eyelids.
References 1. Grusha IaO. [Conceptual basics of paralytic lagophthalmos correction]. Vestn Oftalmol. 2013;129(5):92-6. Russian. 2. Pereira MV, Gloria AL. Lagophthalmos. Semin Ophthalmol. 2010 May;25(3):72-8. 3. Grusha IaO, Ivanchenko IuF. [Facial nerve palsy: topographic features of the damage]. Vestn Oftalmol. 2009;125(3):59-61. Russian. 4. Tabashnikova TV, Serova NK, Shimanskii VN. [Trophic keratopathy management and lagophthalmos correction in neurosurgical patients]. Oftalmol Vedom. 2013;6(4):9-15. Russian. 5. Maio M. Facial palsy and asymmetries. In: Ascher B, Landau M, Rossi B, eds. Injection Treatments in Cosmetic Surgery. 2nd ed. United Kingdom: Informa Healthcare;2008. p.173-9. 6. Y?cel OE, Art?rk N. Botulinum toxin-A-induced protective ptosis in the treatment of lagophthalmos associated with facial paralysis. Ophthal Plast Reconstr Surg. 2012 Jul-Aug;28(4):256-60. 7. Grusha IaO, Ismailova DS, Ivanchenko IuF, Afafonova EI. [The first experience in using the stabilized hyaluronic acid preparation to correct lagophthalmos]. Vestn Oftalmol. 2010;126(1):39-42. Russian. 8. Mancini R, Taban M, Lowinger A. et al. Use of hyaluronic Acid gel in the management of paralytic lagophthalmos: the hyaluronic Acid gel “gold weight”. Ophthal Plast Reconstr Surg. 2009 Jan-Feb;25(1):23-6. 9. Tabashnikova TV, Serova NK, Shimanskii VN. [Dynamics of lagophthalmos depeding on facial nerve repair and its intraoperative monitoring in neurosurgical patients.] Zh Vopr Neirokhir Im N N Burdenko. 2014;78(4):67-70. Russian. 10. Kasparov AA, Kasparova EA, Sobkova OI. [Treatment for central corneal ulcer in the presence of lagophthalmos by autoconjunctivoplasty in combination with optic iridectomy and external blepharorrhaphy a clinical case]. Vestn Oftalmol. 2010;126(2):35-7. Russian. 11. Chang L, Olver J. A useful augmented lateral tarsal strip tarsorrhaphy for paralytic ectropion. Ophthalmology. 2006;113 (1):84-91. 12. Mocan MC, Erdogan-Poyraz C, Erdener U et al. Comparison of the outcomes of internal-fixation versus bolster-suture tarsorrhaphy. Ophthal Plast Reconstr Surg. 2007 May-Jun;23(3):222-4. 13. Tan ST, Staiano JJ, Itinteang T et al. Gold weight implantation and lateral tarsorrhaphy for upper eyelid paralysis. J Craniomaxillofac Surg. 2013 Apr;41(3):e49-53. 14. Malakhovskaia VI, Nerobeev AI, Bragina EI. [Minimally invasive methods of surgical correction in rehabilitation of the patients with facial nerve damage]. In: Proceedings of the Third National Congress of Plastic Surgery; 11-14 December; Moscow, Russia; 2013. p.76. Russian. 15. Bergeron CM, Moe KS. The evaluation and treatment of upper eyelid paralysis.Facial Plast Surg. 2008;24(2):220-30. 16. Demirci H, Frueh BR. Palpebral spring in the management of lagophthalmos and exposure keratopathy secondary to facial nerve palsy. Ophthal Plast Reconstr Surg. 2009; 25(4):270-5. 17. Friedhofer H, Coltro PS, Vassiliadis AH. et al. Alternative surgical treatment of paralytic lagophthalmos using autogenic cartilage grafts and canthopexy. Ann Plast Surg. 2013 Aug;71(2):135-9. 18. Grusha IaO, NovikovIA, Afafonova EI. [The first experience of using an implant for upper eyelid loading in paralytic lagophthalmos]. Vestn Oftalmol. 2012;128(1):41-43. Russian.
|