J.ophthalmol.(Ukraine).2020;1:10-13.
|
http://doi.org/10.31288/oftalmolzh202011013 Received: 30 December 2019; Published on-line: 21 February 2020
Ocular heat exchange indices in terminal neovascular glaucoma patients with proliferative diabetic retinopathy O.S. Zadorozhnyy, Cand Sc (Med); O.V. Guzun, Cand Sc (Med); T.B. Kustrin, Cand Sc (Med); A.R. Korol, Dr Sc (Med); V.A. Naumenko, Dr Sc (Med), Prof.; N.V. Pasyechnikova, Associate Member of the NAMS of Ukraine, Dr Sc (Med), Prof. Filatov Institute of Eye Diseases and Tissue Therapy, National Academy of Medical Science; Odesa (Ukraine) E-mail: zadoroleg2@gmail.com TO CITE THIS ARTICLE: Zadorozhnyy OS, Guzun OV, Kustrin TB, Korol AR, Naumenko VA, Pasyechnikova NV. Ocular heat exchange indices in terminal neovascular glaucoma patients with proliferative diabetic retinopathy. J.ophthalmol.(Ukraine).2020;1:10-13. http://doi.org/10.31288/oftalmolzh202011013
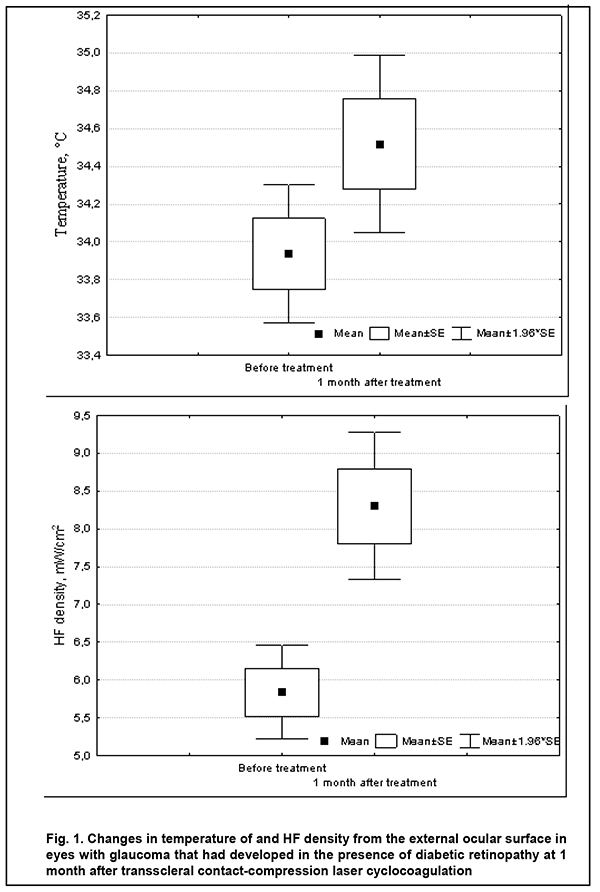
Background: The heat processes in patients with diabetes mellitus are still poorly understood. Purpose: To examine temperature of and heat flow (HF) density from the ocular surface in the eyes of patients with neovascular glaucoma that had developed in the presence of proliferative diabetic retinopathy (PDR). Material and Methods: In this open pilot study, 25 patients (50 eyes) with PDR in both eyes were under observation. In each patient, one eye was diagnosed with terminal neovascular glaucoma, and received laser treatment that included three sessions of transscleral contact-compression laser cyclocoagulation (TSCC LC). Before and 1 month after laser treatment, patients underwent examinations in both eyes as follows: best-corrected visual acuity testing, intraocular pressure (IOP) measurements, and measurements of temperature of the external corneal surface and HF density from the eye. Results: Before laser treatment, mean corneal surface temperature and mean HF density from the eye in glaucomatous eyes were 33.9 ± 0.9°С and 5.8 ± 1.6 mW/cm2, respectively, and were lower than in the fellow eyes (34.4 ± 1.0°С (p = 0.08) and 6.9 ± 1.4 mW/cm2 (p = 0.02), respectively). At 1 month after laser treatment, in glaucomatous eyes, mean IOP decreased from 36.3±5.4 mmHg to 25.8±4.6 mmHg (p =0.000), mean corneal surface temperature increased to 34.5 ± 0.9°С (p = 0.06), and mean HF density from the eye increased to 8.3±1.99 mW/cm2 (p =0.000). Conclusion: In patients with terminal neovascular glaucoma in one eye only, there was an asymmetry in ocular heat exchange indices between glaucomatous eyes and fellow eyes (with normal IOP). In addition, an increase in HF density from the eye in the presence of decreased IOP in eyes with terminal neovascular glaucoma after transscleral contact-compression laser cyclocoagulation seems to result from an increased intraocular thermal gradient in the presence of improved ocular hemodynamics Keywords: temperature of the external ocular surface, heat flow density, rheoophthalmography, diabetic retinopathy, terminal neovascular glaucoma
Introduction Heat exchange processes in biological objects (e.g., cells, organs and bodies) are subject to the laws of thermodynamics that studies general regularities of energy transformation and transmission. Biological objects could be considered as the open thermodynamic systems that are not under heat equilibrium conditions and in which heat transfer always takes place [1-3]. Heat transfer requires the existence of a thermal gradient that is a heat flow (HF) condition. HF, as opposed to temperature, has a certain direction, and is directed toward a decrease in temperature. A notion of HF density is used as a quantitative measure of heat distribution intensity. HF density is defined as an amount of heat flowing through a unit of isothermic area within a defined unit of time [3]. A thermal gradient between the outer and inner eye portions has been demonstrated in experimental studies [4]. Previously, we have reported the first results of direct HF density measurements in the ocular surface in healthy individuals, and found a relationship between the individual’s age and ocular HF density [5]. Our preliminary data demonstrated, in patients with diabetic retinopathy, there was a statistically significant difference in ocular HF density, but not in corneal temperature between patients differing in disease stage. In addition, we noted a relationship between ocular HF density and rheographic coefficient (RQ) as assessed by rheoophthalmography [6]. The heat processes in patients with diabetes mellitus, however, are still poorly understood [7]. The purpose of the study was to examine temperature of and HF density from the ocular surface in the eyes of patients with neovascular glaucoma that had developed in the presence of proliferative diabetic retinopathy (PDR). Material and Methods This open pilot study followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee of the Filatov Institute. Written informed consent was obtained from all individuals enrolled in the study. Twenty-five patients (50 eyes; age, 32 to 64 years; mean age, 54 ± 9.1 years) with PDR in both eyes were under observation. In each patient, one eye was diagnosed with terminal neovascular glaucoma. Not later than one month before the study, each patient had undergone anterior panretinal laser photocoagulation which did not result in complete regress of new vessels and normalization of intraocular pressure (IOP). In each patient, to reduce IOP, the study eye received twice-a-day instillations of brimonidine, a carbonic anhydrase and beta-blocker inhibitor. The fellow eye, however, received no medical agent instillation. Patients underwent examinations in both eyes as follows: best-corrected visual acuity testing, IOP measurements, and measurements of temperature of the external corneal surface and HF density from the eye. The thermoelectric device developed within the framework of the partnership agreement between the Institute of Thermoelectricity of the NAS of Ukraine and MES of Ukraine and the Filatov Institute of the NAMS of Ukraine was used for measurements of temperature of the external ocular surface and HF density from the eye [5]. Studies were performed under stable environmental conditions (air temperature and humidity control and minimal indoor air velocity). During the study period, the mean temperature in the room was 22.5 ± 1.7 °С. Before evaluation, patients spent 15 minutes indoors for adaptation to the room environment. Patients were administered epibulbar anesthesia with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®, SA Alcon-Couvreur NV, Puurs, Belgium). Temperatures and HF density were recorded 15 minutes after instilling a drop of the anesthetic. During data acquisition, patients were positioned before a slit-lamp apparatus. The prism-transducer assembly was attached to the conventional prism mount of the Goldmann tonometer, and the thermoelectric HF transducer came into direct contact with the subject’s central cornea in all cases. At least three real-time measurements were obtained for each eye. Corneal surface temperature, HF density from the eye and IOP were assessed before and at 1 month after laser treatment. Laser treatment included three sessions of transscleral contact-compression laser cyclocoagulation (TSCC LC) using a Neodymium: yttrium-aluminum-garnet (Nd: YAG) laser with ?=1064 nm and with a 600 µm quartz fiberoptic polymer contact probe for dosed compression of the sclera. Impulse laser energy was 0.8 J [8]. A TSCC LC was performed every other day. Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. Means and standard deviations (SD) were calculated. The Student t-test was used to assess post-treatment changes in IOP, corneal surface temperature, and HF density from the eye. The level of significance p ? 0.05 was assumed. Results Best-corrected visual acuity of all affected eyes remained as a perception of light with an inaccurate projection of rays. Before laser treatment, mean IOP in glaucomatous eyes was 36.3±5.4 mmHg, and in fellow eyes, 18.3 ± 2.8 mmHg (p = 0.00). In addition, mean corneal surface temperature in glaucomatous eyes was 33.9 ± 0.9°С, and in fellow eyes, 34.4 ± 1.0°С (p = 0.08). Moreover, mean HF density from the eye in glaucomatous eyes was 5.8 ± 1.6 mW/cm2, and in fellow eyes, 6.9 ± 1.4 mW/cm2 (p = 0.02). At 1 month after treatment, mean IOP in glaucomatous eyes decreased from 36.3±5.4 mmHg to 25.8 ± 4.6 mmHg (p = 0.00), i.e., by 10.5 mmHg (29%), and mean IOP in the fellow eyes was 19.1 ± 2.4 mmHg. In addition, mean corneal surface temperature in glaucomatous eyes was 34.5 ± 0.9°С, and in fellow eyes, 34.2 ± 0.7°С (p = 0.38). Moreover, mean HF density from the eye in glaucomatous eyes was 8.3 ± 1.99 mW/cm2, and in fellow eyes, 7.03 ± 1.9 mW/cm2 (p = 0.07). Fig. 1 presents changes in mean corneal surface temperature and mean HF density from the eye after treatment with TSCC LC.
No corneal trauma or other complications were observed in any patient during HF density examination. Discussion In patients with terminal neovascular glaucoma in one eye only, there was an asymmetry in ocular heat exchange indices between glaucomatous eyes and fellow eyes (with normal IOP). We found that the former eyes had lower mean corneal surface temperature and lower mean density of HF from the ocular surface compared to the latter eyes, possibly mainly due to a severe impairment in hemodynamics induced by elevated IOP and leading to changes in intraocular thermal gradient. Previously, an animal study by Auker and colleagues [9] has already showed an effect of increasing IOP on choroidal blood flow and ocular tissue temperature. In addition, a recent study by Konieczka and co-authors [10] has confirmed our previous hypothesis that the use of certain IOP-lowering eye-drops may result in a decrease in ocular surface temperature [11]. In the current study, we noted a tendency to an increase in ocular surface temperature in glaucomatous eyes at 1 month after TSCC LC, which is in agreement with our previous findings [10]. We noted also a significant increase in HF density from the eye in the presence of a decrease in IOP, which indicates that an increase in intraocular thermal gradient took place after laser treatment, because it is known that HF density from the eye increases with an increase in temperature difference (i.e., thermal gradient) [3]. Therefore, compared to corneal temperature, HF density from the eye may reflect, more comprehensively, ocular heat exchange [6]. An increase in ocular heat exchange indices in eyes with terminal neovascular glaucoma after TSCC LC seems to result from improved ocular hemodynamics in the presence of a decrease in IOP. Thus, there have been reports on increased ocular surface temperature after surgical treatment for glaucoma [12]. Conclusion First, in patients with terminal neovascular glaucoma in one eye only, there was an asymmetry in ocular heat exchange indices between glaucomatous eyes and fellow eyes (with normal IOP). Thus, corneal surface temperature and HF density from the eye in the former eyes (33.9 °C and 5.8 mW/cm2, respectively) were lower than in the latter eyes (34.4 °C and 6.0 mW/cm2, respectively). Second, an increase in HF density from the eye in the presence of decreased IOP in eyes with terminal neovascular glaucoma after transscleral contact-compression laser cyclocoagulation seems to result from an increased intraocular thermal gradient in the presence of improved ocular hemodynamics.
References 1.Savvin VN, Korotkova OL, Shishkin GP. [Use of thermodynamic approaches in assessment of the state of living systems]. Viatskii meditsinskii vestnik. 2017; 2:40-44. Russian. 2.Lucia U. Bioengineering thermodynamics of biological cells. Theor Biol Med Model. 2015 Dec 1;12:29. doi: 10.1186/s12976-015-0024-z. 3.Kudinov VA, Kartashov EM, Stefaniuk EV. [Technical thermodynamics and heat transfer]. Textbook for Academic Baccalaureate. Мoscow: Iurait; 2019. Russian. 4.Schwartz B, Feller MR. Temperature gradients in the rabbit eye. Invest Ophthalmol. 1962 Aug;1:513-21. 5.Anatychuk LI, Pasyechnikova NV, Naumenko VА, Zadorozhnyy OS, Gavrilyuk MV, Kobylianskyi R.R. A thermoelectric device for ophthalmic heat flux density measurements: results of piloting in healthy individuals. J Ophthalmol (Ukraine). 2019; 3:45-51. 6.Anatychuk LI, Pasyechnikova NV, Naumenko VА, Zadorozhnyy OS, Hramenko NI, Kobylianskyi RR. Temperature of and heat flux density from the external ocular surface in diabetic retinopathy patients: a pilot study. J Ophthalmol (Ukraine). 2019; 6:3-5. 7.Kenny GP, Sigal RJ, McGinn R. Body temperature regulation in diabetes. Temperature. 2016;3(1):119-45. 8.Chechin PP, Guzun OV, Khramenko NI, Peretyagin OA. Efficacy of transscleral Nd:YAG laser cyclophotocoagulation and changes in blood circulation in the eye of patients with absolute glaucoma. J Ophthalmol (Ukraine). 2018; 2:34-9. 9.Auker CR, Parver LM, Doyle S, et al. Choroidal blood flow. I. Ocular tissue temperature as a measure of flow. Arch Ophthalmol. 1982; 100:1323-6. 10.Konieczka K, Koch S, Hauenstein D, et al. Effects of the glaucoma drugs latanoprost and brimonidine on corneal temperature. Trans Vis Sci Tech. 2019 May; 8(3): 47. doi: 10.1167/tvst.8.3.47. 11.Zadorozhnyy OS, Guzun OV, Bratishko AIu, Kustrin TB, Nasinnik IO, Korol AR. Infrared thermography of external ocular surface in patients with absolute glaucoma in transscleral cyclophotocoagulation: a pilot study. J Ophthalmol (Ukraine). 2018; 2:23-2. 12.Galassi F, Giambene B, Corvi A, et al. Retrobulbar hemodynamics and corneal surface temperature in glaucoma surgery. Int Ophthalmol. 2008 Dec;28(6):399-405.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|