J.ophthalmol.(Ukraine).2018;6:10-18.
|
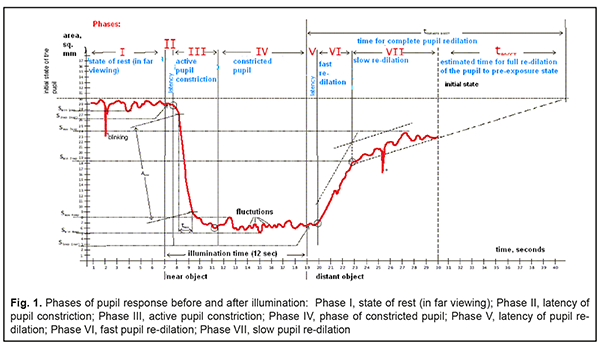
http://doi.org/10.31288/oftalmolzh201861018 Received: 23 August 2018; Published on-line: 21 September 2018 Outcomes of medical treatment for accommodative impairments, with a consideration of the balance of autonomic innervation and pupillography data Dukhayer Shakir, MD; N.M. Bushuieva, Dr Sc (Med); S.B. Slobodianyk, Cand Sc (Med) Received: 23 August 2018 Published: 21 September 2018 Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine; Odessa (Ukraine) E-mail: shakirdukhayer@gmail.com TO CITE THIS ARTICLE: Dukhayer Shakir, Bushuieva NM, Slobodianyk SB. Outcomes of medical treatment for accommodative impairments, with a consideration of the balance of autonomic innervation and pupillography data. J.ophthalmol.(Ukraine).2018;6:10-18.http://doi.org/10.31288/oftalmolzh201861018 Background: The relationships of characteristics of accommodation-and-convergence pupil response with age and balance between sympathetic and parasympathetic innervation (or eutony) in healthy children and adolescents are complex and ambiguous. The results of this study were needed to select a treatment for accommodative impairments. Purpose: To investigate the efficacy of instillation of mydriatic eye drops in patients with impaired accommodation, with a consideration of both the balance of autonomic innervation and pupillography data. Materials and Methods: Seventy-one children and adolescents (age, 5 to 16 years) with impaired accommodation were treated with 1% cyclopentolate and/or 2.5% phenylephrine. The examinations included measurements of uncorrected and best-corrected visual acuity for near and distance, accommodation reserve (by the technique of Dashevsky) and autorefractometry. In addition, autonomic nervous system balance was assessed using Kerdo index (KI). Pupil responses were recorded using an OK-2 pupillographer (Ukraine). Results and Conclusion: The maximum mydriatic effect and cycloplegia were achieved within 1-2 hours after the application of 1% cyclopentolate, leading to a decrease in myopia and detection of hyperopic refractive errors, which justifies the effective use of this agent for diagnosing accommodative spasm. Using pupillography, we found that the mydriatic effect of 2.5% phenylephrine was less apparent than that of 1% cyclopentolate. Efficacy of 1% cyclopentolate and 2.5% phenylephrine was significantly higher in individuals with an increased parasympathetic tone of the ANS. We developed a combination regimen to treat accommodative impairments, with the bedtime administration of 2.5% phenylephrine (1 drop) and 1% cyclopentolate (1 drop) in both eyes (4 days on for the former only, 1 day on for the latter only, and 2 days off for both) for a month. Treatment with the combination regimen resulted in improvements in visual acuity and accommodative reserve in all patients. The regimen was well tolerated by patients, and no allergic or toxic effects were noted. Keywords: accommodative impairments, pupillography, 2.5% phenylephrine, 1% cyclopentolate, autonomic nervous system tone Introduction The relationships of characteristics of the accommodation-and-convergence pupil response with age and balance between sympathetic and parasympathetic innervation (or eutony) in healthy children and adolescents are complex and ambiguous. Impaired accommodated function (accommodative spasm or palsy) is manifested by visual fatigue and near and distant vision abnormalities and may herald the onset of myopia, in the development of which a weakened accommodation, according the theory of Avetisov, Dashevsky and others [1-5], plays a major role. Various mydriatics (atropine, tropicamide, mydriacyl, and mesaton) relax the ciliary muscle and cause a paresis of accommodation, and have been extensively used in the diagnosis and treatment of impaired accommodation in recent years [6]. Mydriatic agents are usually administered with a disregard of the state of autonomic innervation balance. As mydriatics directly influence the autonomic nervous system (sympathetic and/or parasympathetic), they, however, can produce undesirable effects, if administered with a disregard of the state of autonomic innervation balance. Thus, cases of a failure to restore the accommodation reserve, with a decline in visual acuity, after long-term (7-10 days) pharmacological mydriasis have been reported [6, 7-12]. Therefore, a differential approach to selection and administration of an appropriate mydriatic should involve consideration of (1) the state of autonomic innervation balance in patients with impaired accommodation and (2) potential changes in this state after administration of various mydriatics. The purpose of the study was to investigate the efficacy of instillation of mydriatic eye drops in patients with impaired accommodation, with a consideration of the balance of autonomic innervation and pupillography data. Material and Methods Seventy one patients (age, 5 years to 16 years) with impaired accommodation (a decreased accommodation reserve (AR) of 0 to -2 D) were under observation. Two mydriatics differing in their mechanism of action, either alone or in combination with each other were used to perform diagnostics and treatment. Cyclomed 1% is the cyclopentolate hydrochloride preparation that blocks the responses of the iris sphincter muscle and accommodative ciliary muscle to cholinergic stimulation producing pupillary dilation (due to an increased tone of the iris dilator muscle and relaxation of the sphincter muscle) and ciliary muscle relaxation leading to cycloplegia. Irifrin 2.5% is the phenylephrine hydrochloride preparation that stimulates postsynaptic alpha adrenoceptors and causes the contraction of the iris dilator muscle and smooth muscles of conjunctival arterioles; the agent has no effect on the ciliary muscle, and the induced mydriasis is not accompanied by cycloplegia. Of the 71 followed-up patients, 26, 30 and 15 were treated with cyclopentolate only, phenylephrine only, and a combination of cyclopentolate and phenylephrine, respectively. The examinations for each eye included measurements of uncorrected and best-corrected visual acuity for near and distance, accommodation reserve (by the technique of Dashevsky) and autorefractometry. In addition, autonomic nervous system balance was assessed using Kerdo index (KI) [6]: KI = 1 – D/P, where D is diastolic blood pressure and P is cardiac frequency (or heart rate, beats/min). KI equals zero in normal autonomic nervous system tone, is negative in individuals with an increased parasympathetic tone, and positive in those with an increased sympathetic tone of the autonomic nervous system. Pupil responses were recorded using an OK-2 pupillographer (Ukraine) [8-9]. Pupil flash response curves were recorded and included seven phases of changes in pupil area before and after presentation of a light stimulus (Fig. 1).
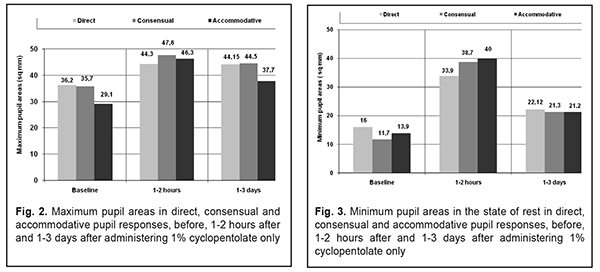
The following pupillography indices were subjected to analysis: maximum and minimum pupil areas in direct, consensual and accommodative pupil responses before and after administering mydriatic eye drops; phase II of pupil response, or pupil constriction latency, which reflects the parasympathetic pupil response; and phase V of pupil response, or pupil re-dilation latency, which reflects the sympathetic pupil response. Results Twenty six patients with a decreased AR of 0 to -2D were followed after treatment with cyclopentolate only. Of these, 9 exhibited emmetropia, 10 exhibited myopia of -0.5 D to -0.75 D, and 7 had myopia of up to -3.0 D at baseline. Thirty minutes after administration of cyclopentolate only, 4 patients with baseline mild myopia were found to have mild hyperopia, 7 exhibited a reduction in myopia by 1.0 D, and 13 exhibited emmetropia. Under full cycloplegia with cyclopentolate only, 10 patients showed improvements in visual acuity by 0.1, three by 0.25 and 7 by 0.4 (from 0.6 at baseline to 1.0). All these patients had an increased parasympathetic autonomic nervous system tone (KI < 0). The visual acuity, however, did not change in 6 patients with an increased sympathetic autonomic nervous system tone (KI > 10). Of the cyclopentolate-only-treated patients with an increased parasympathetic ANS tone, 8 (16 eyes) were followed for changes in pupil response. Fig. 2 presents maximum pupil areas in the state of rest in direct, consensual and accommodative pupil responses to gaze shift at 10 cm, before, 1-2 hours after and 1-3 days after administering cyclopentolate only. One to three days after administering cyclopentolate only, maximum pupil areas in direct, consensual and accommodative pupil responses increased compared to baseline.
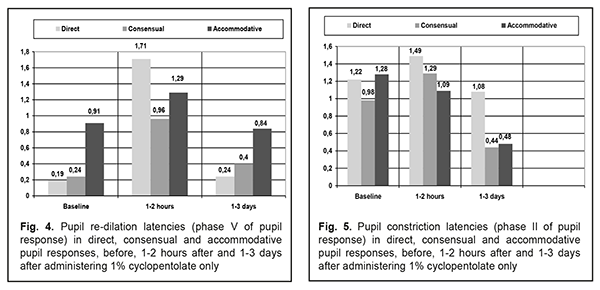
Fig. 3 presents minimum pupil areas in the state of rest in direct, consensual and accommodative pupil responses, before, 1-2 hours after and 1-3 days after administering cyclopentolate only. One to two hours after administering cyclopentolate only, minimum pupil areas in direct, consensual and accommodative pupil responses increased compared to baseline; one to three days after administering cyclopentolate only, they somewhat decreased but were still higher than at baseline. We also examined changes in pupil re-dilation latency (phase V of pupil response) and pupil constriction latency (phase II of pupil response) after administering cyclopentolate only. Pupil re-dilation latencies in a direct pupil response at baseline was 1.28 s, increased to 1.49 s one to two hours, and decreased almost to baseline (1.08 s) by day 1-3 after administering cyclopentolate only. At days 1-3 after administering cyclopentolate only, pupil re-dilation latencies in consensual and accommodative pupil responses decreased more than twofold (to 0.98 s and 1.28 s, respectively) compared to baseline values (0.44 s and 0.45 s, respectively) (Fig. 4).
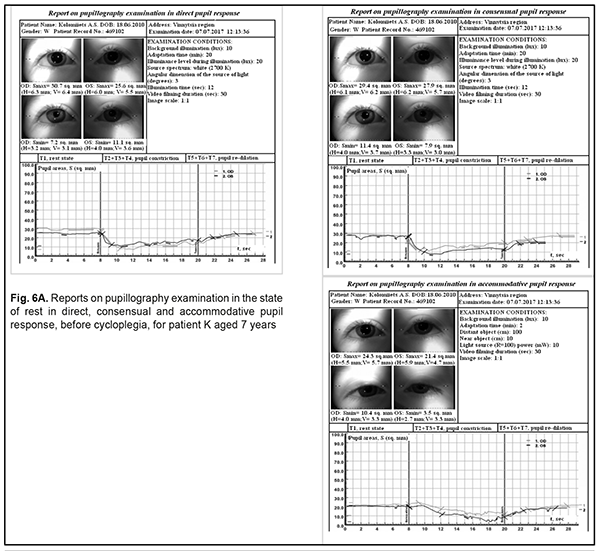
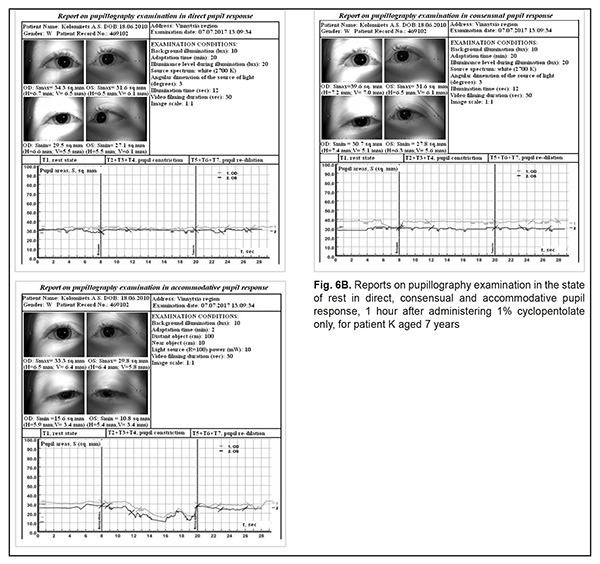
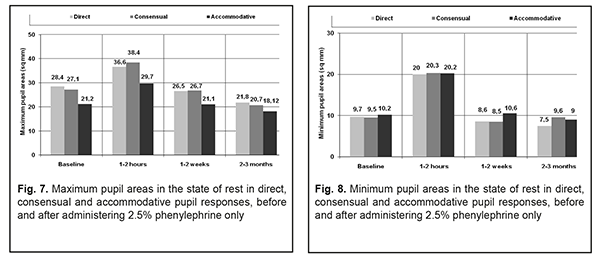
Pupil constriction latencies (phase II of pupil response) in direct, consensual and accommodative pupil responses markedly increased compared to baseline 1-2 hours after administering cyclopentolate only (with the greatest, almost ten-fold, increase from 0.18 s to 1.71 s observed in a direct pupil response), and decreased almost to baseline by day 1-3 after administering cyclopentolate only (Fig. 5). Therefore, cyclopentolate was found to be effective for mydriasis for diagnostic and treatment purposes in the presence of increased parasympathetic autonomic nervous system tone in children and adolescents with impaired accommodation. Using pupillography, we found that the mydriatic and cycloplegic effect of cyclopentolate persisted for 1-3 days. The data obtained justify the regimen being used in the clinical practice of pediatric ophthalmology for impaired accommodation, with one drop of 1% cyclopentolate instilled in both eyes at bed time for a month, which leads to elimination of asthenopic complaints, stable improvement in vision, and increase in the amount of AR. Assessing baseline autonomic nervous system tone before treatment would enable a more differential approach to cyclopentolate administration. Example case: patient K, aged 7 years; Patient Record No. 469102. Baseline complaints: Visual fatigue and headache Baseline uncorrected visual acuity (UCVA): OU 1.0 Baseline accommodative reserve: 0 D Refraction: Emmetropic Kerdo index: <0 (i.e., increased parasympathetic autonomic nervous system tone) One hour after instillation of a single drop of 1% cyclopentolate, in the presence of cycloplegia, the UCVA in both eyes improved to 1.2, and the refraction changed to hypermetropia of +0.75 D. The reports of pupillography examination in the state of rest in direct, consensual and accommodative pupil response, before cyclopegia and 1 hour after administering 1% cyclopentolate only are presented in Figs. 6A and 6B, respectively. Thirty patients with a decreased AR of 0.5 to 2.0 D were followed after treatment with phenylephrine hydrochloride only. Initially, all of them exhibited mild myopia of -0.5 D to -2.5 D. Thirty minutes to one hour after administration of phenylephrine hydrochloride only, 2 patients with baseline mild myopia were found to have emmetropia, and 28 exhibited a reduction in myopia by 0.5 D to 1.0 D. Twenty five patients had an increased parasympathetic ANS tone (KI < 0), and 5, an increased sympathetic ANS tone (KI > 0). All of these were treated with one drop of 2.5% phenylephrine instilled in both eyes at bed time for a month for impaired accommodation. The treatment led to improvements in visual acuity by 0.1 to 0.2, with reduced visual fatigue. In addition, accommodation reserve increased by 0.5 D to 1.0 D in the 25 patients that had an increased parasympathetic ANS tone at baseline, and did not change from baseline of 0 D in the 5 patients that had an increased sympathetic ANS tone. Pupillographic records of 15 patients (30 eyes) with an increased parasympathetic ANS tone treated with phenylephrine only were subjected to analysis. Minimum and maximum pupil areas increased at 1 to 2 hours, and decreased to baseline levels at 1-2 weeks after administering phenylephrine only (Figs. 6 and 7). There was nearly no pupil responses at 2-3 months after administering phenylephrine only. Therefore, it can be stated that the effect of phenylephrine lasts for 1-2 weeks at least.
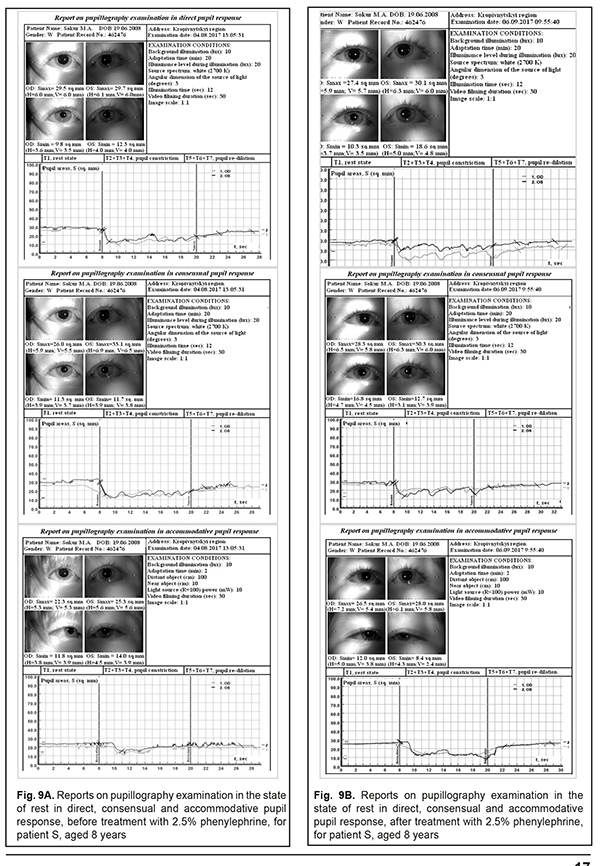
Example case: patient C, aged 8 years, Patient Record No. 462476 Baseline UCVA: OU 0.35 Baseline BCVA: OU 1.0 Refraction: OU -1.0 D Sph Kerdo index: -10.0 After treatment with one drop of 2.5% phenylephrine instilled in both eyes at bed time for a month for impaired accommodation, UCVA in both eyes improved to 1.0. The reports of pupillography examination in direct, consensual and accommodative pupil response, before (Fig. 9A) and 1 month after (Fig. 9B) administering 2.5% phenylephrine only are presented below.
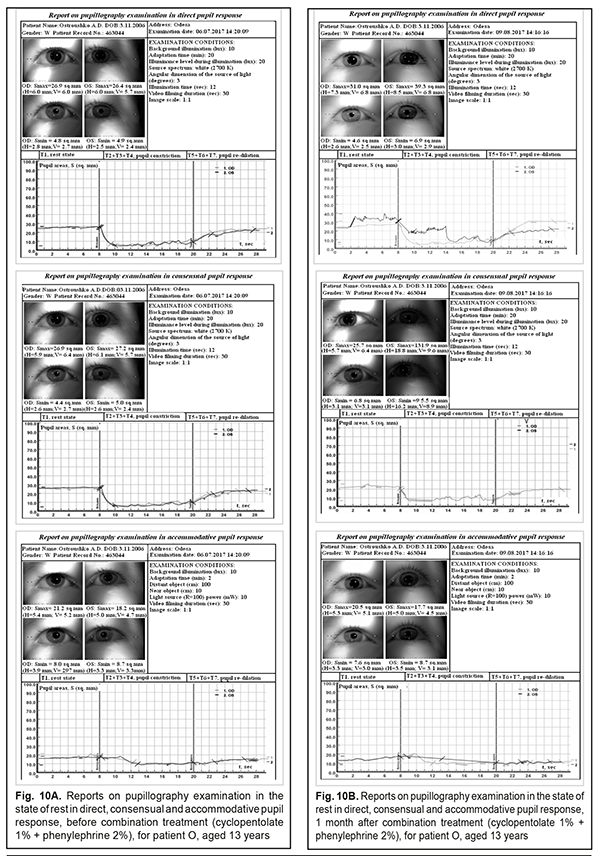
Based on these findings, we developed a combination regimen to treat accommodative impairments, with the bedtime administration of 2.5% phenylephrine (1 drop) and 1% cyclopentolate (1 drop) in both eyes (4 days on for the former only, 1 day on for the latter only, and 2 days off for both) for a month. In this treatment regimen, the two mydriatics differing in their mechanism of action simultaneously exert their effects on the sympathetic and parasympathetic autonomic innervation of various ciliary muscle groups and iris muscle groups, contributing to improvements in visual functions, and, apparently, to the restoration of a local autonomic nervous system balance. The combination treatment regimen for accommodative impairments in children and adolescents was well tolerated by patients, and no allergic or toxic effects were noted. The outcomes of treatment of 10 patients with accommodative impairments (AR < 1.0 D) and an increased baseline parasympathetic ANS tone (KI < 0) using the combination treatment regimen were subjected to analysis. Uncorrected visual acuity improved from baseline values of 0.6-0.8 to 1.0 in 6 patients, and improved from baseline values of 0.4-0.5 to 0.6 in 9 patients, and the amount of accommodation reserve increased to 2.5 D-3.0 D. Example case: Patient O, aged 13 years, Patient Record No. 469043 Baseline UCVA: OU 0.4 Baseline BCVA: OU 1.0 Refraction: OU -1.0 D Sph Baseline AR= 0 D KI= -10 (parasympathotonia) The patient was administered 2.5% phenylephrine, 1 drop in both eyes at bed time (with a dosing schedule of four days on, two days off), and 1% cyclopentolate, 1 drop in both eyes at bed time (with a dosing schedule of one day on, two days off) for a month. After treatment, UCVA improved to 1.0, and AR improved to 2.0 D. The reports of pupillography examination before (Fig. 10A) and after treatment (Fig. 10B) are presented below.
Conclusion The maximum mydriatic effect and cycloplegia were achieved within 1-2 hours after the application of 1% cyclopentolate, leading to a decrease in myopia and detection of hyperopic refractive errors, which justifies the effective use of this agent for diagnosing accommodative spasm. Using pupillography, we found that the mydriatic effect of 2.5% phenylephrine was less apparent than that of 1% cyclopentolate. Efficacy of 1% cyclopentolate and 2.5% phenylephrine was higher in individuals with an increased parasympathetic tone of the ANS. We developed a combination regimen to treat accommodative impairments, with 1 drop of 2.5% phenylephrine instilled in both eyes at bed time (with a dosing schedule of four days on, two days off), and 1 drop of 1% cyclopentolate instilled in both eyes at bed time (with a dosing schedule of one day on, two days off) for a month. Treatment with the combination regimen resulted in improvements in visual acuity and accommodative reserve in all patients. The regimen was well tolerated by patients, and no allergic or toxic effects were noted.
References 1.Avetisov ES. [Myopia]. Moscow: Meditsina; 1986. Russian. 2.Vein AM, editor. [Accommodation: A guide for physicians]. Moscow: Meditsinskoe informatsionnoe agenstvo; 1998. p. 336-54. Russian. 3.Dashevsky AI. [Pseudomyopia]. Moscow: Meditsina; 1973. p. 5-37. Russian. 4.Ponomarchuk VS, Terletska OIu. [Novel advanced method of electric phosphene puncture for the treatment of accommodative dysfunction]. Odesa: Astroprint; 2018. Russian. 5.Mutti DO, Mitchell GL, Hayes JR, et al. The Response AC/A Ratio Before and After the Onset of Myopia. Invest Ophthalmol Vis Sci. 2017 Mar 1;58(3):1594-1602. 6.Katargina LA, editor. [Accommodation: A guide for physicians]. Moscow: Aprel; 2012. Russian. 7.Bushuieva NM, Dukhayer Shakir, Kul’bida MP, Slobodjanik SB. [Pupil responses in healthy children and adolescents with a consideration of the balance of autonomic innervation to the eye]. Oftalmologiia. Vostochnaia Evropa. 2017;7(4):524-31. Russian. 8.Bushuieva NM, Ushan OV, Dukhayer Shakir. [Method for diagnosing accommodative and pupillary dysfunction]. Information Bulletin No. 4, Declar. Pat. of Ukraine №6,231 A61F 9/00 issued 15.04.2005. Ukrainian. 9.Bushuieva NM, Boychuk IM, Dukhayer Shakir, Khramenko NI, Ponomarchuk VS. [Method of computer pupillography]. Ukrainskyi medychnyi almanakh. 2006;9(2):24-7. Ukrainian. 10.Bushuieva NM, Dukhayer Shakir. [Indications for 1% cyclomed and 2.5% irifrin in patients with accommodative impairments]. In: [Proceedings of the 7th Pediatric Ophthalmology Conference]. Kyiv. June 14-15, 2018. p. 52-3. Russian. 11.Bushuieva NM, Dukhayer Shakir. [Regimen of treatment of accommodative impairments with 1% cyclomed and 2.5% irifrin]. In: [Proceedings of the Conference of Ophthalmologists from Chernivtsi, Ivano-Frankivsk, Ternopil and Khmelnytskyi oblasts of Ukraine]. Chernivtsi. 2017. p. 77-9. Ukrainian. 12.Dukhayer Shakir, Bushuieva NM. [Outcomes of treatment of accommodative impairments with 1% cyclomed and 2.5% irifrin]. In: [Proceedings of the 14th Ukrainian Ophthalmology Congress]. Odesa. June 23-25, 2018. p. 240-1. Ukrainian.
|