J.ophthalmol.(Ukraine).2019;2:39-43.
|
http://doi.org/10.31288/oftalmolzh201923943 Received: 21 January 2019; Published-online: 24 April 2019 Axial length and refraction errors in premature infants with and without retinopathy of prematurity S.V. Katsan, Cand. Sc. (Med.); A.A. Adakhovskaia, MD SI “The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine”; Odessa (Ukraine) E-mail: adakhovskayaa@gmail.com TO CITE THIS ARTICLE: Katsan SV, Adakhovskaia AA. Axial length and refraction errors in premature infants with and without retinopathy of prematurity. J.ophthalmol.(Ukraine).2019;2:39-43. http://doi.org/10.31288/oftalmolzh201923943 Background. Preterm children, to a greater extent, can be affected by myopia in infancy and early childhood. Refractive errors can be related to the irregular growth of the eye. Purpose. To assess the incidence of refractive errors in groups of premature infants, aged 1 to 3 years, without ROP, with regressed ROP, and ROP treated with laser photocoagulation (LP). Material and Methods. Ophthalmological examination findings of 175 premature infants were studied. At the age of 4-5 weeks, the children were examined for ROP. Within the period between 6 months and 3 years, the children underwent standard ophthalmological examination and ultrasound diagnosis through closed eyelids. The findings were analyzed in three groups based on the main diagnoses: group 1, children without ROP; group 2, children with spontaneously regressed ROP; group 3, children with ROP, treated with retinal laser photocoagulation of avascular zones. MedCalc v.17.4 (MedCalc Software bvba, 1993-2017) was used to statistically process the data. Results. In 111 children (63%) of group 1, axial length (AL) of the right and left eyes was 19.3±1.1 mm and 19.4±1.1 mm, respectively. Hyperopia was noted in the right eye in 104 children (93.7%) and in the left eye in 105 children (94.6%). In 42 children (24%) of group 2, AL was 19.2±1.2 mm and 19.2±1.3 mm in the right and left eyes, respectively. Hyperopia was noted in the right eyes in 39 children (92.9%) and in the left eye in 37 children (88.1%). In 22 children (13%) of group 3, AL of the right and left eyes was 18.6±1.1 mm and 18.8±1.2 мм, respectively. Myopia was noted in the right eye in 6 children (27.3%) and in the left eye 3 children (13.6%); hyperopia was noted in the right eye in 11 children (50%) and in the left eye in 12 children (54.6%); emmetropia was in the right eye in 1 child (4.5%) and in the left eye in 2 children (9,1%); and astigmatism was in the right eyes in 4 children (18.2%) and in the left eye in 5children (22.7%). Conclusions. It was found that axial length in preterm children at the age of 1-3 years with a history of LP for ROP was smaller than that in children without ROP and with regressed ROP (18.7 mm versus 19.35 mm and 19.2 mm, respectively). The incidence rates of myopia (20.45%) and astigmatism (20.45%) were higher in preterm children with LP-treated ROP as compared to children without ROP (4.95% and 2.7%, respectively) and with regressed ROP (8.3% and 1.2%, respectively). Keywords: axial length, retinopathy of prematurity
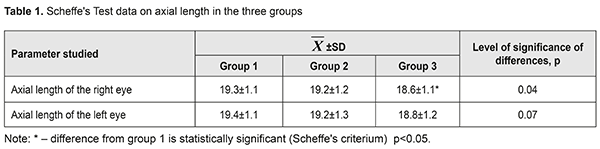
Background Retinopathy of prematurity (ROP) is one of the leading causes of bilateral blindness and visual impairment in premature infants in the world (CRYO-ROP trial 1990), which is not always related to previous disease-associated alterations [3]. Patients with favorable treatment outcome are also at high risk of ophthalmic pathology. Among eye diseases, myopia has a special place [9]. The Multicenter Study of the Early Treatment for Retinopathy of Prematurity (ETROP) has shown that 60% of patients, who had undergone early laser photocoagulation, developed visual acuity worse than 20/40 and 29% of patients had unfavorable outcomes (visual acuity worse than 20/200) [10]. Premature infants, to a greater extent, can be affected by myopia in early infancy and early childhood, opposite to full-term newborns, for whom hypermetropic refraction is common. In 1992, Quinn and colleagues showed that, in 20 % of premature infants with birth weights of less than 1251 g and with a self-regressing form of ROP, myopia developed within the first two years of life; high myopia (> 5.0 D) was observed in 4.6% [16]. It is crucial to understand the mechanism of refractive error development and progression in premature infants with ROP for searching for new treatment approaches and consulting parents on the further course of the disease. Today, researchers associate myopia with prematurity, ROP, and laser photocoagulation sequelae [6, 18]. However, the major cause of development and progression of a refractive error is still unclear [3, 15]. Therefore, to determine the cause of myopia it is necessary to identify the changes in a biometric profile of premature infants’ eyes in early infancy and early childhood. The purpose of the present paper was to assess the incidence of refractive errors in groups of premature infants, aged 1 to 3 years, without ROP, with self-regressive ROP, and ROP treated with laser photocoagulation (LP). Material and Methods Ophthalmological examination findings of 175 premature infants were studied. The study was carried out on the basis of Policlinic of SI “The Filatov Institute of Eye Diseases and Tissue Therapy”. Over stipulated time periods, all infants were examined for ROP at Department of Prematurity Pathology and Department of Neonatal Reanimation and Intensive Therapy. The stage and severity of ROP, if occurred, was classified according to the International Classification of ROP (ICROP, 2005) [11]. The infants with scarring Stages 4 and 5 were excluded from the study. Within the period between 6 months and 3 years, the children underwent standard ophthalmological examination which included physical examination, visual acuity testing, tests for strabismus, assessment of eyeball movements and convergence, wet retinoscopy for clinical refraction (double instillations of 0.5% cyclopentolate), ultrasound scanning, fundus ophthalmoscopy, and ultrasound biometry. Axial length (AL) was measured during the outpatient examination. The findings were analyzed in three groups based on the main diagnose: group 1, children without ROP; group 2, children with spontaneously regressed ROP; group 3, children with ROP, treated with retinal laser photocoagulation of avascular zones. MedCalc v.17.4 (MedCalc Software bvba, 1993-2017) was used to statistically process the data [1,13]. In analysis of qualitative attributes, the results are given as percentage values and their standard errors (±m%). Scheffe's Test for multiple comparisons was used to reveal statistical differences between means in normally distributed data. Results Based on ophthalmic examination, 175 children were divided as follows: group 1, 111 children (63%) without ROP; group 2, 42 children (24%) with simultaneously regressed ROP; and group 3, 22 children (13%) with ROP treated with LP. At the first study phase, we measured AL in the premature infants, aged 6 months to 3 years, in the three groups. A statistically significant difference was revealed in the AL values in group 3 compared to values in groups 1 and 2 (p=0.04). Table 1 demonstrates Scheffe's test data on the AL values. The mean value and 95% CI are given for right and left eyes.
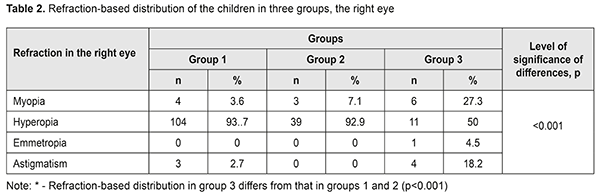
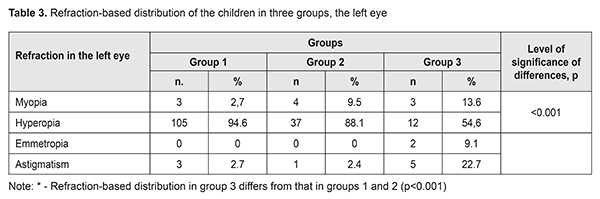
At the second study phase, we distributed the children according to diagnosis in the right and left eyes in the three groups. Tables 2 and 3 demonstrate that refraction-based distribution in group 3 statistically significantly differed from that in groups 1 and 2 (p<0.001).
Table 2 demonstrates that, in the right eye, hyperopia was diagnosed in 93.7% and 92.9% of the infants in groups 1 and 2, respectively, while, in group 3, hyperopia was found in 50% while 27.3% and 18.2% of the infants had myopia and astigmatism, respectively. Table 3 shows that, in the left eye, hyperopia was diagnosed in 94.6% and 88.1% of the children in groups 1 and 2, respectively, while, in group 3, hyperopia was found in 54.6% while 13.6% and 22.7% of the children had myopia and astigmatism, respectively. Discussion Our paper was a study of a biometric parameter, in particular, axial length of premature infants without ROP, with regressed ROP, ROP treated by laser photocoagulation. It does not provide proof but shows the mean axial length. It is a well-known fact that preterm children have higher rates of myopia as early as in early childhood; and this is, in a greater extend, true for children with a history of laser treatment for retinopathy of prematurity [3, 15]. Since “the third epidemic” has been declared in developing countries, including Ukraine, it is expected that the incidence of refractive errors, and, first of all, myopia, will increase in children [9]. In this regards, early diagnosis of refraction errors is an important predictor to avoid refractive amblyopia which can develop in these patients [18]. During the first 3-12 months of life, an eye is in the process of achieving emmetropia [19]. Thus, by the age of 1 year, there can be certain changes in the anatomical ocular structures. It is known that major causes of myopia in children are long axial length of the eye, shallower anterior chamber, and thicker lenses [14, 5]. However, which of those is more influential in myopia development in preterm babies is still unclear. Various hypotheses have been suggested. Congenital myopia has been associated with an abnormal diameter of the cornea and steep curvature, shallow anterior chamber, higher axial length, and thicker lens (Fledelius 1976; Gordon & Donzis 1986; Quinn et al., 1992). Thereafter, new evidence on the anatomical features of ocular tissues in the premature infants has come to light telling that such children are characterized by the convex cornea, deeper anterior chamber, thicker lens, and shorter axial length. These anatomical features are associated with irregular growth [4, 7, 8, 17]. In our study we assessed only axial length of the eye since this diagnostic procedure is performed to children aged 6 months to 3 years through closed eyelids. According to the data obtained, AL in premature infants with a history of LP for ROP was smaller than that in children without ROP and with regressed ROP (p=0.04). The rates of refractive errors in the children with a history of LP for ROP significantly differed from those in groups 1 and 2. It should be noted that this regularity was noted in early infancy and early childhood. In this cohort, the myopia and astigmatism rates were 20.45% and 20.45%, respectively. The issue what exactly determines the refractive abnormality in preterm patients with ROP still is a subject of discussion [2, 3, 20]. We endorse a view that laser treatment over the whole circumference of the retina (360°) possibly hampers ocular growth, and, consequently, results in a shorter AL even in the presence of myopia [12]. In addition, there is stunted growth of the posterior eye and active growth of the anterior eye. Chang-Sue Yang et al. performed a prospective, cross-sectional study on ocular structures in preterm children at the age of 9 years. They found some structural peculiarities including thicker lens (3.94 versus 3.39 mm in full-term children) and shallower anterior chamber depth (2.91 versus 3.58 mm). Also, the authors demonstrated that the eyes with laser-treated ROP had greater vertical corneal radius (7.67 versus 7.47 mm), smaller vertical corneal radius and the mean corneal curvature was steeper in eyes with laser-treated ROP when compared to full-term controls. (7.73 versus 7.76 mm). However, no difference in terms of axial length between the two groups was noted (23.32 versus 23.24 mm) [3]. We carried out, for the first time, the analysis of axial length in premature children at the age of 1 to 3 years. The analysis data showed the difference in axial length between children without ROP, regressed ROP, and LP-treated ROP ((18.7 mm versus 19.35 mm versus 19.2 mm, respectively). These findings can give evidence of importance of a refractive component and, consequently, development of refractive myopia and astigmatism. That is why it is required to perform a major and detailed study of all anatomical ocular structures in early and late childhood. In conclusion, firstly, it was found that axial length in preterm children at age of 1-3 years with a history of LP for ROP was smaller than that in children without ROP and with regressed ROP (18.7 mm versus 19.35 mm and 19.2 mm, respectively). Secondly, the incidence rates of myopia (20.45%) and astigmatism (20.45%) were higher in preterm children with LP-treated ROP as compared to children without ROP (4.95% and 2.7%, respectively) and with regressed ROP (8.3% and 1.2%, respectively). References 1.Lyakh YuE, Guryanov VG, Khomenko VN, Panchenko OA. [Basics of Computer Biostatistics. Data Analysis in biology, medicine and pharmacy statistical using statistical software Med Stat]. Donetsk: Papakitsa EK; 2006. 214p. Russian 2.Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74:35-9. 3.Chang-Su e Yang, An-Guor Wang, Yung-Feng Shih, Wen-Ming Hsu Long-term biometric optic components of diode lasertreated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmologica. 2013; 91: 276 - 82. 4.Chen TC, Tsai TH, Shih YF, Yeh PT, Yang CH, Hu FC. Long–term Evaluation of Refractive Status and Optical Components in Eyes of Children Born Prematurely. Invest Ophthalmol Vis Sci – 2010;12(51):6140-8. 5.Choi MY, Park IK, Yu YS. Long term refractive outcome ineyes of preterm infants with and without retinopathy of prematurity: comparison of keratometric value, axial length, anterior chamber depth, and lens thicknes. Br J Ophthalmol. 2000;2(84):138-43. 6.Connolly BP, Ng EY, McNamara JA, Regillo CD, Vander JF, Tasman W. A comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years: Part 2. Refractive outcome. Ophthalmology.2002;109:936-41. 7.Cook A, White S, Batterbury M, Clark D. Ocular growth and refractive error development in premature infants with or without retinopathy of prematurity. Invest Ophthalmol Vis Sci. 2008;12(49): 5199-207. 8.Cosgrave E, Scott C, Goble R. Ocular findings in low birthweight and premature babies in the first year: Do we need to screen? Eur J Ophthalmol. 2008;1(18):104-11. 9.Davitt BV, Dobson V, Good WV, Hardy RJ, Quinn GE, Siatkowski RM. Prevalence of myopia at 9 months in infants with high-risk prethreshold retinopathy of prematurity. Ophthalmology. 2005;112:1564-8. 10.Good WV, Hardy RJ, Dobson V. Final visual acuity results in the early treatment for retinopathy of prematurity study. Arch. Ophthalmol. 2010;6(128):663-71. 11.ICROP Committee for Classification of Late Stages ROP. An international classification of retinopathy of prematurity, II: the classification of retinal detachment. Arch Ophthalmol. 1987;105: 906-12. 12.Iwase S, Kaneko H, Fujioka C, Sugimoto K, Kondo M, Takai Y. A long-term follow-up of patients with retinopathy of prematurity treated with photocoagulation and cryotherapy. Nagoya J Med Sci. 2014;76:121-8. 13.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. 14.Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48: 2510−1219. 15.Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B. Progression of myopia and high myopia in the early treatment for retinopathy of prematurity study: Findings at 4 to 6 years of age. J AAPOS. 2013;17:124-8. 16.Quinn GE, Dobson V, Repka MX. Development of myopia in infants with birth weights less than 1251 grams. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology. 1992;3(99):329-40. 17.Saunders KJ, McCulloch DL, Shepherd AJ, Wilkinson AG. Emmetropisation following preterm birth. Br J Ophthalmol. 2002; 9(86):1035−40. 18.Savleen K, Jaspreet S, Deeksha K, Mansi S, Ramanuj S, Mangat RD. Refractive and ocular biometric profile of children with a history of laser treatment for retinopathy of prematurity Indian. J Ophthalmol.2017:9(65):835–40. 19.Troilo D, Wallman J. The regulation of eye gowth and refractive state: an experimental study of emmetropization. Vision Res. 1991;7-8(31):1237−50. 20.Ziylan S, Serin D, Karslioglu S. Myopia in preterm children at 12 to 24 months of age. J Pediatr Ophthalmol Strabismus. 2006;43:152–6.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.Received: 21 January 2019; Published: 24 April 2019
|