J.ophthalmol.(Ukraine).2018;2:56-59.
|
https://doi.org/10.31288/oftalmolzh/2018/2/5659 A case of successful using a stromal corneal transplant for therapeutic keratoplasty in a patient with herpetic keratitis E. V. Sereda, a junior research fellow; G. I. Drozhzhyna, Dr. Sc. (Med.), Prof.; T. B. Gaidamaka, Dr. Sc. (Med.) SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”; Odessa (Ukraine) E-mail: evsereda08@gmail.com TO CITE THIS ARTICLE: Sereda EV, Drozhzhyna GI, Gaidamaka TB. A case of successful using a stromal corneal transplant for therapeutic keratoplasty in a patient with herpetic keratitis. J.ophthalmol.(Ukraine).2018;2:56-9. https://doi.org/10.31288/oftalmolzh/2018/2/5659
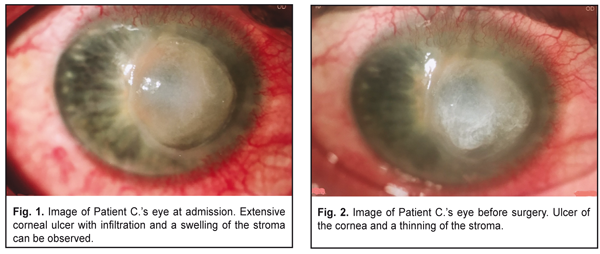
Introduction. Herpes virus infection is a cause of inflammatory corneal diseases in 20-57 % of cases. To date, due to the lack and high cost of donor material in Ukraine, approbation of new material for keratoplasty is of great relevance. Purpose. To report a case of successful using a stromal corneal transplant for therapeytic keratoplasty in a patient with herpitic keratitis. Material and Methods. Visual acuity testing, standard ophthalmic examination, microbiology study. Results. Using lyophilized stromal layers made it possible to prevent corneal perforation in a patient with herpetic keratitis. Early operative intervention made it possible to preserve visual function and to avoid severe complications. Conclusions. If urgent keratoplasty is required and keratobioimplant is not available/affordable, lyophilized stromal layers of the cornea with the Descemet's membrane can serve as an alternative material for therapeutic tectonic keratoplasty and can prevent development of severe keratitis complications including descemetocele, corneal perforation etc. Key-words: herpes, corneal ulcer, therapeutic keratoplasty, corneal stroma Herpes virus infection is a cause of inflammatory corneal diseases in 20-57 of cases. It is characterized by a persistent relapsing course and often leads to a longstanding temporary or permanent loss of ability to work [1]. According to data of World Health Organization, an overall percentage of herpetic keratitis in the structure of corneal blindness is 60%. Early treatment and, if required, surgery for herpetic keratitis largely determines the outcome of the disease. Lamellar keratoplasty has been proved to be the most optimal surgery for recurrent herpetic keratitis compared to penetrating keratoplasty [2, 3, 4].To date, due to the lack and high cost of donor material in Ukraine, there is a constant search for alternative material for keratoplasty, especially for therapeutic one. That is why, approbation of new material for keratoplasty is of great relevance. A clinical case as follows can serve an illustration of that. A 42 y/o patient S. referred to Corneal Pathology Department in the Filatov Institute on December 21, 2016, with complaints of tearing, photophobia, redness and visual acuity impairment in the right eye. According to patient’s words, he noted redness of the right eye three weeks earlier after supercooling during the construction work in the open air. On the following day, the patient referred to a local out-patient clinic where he was prescribed instillation of disinfecting and antibacterial drops. Due to the absence of positive changes and the appearance of pain syndrome in the right eye, the patient was referred to SI “Filatov Institute of Eye Diseases and Tissue Therapy of NAMS of Ukraine”. Slit-lamp biomicroscopy of the right eye revealed: combined conjunctival injection; vascularization of the corneal limbus and paralimbic areas within 12 to 16 o’clock; extensive corneal ulcer involving the optic zone; diffuse edema of the stroma; a zone of thinning in the lower part of ulceration; the anterior chamber of a moderate depth; miosis (Fig. 1). Fluorescence test was positive with a staining of the entire area of corneal ulceration. Visual acuity was equal to light perception with a correct light projection in the right eye and 1.0 in the left eye. Pneumotonometry showed intraocular pressure of 25.0 and 16.0 mmHg in the right and left eyes, respectively. The occurrence of hypertension in the right eye was confirmed by a palpatory method.
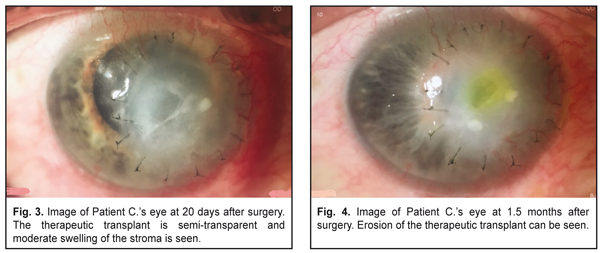
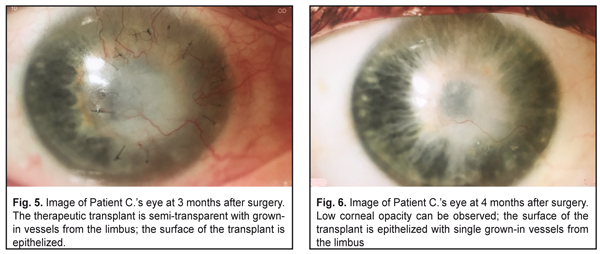
The patient was diagnosed metaherpetic keratitis with hypertension and corneal ulcer with stromal thinning. A course of conservative therapy included: instillations of disinfecting, antiviral, hypotensive, non-conservative, tear- substituent drops as well as mydriatics and dexpanthenol; parabulbar heparin sodium, dexamethasone, gentamicin injections; intramuscular injections of meloxicam, interferon; intravenous calcium gluconate, ascorbic acid, dimedrol, dexamethasone injections; oral administration of valaciclovir and hepatoprotectors. Microbiological study of the conjunctival discharge from both eyes revealed no pathological microflora. During the first five days we observed in the right eye a corneal thinning in the site of ulceration; therefore, the patient was proposed therapeutic and tectonic keratoplasty in order to prevent corneal perforation (Fig. 2). On December 27, 2016, the patient (the right eye) underwent therapeutic and tectonic lamellar keratoplasty d=8.0/7.0 mm using a lyophilized stromal corneal transplant. In surgery, we used deep stromal lamellae of keratobioimplant with the Descemet's membrane left after previous lamellar keratoplasty and were lyophilized. After cleansing the surface of the cornea and forming a layered bed, the therapeutic graft was located with the Descemet's membrane to the wound surface and the stromal side to the top. The graft was secured using interrupted 10/00 nylon sutures. In the postoperative period, the surface of the graft was doughy with a moderate swelling. Microbiology study revealed no bacterial and fungal flora in the conjunctival cavities in both eyes, which made it possible to put a therapeutic soft contact lens (SCL) on the right eye in order to prevent lysis of the cells on the surface of the transplant. At discharge from the hospital (01 January, 2017), biomicroscopy of the right eye showed moderate conjunctival hyperemia on the nasal side; vascularization of the limbus and the cornea at 12-16 o’clock; correct position of the SCL; the semi-transparent therapeutic transplant was adapted by interrupted sutures; the anterior chamber of an average depth; mydriasis (Figure 3). IOP by palpation was in the norm against the antihypertensive drops. Visual acuity in the right eye was 0.01 eccentrically; visual acuity in the left eye was 1.0.
Reexamination was performed on 08 February 2017. Biomicroscopy of the right eye showed: a decrease in the vascularization of the limbus and the cornea; the therapeutic transplant was semi-transparent with erosion remained in the center; no suture failure; the anterior chamber of an average depth; a mobile pupil (Fig. 4). Visual acuity was 0.03 and 1.0 in the right and left eyes, respectively. It should be noted that at the moment of the follow-up examination the patient had no complaints except for poor visual acuity. The therapeutic SML was replaced as well as prescriptions and recommendations were given. At 3 months after surgery, biomicroscopy of the right eye showed: the semi-transparent transplant with the epithelized surface; vascularization of the limbus and the cornea (Fig. 5). Visual acuity of the right eye remained the same.
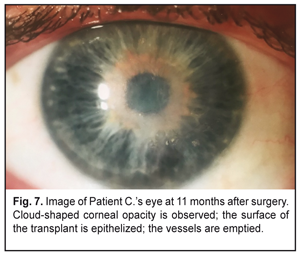
At 4 months after surgery (25 April 2017), the interrupted sutures were removed from the transplant due to suture loosening. At the discharge from the hospital (04 May, 2017), biomicroscopy of the right eye showed: a pink conjunctiva, uneven low opacity of the cornea; fluorescence test was negative; single limbal vessels grew into the transplant; the anterior chamber of an average depth; a mobile pupil (Fig. 6). IOP in the right eye was 18.0 mmHg. Visual acuity in the right eye was 0.1. At 11 months after surgery, biomicroscopy of the right eye showed a pale pink conjunctiva; an intact limbus; low corneal opacity; empty corneal vessels; and the surface of the transplant was epithelized (Fig. 7). Visual acuity in the right eye was 0.2.
Conclusions Viral herpetic keratitis with damage to deep layers of the stroma has a severe course and leads to formation of severe corneal opacities and development of a number of complications (descemetocele, corneal perforation etc.). The clinical case described demonstrates a successful effort to use lyophilized stromal layers to prevent corneal perforation. Timely operative intervention made it possible to preserve visual function and to avoid severe complications.
Thus, if urgent keratoplasty is required and keratobioimplant is not available/affordable, lyophilized stromal layers of the cornea with the Descemet's membrane can serve as an alternative material for therapeutic tectonic keratoplasty and can prevent development of severe keratitis complications including descemetocele, corneal perforation etc. Reference
|