Effect of microprismatic eyeglasses on the character of binocular vision in children with strabismic amblyopia over treatment time
S.O. Rykov,1 Dr Sc (Med)
V.B. Mellina,2 Pediatric Ophthalmologist
1Shupyk National Medical Academy of Postgraduate Education
2Eye Microsurgery Center, Kyiv City Clinical Ophthalmologic Hospital
E-mail: Mellina111@rambler.ru
Background: Strabismic children develop early motor and/or sensory complications (amblyopia, poor fixation of the eye, impaired fusion, and impaired binocular vision). The major goals of treatment for strabismic amblyopia are to remove strabismus, to improve the vision of the amblyopic eye, and to restore the binocular vision. Prisms and apparatus-based orthoptics techniques have been used for a long time for the treatment of impairments in binocular vision. In Ukraine, the technology for manufacture of spheroprismatic lenses designed as microprismatic combination eyeglasses was developed in 2009.
Purpose: To investigate the effect of microprismatic glasses versus apparatus-based pleoptics-and-orthoptics techniques on the character of binocular vision in children with strabismic amblyopia.
Materials and Methods: One hundred and forty nine children with strabismic amblyopia aged 4 to 18 years were included into the study. Concomitant esotropia and exotropia were found in 77 children and 11 children, respectively, of the study group, versus 54 children and 7 children, respectively, of the control group. Six children (6.8%) of the study group, versus 13 children (21.3%) of the control group were those with partially accommodative strabismus, whereas the rest were those with non-accommodative strabismus. Children of the study group were treated with microprismatic glasses, whereas those of the control group were treated with apparatus-based techniques.
Results: At 6 months, binocular single vision was obtained in 20 children (22.7%) of the study group versus only one child (3.0%) with low amblyopia of the control group. In addition, diplopia was present in 51 children (58.0%) of the study group versus 10 children (16.4%; 8 children (13.1%) at baseline) in the control group.
Conclusion: The treatment proposed for strabismic amblyopia (a) requires no additional time, (b) has good outcomes, (c) is suitable for patients, and (c) is more efficacious than conventional apparatus-based pleoptics-and-orthoptics therapy.
Key words: strabismic amblyopia, binocular character of vision, microprismatic glasses
Introduction
Amblyopia is reduced visual function in one or two eyes - without any evidence of organic eye disease - resulting from a limited sensory experience during the development of the visual system [1, 2]. The pathogenesis of strabismic amblyopia is closely associated with that of concomitant strabismus which is a binocular vision disorder [3, 4]. Strabismic children develop early motor complications (spasm, contracture, secondary strengthening and weakening of synergists and antagonists) and/or early sensory complications (amblyopia, poor fixation of the eye, impaired fusion, impaired binocular vision and abnormal retinal correspondence). These complications interact with each other, become chronic rapidly, and often manifest more apparently than the original pathogenic factors. It is the secondary complications that determine the clinical picture of strabismus after the age of 7 [1]. These complications are considered as a way of sensory adaptation for the compensation of the effect of image doubling in vision with two eyes. In most of patients with monocular strabismus, a functional scotoma results in a fall in visual acuity in the strabismic eye, in spite of the absence of changes in the fundus. Such a fall in visual acuity appears as amblyopia or strabismic amblyopia [5].
The key principles of the management of amblyopia are as follows: (a) the removal, if possible, of any obstacle to normal vision (repair of strabismus), (b) optimum correction of refractive defects, (c) measures for a complete integration of amblyopic eye into functioning or forced integration of this eye into functioning, with concomitant measures to limit the contribution of the eye with better vision into binocular vision [6]. According to Ding and Levi [7], in functional rehabilitation of patients with strabismus, the main purpose is to restore the binocular single vision which is based on the ability of a healthy visual system to integrate two monocular images into one binocular image. It has been reported that ophthalmologists managed to restore binocular single vision only in 40-45% of patients with strabismus [8, 9].
Most of the authors believe that continuity and sequence of pleoptic, orthoptic, diploptic and stereoptic techniques are the factor that substantially influences the efficacy of treatment [10-12]. Currently, various techniques (monochromic and color stimulation of the retina with static and dynamic patterns, retinal magnetic stimulation, retinal electric stimulation, synoptophore exercises, diploptics, etc.) are available for the treatment of any amblyopia. The availability of multiple treatment options for the disease is a reflection of the fact that none of them have emerged as a clearly superior choice for all patients [13]. The outcome of the treatment of strabismic amblyopia depends on the initial severity of the amblyopia and fixation of the amblyopic eye, which in their turn depend on the time at which the strabismus becomes manifest, and the time from disease onset until start of treatment.
As early as the nineteenth century, prisms were prescribed to be worn for the treatment of strabismus in a so called passive or in a so called active way [14]. In the former case, a prism corrected the strabismus angle and projected the image onto the central retinal fovea and, in doing so ensured bifoveal fusion and corrected strabismus. In the latter case, either a hypo- or a hypercorrection prism was prescribed, and the patient, as described by Voinov [14], if capable of merging double images into a single image through unassisted exercises of his muscles, overcame the load imposed on his ocular fusion system. This contributed to the improvement in fusional amplitude [14]. Although the prismatic approach to correction of strabismus lost some favor with the advent of special equipment for orthoptic treatment, reports on successful prescription of prisms as a treatment for the disease reappeared in the thirties of the twentieth century [15]. At that time, the use of prismatic correction was limited by the thickness of the lenses for correcting a strabismus angle of more than 10?, which were rather heavy and caused significant aberrations. These difficulties were eliminated with the introduction of Fresnel prisms [16] into practice. The development of elastic Fresnel prisms is considered a real breakthrough, and became the basis for expanding opportunities for patients to benefit from prismatic correction. Initially, the Fresnel wafer prisms were designed to clip onto existing glasses. Subsequently, flexible membrane Fresnel prisms were proposed to press onto existing prescription lenses. Such a flexible membrane Fresnel prism with a power of 30 prism diopters (?) was 0.8 mm thick [17, 18]. In 1971, Adams and colleagues [19] demonstrated that optical distortions due to these prisms were significantly less than aberrations due to conventional glass prisms. However, the presence of the lines on the Fresnel prism may cause slight blurring of vision, and, therefore, the prisms cause some reduction in visual acuity (3% per prism diopter vs 2% per prism diopter due to conventional glass prisms) [19]. Despite some disadvantages, Fresnel prisms have gained favor rapidly.
In addition, prisms are used at the last stage of orthoptic treatment of strabismus for the development of the potential for fusion and binocular single vision [20]. Eyeglasses with Fresnel prisms are prescribed in children aged at least two years, when, according to current theories, the active development of the visual system (including that of binocular interactions) takes place, which promotes the early formation of normal binocular connections long before the surgical intervention at adult age.
In Ukraine, the issue of prism therapy for strabismus was resolved only as recently as in 2009, with the introduction of the technology for manufacture of spheroprismatic lenses that combine the features of prismatic and spherical lenses (including astigmatic lenses). The lens was designed as a conventional spherical polycarbonate lens, to which surface the Fresnel microprism with a required power was hermetically welded using ultrasound, with prism relief lines positioned inwards [21]. Spheroprismatic lenses are made individually based on the prescription, in any combination of the optic power of the two components: a spherical lens of 0 to ±8D, and a Fresnel prism with a power of 0 to 30?. Microprismatic components have a number of advantages compared to conventional glass prisms, with their immediate availability in powers up to 30? versus ? 5 ?, and lightness in weight (which is crucial for children). In addition, it does not matter on which of the two eyes the microprismatic component is put on. To reduce the weight and thickness of ocular lenses, the power of the ocular lens can be uniformly distributed among the lenses of glasses [22].
The study purpose was to investigate the effect of microprismatic glasses on the binocular function in children with strabismic amblyopia.
Materials and Methods
One hundred and forty nine strabismic amblyopia children with concomitant strabismus aged 4 to 18 years were included into the study. Concomitant esotropia and exotropia were found in 77 children and 11 children, respectively, of the study group, versus 54 children and 7 children, respectively, of the control group. Six children (6.8%) of the study group versus 13 children (21.3%) of the control group were those with partially accommodative strabismus, whereas the rest were those with non-accommodative strabismus. The angle of deviation (Hirschberg test) varied between 5° and 25° (10? and 50?) at near.
The control group comprised 61 strabismic amblyopia children (those with partially accommodative or non-accommodative concomitant esotropia or exotropia) who were treated with conventional therapy at an ocular health room. The group was subdivided into three approximately equal subgroups based on degree of amblyopia by Avetisov (low (corrected ametropy; VA range, 0.8 to 0.4), moderate (VA range, 0.3 to 0.2), and high (VA range, 0.1 to 0.05)).
The study group comprised 88 strabismic amblyopia children and was also subdivided into three subgroups based on degree of amblyopia by Avetisov (low, moderate and high amblyopia subgroups comprising 27 children, 29 children, and 32 children, respectively).
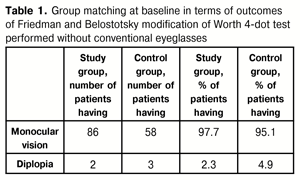
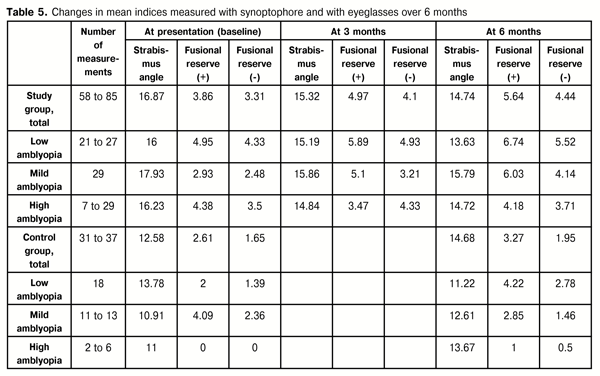
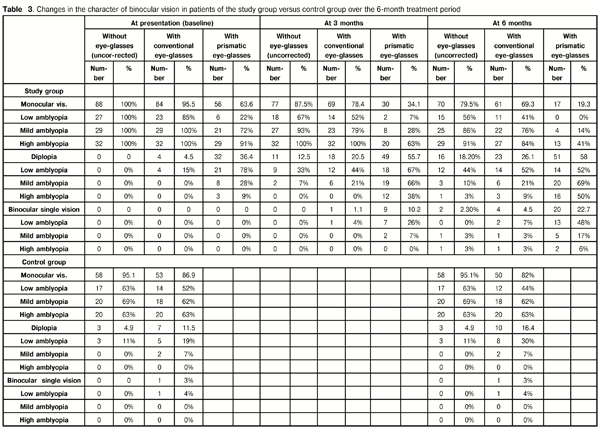
At baseline, we checked whether the study group and control group were matched in terms of the character of binocular vision (with uncorrected refractive errors or after correction for refractive errors). With uncorrected ametropia, monocular vision and diplopia were found in 86 children (97.7%) and 2 children (2.3%), respectively, of the study group, versus 58 children (95.1%) and 3 children (4.9%), respectively, of the control group (Table 1).
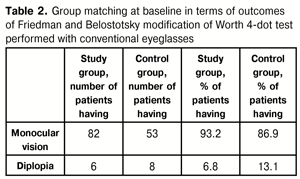
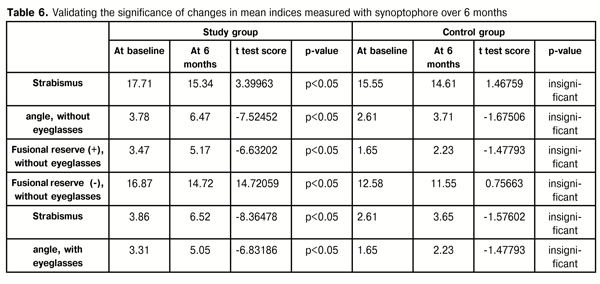
Although the baseline indices of binocular vision somewhat changed with correction of refractive errors, no substantial difference was found between the groups: monocular vision and diplopia were observed in 82 children (93.2%) and 6 children (6.8%), respectively, of the study group, versus 53 children (86.9%) and 8 children (13.1%), respectively, of the control group (Table 2). That is, with correction of ametropia, the number of children with diplopia in the study group and in the control group increased by 4 and 8, respectively.
At baseline, the groups were also compared for distribution of refractive errors. The numbers and percentages of low hyperopic, moderate hyperopic and high hyperopic eyes in the study group were 109 (61.9%), 44 (25.0%), and 13 (7.4%), respectively, against 46 (37.7%), 50 (41.0%) and 18 (14.8%), respectively, in the control group. The numbers and percentages of low myopic and moderate myopic eyes in the study group were 9 (5.1%) and 1 (0.6%), respectively, against 7 (5.7%) and 1 (0.8%), respectively, in the control group. However, the numbers and percentages of eyes with hyperopic astigmatism and those with myopic astigmatism in the study group were 62 (35.2%) and 7 (4.0%), respectively, against 80 (65.6%) and 6 (4.9%), respectively, in the control group.
Friedman and Belostotsky modification of Worth 4-dot test (with uncorrected ametropia and, subsequently, with correction for ametropia) was used to determine the character of vision in any of the two groups. In addition, modified Fresnel microprisms in conjunction with lenses for correction of ametropia were used for this purpose in the study group.
Special instruments (synoptophore and amblyocore), ocular exercises with special software games (“flower”, “cross”, “spider”), laser biostumulation with He-Ne laser SM-4, etc. were used for treatment of amblyopia in the control group. The duration of the instrument-based treatment course was 10 days. In addition, subsequently, treatment for this group included conventional occlusive therapy for strabismic amblyopia (covering the dominant eye with a patch for 2-3 hours a day depending on the degree of amblyopia in the strabismic eye). Visual acuity outcomes and binocular function outcomes were monitored at 6 months from commencing treatment.
Microprismatic glasses were used for treatment in the study group. In addition, in children with high degree of amblyopia, treatment included conventional occlusive therapy for strabismic amblyopia (covering the dominant eye with a patch for 2 hours a day). Binocular function outcomes were monitored at 3 months and 6 months from commencing treatment.
To achieve optical penalization (in order to encourage the use of the amblyopic eye), microprismatic glasses were prescribed with the maximum prism power for the dominant eye. The microprism power was distributed between the two eyes based on the principle of balance of visual acuity between them to encourage binocular vision.
Totally, 88 prescriptions were made, including those for prismatic glasses, spheroprismatic glasses, cylinder-prismatic glasses, and sphero-cylinder-prismatic glasses, in 33 cases, 32 cases, 12 cases and 11 cases, respectively (Figure 1).

Results
At baseline, with uncorrected ametropia, monocular vision and diplopia were found in 86 children (97.7%) and 2 children (2.3%), respectively, of the study group, versus 58 children (95.1%) and 3 children (4.9%), respectively, of the control group. The two children of the study group and the three children of the control group who had diplopia, were those with low degree of amblyopia, and made up 7.0% and 22.0%, respectively, of the relevant amblyopia subgroups. After adjustment for refractive errors, monocular vision and diplopia were found in 53 children (86.9%) and 8 children (13.1%), respectively, of the control group. Out of these 8 children with diplopia, 2 children and 6 children had low degree of amblyopia and mild degree of amblyopia, respectively, making up 22.0% and 7.0%, respectively, of the relevant amblyopia subgroups.
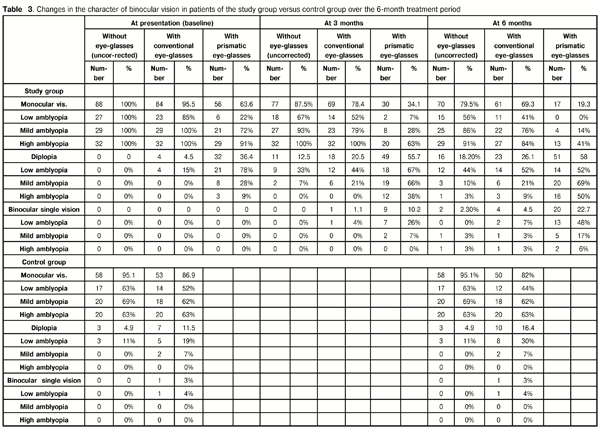
Following prescription of prismatic glasses for the children of the study group, the indices improved substantially. Monocular vision retained in 56 children (63.6%), and diplopia was found in 32 children (36.4%). Out of the latter children, 8 and 3 had mild and high degrees of amblyopia, respectively, making up 28.0% and 9.0% of the amblyopia subgroups.
At 3 months, with uncorrected ametropia, monocular vision and diplopia were found in 77 children (87.5%) and 11 children (12.5%), respectively, of the study group. Out of the latter children, 9 and 2 had low and mild degrees of amblyopia, respectively, making up 12.5% and 7.0% of the relevant amblyopia subgroups. After correction with conventional glasses for ametropia, diplopia was found in 18 children (20.5%) of the study group; in addition, binocular single vision was found in 1 child who had a low degree of amblyopia. After correction with prismatic glasses, monocular vision, diplopia and binocular single vision were found in 30 children (34.1%), 49 children (55.7%), and 9 children (10.2%), respectively, of the study group. Out of the latter children, 7 and 2 had low and mild degrees of amblyopia, respectively, making up 26.0% and 7.0% of the relevant amblyopia subgroups.
At 6 months, with uncorrected ametropia, diplopia and binocular single vision were present in 16 children (18.2%) and 2 children (2.3%), respectively, of the study group, whereas the rest of the children retained monocular vision. After correction with conventional glasses for ametropia, diplopia was found in 23 children (26.1%) of the study group. Out of these, 14, 6 and 3 had low, mild and high degrees of amblyopia, respectively, making up 52.0%, 21.0% and 9.0% of the relevant amblyopia subgroups. In addition, binocular single vision was reported in 4 children (4.5%). Out of these, 2, 1 and 1 had low, mild and high degrees of amblyopia, respectively, making up 7.0%, 3.0% and 3.0% of the relevant amblyopia subgroups.
At 6 months, after correction with prismatic glasses, diplopia was found in 51 children (58.0%) of the study group, showing a 21.6% increase compared to baseline. Moreover, among those with low, mild and high degrees of amblyopia, diplopia was present in 14, 20 and 16 patients, respectively, making up 52.0%, 69.0% and 50.0% of the relevant amblyopia subgroups. With uncorrected ametropia, binocular single vision was reported in 2 children (2.3%) of the study group, whereas after correction with conventional glasses, it was reported in 4 children (4.5%), of whom 2 had low degree of amblyopia and the rest had mild or high degree of amblyopia. After correction with prismatic glasses, the number of children with binocular single vision increased to 20 (22.7%). Out of these, 13, 5 and 2 had low, mild and high degrees of amblyopia, respectively, making up 48.0%, 17.0% and 6.0% of the relevant amblyopia subgroups.
Therefore, at 6 months, 20 children (22.7%) of the study group obtained binocular single vision versus only one child (3.0%) with low amblyopia of the control group. In addition, during the treatment period, with corrected ametropia, the number of children with diplopia in the control group increased from 8 (13.1%) to 10 (16.4%) (Table 3).
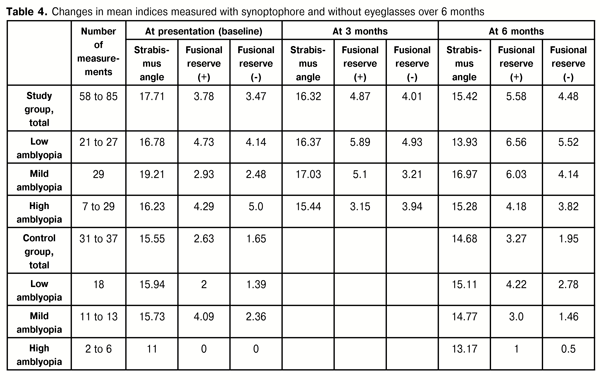
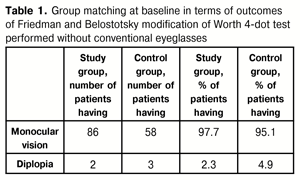
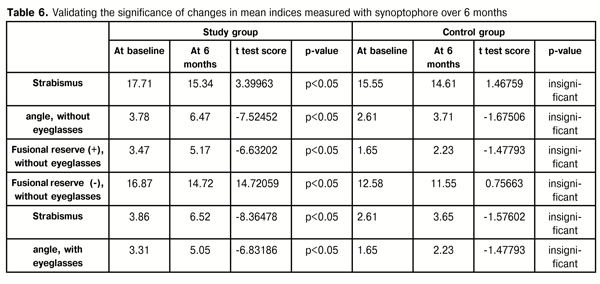
At baseline, mean fusion amplitude (with corrected or uncorrected ametropia) in the study group was 7.25 versus 4.28 in the control group. At 3 months, mean fusion amplitude in the study group increased to 8.88. In addition, at 6 months, mean fusion amplitude in the study group increased to 10.06, versus 5.22 in the control group. Interestingly, that in some cases of the study group or the control group, mean fusion amplitude values before treatment were better than those after treatment (Tables 4 and 5).
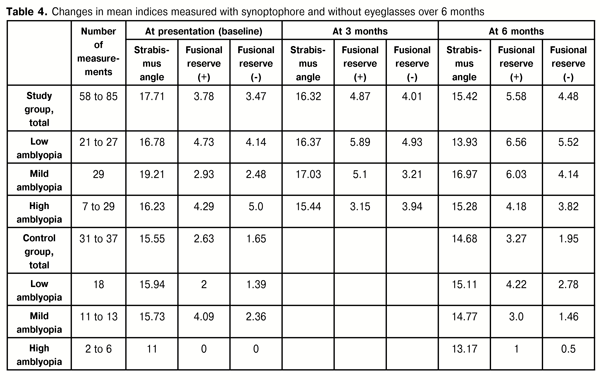
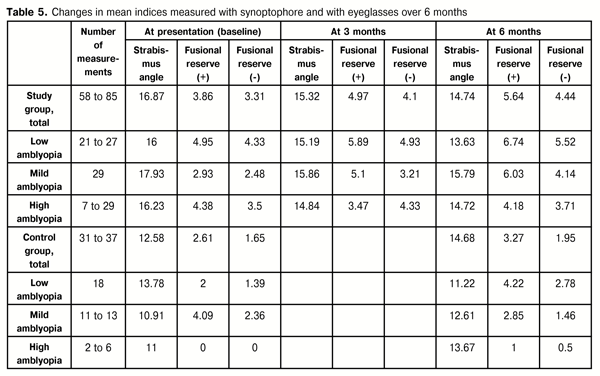
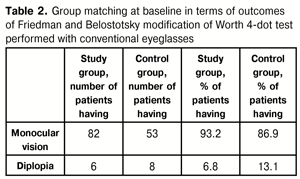
The paired t test was used to check for the significance of changes. A value of p < 0.05 was considered significant. It was found that changes in fusional reserves (with corrected or uncorrected ametropia) in the study group over treatment period were substantial and statistically significant, whereas changes in fusional reserves in the control group were insignificant in all the cases (Table 6).
Conclusions
First, in patients with strabismic amblyopia, wearing microprismatic glasses promotes improvement in binocular function due to prolonged action of pleoptics and orthoptics.
Second, the amount of changes in binocular function indicates that the period of treatment for strabismic amblyopia with these eyeglasses should be at least six months.
Finally, the treatment proposed for strabismic amblyopia (a) requires no additional time, (b) is suitable for patients, and (c) is more efficacious than conventional apparatus-based pleoptics-and-orthoptics therapy.
References
1. Abramov VG. [Common pediatric ocular diseases and their clinical features]. Moscow: Mobile; 1993 Russian
2. DeSantis D. Amblyopia. Pediatr Clin North Am. 2014 Jun;61(3):505-18
Crossref Pubmed
3. Granet DB, Khayali S. Amblyopia and strabismus. Pediatr Ann. 2011;40:89–94
Crossref Pubmed
4. Van de Graaf ES. Amblyopia and strabismus questionnaire: Rasch analysis. Invest Ophthalmol Vis Sci. 2010 Dec;51(12):6898
Crossref Pubmed
5. Avetisov SE, Kaschenko TP, Shamshinova AM, editors. [Ocular functions and their correction in children] Moscow: Meditsina; 2005 Russian
6. Smirnova IuV, Shishova OV, Smirnov KV. [Experience with complex treatment for childhood amblyopia]. Vestn Oftalmol. 2008 Jan-Feb;124(1):32-4 Russian
7. Ding J, Levi DM. Rebalancing binocular vision in amblyopia. Ophthalmic Physiol Opt. 2014 Mar;34(2):199-213
Crossref Pubmed
8. Pratt-Johnson JA, Tillson, G. Management of Strabismus and Amblyopia. A Practical Guide. 2nd ed. New York: Thieme Medical; 2001
9. Birch EE. Amblyopia and binocular vision. Prog Retin Eye Res. 2013 Mar;33:67-84
Crossref Pubmed
10. Bhola R, Keech RV, Kutschke P, et al. Recurrence of amblyopia after occlusion therapy. Ophthalmology. 2006 Nov;113(11):2097-100
11. Flynn JT, Schiffman J, Feuer W, Corona A. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of published studies. Trans Am Ophthalmol Soc. 1998; 96: 431–53
12. Wallace DK, Pediatric Eye Disease Investigator Group, Edwards AR, Cotter SA, et al. Ophthalmology. 2006 Jun;113(6):904-12
13. A randomized trial of increasing patching for amblyopia. Pediatric Eye Disease Investigator Group, Wallace DK, Lazar EL, Holmes JM, et al. Ophthalmology. 2013 Nov;120(11):2270-7
14. Voinov MM. [Ocular motility abnormalities]. St Petersburg: Glavnyi Voenno-Meditsinskii Departament; 1873 Russian
15. Evens L. History of strabismus treatment. Bull Soc Belge Ophtalmol. 1981;195:19-52
16. M?nchow W. [History of strabismus therapy]. Klin Monbl Augenheilkd. 1973 Mar;162(3):413-22 German
17. Moore S, Stockbridge L. An evaluation of the use of Fresnel press-on prisms in childhood strabismus. Am Orthopt J. 1975;25:62–6
18. Dal Fiume E, Navarra R. [Prismatic correction of small residual angles of strabismus]. Minerva Oftalmol. 1966 May-Jun;8(3):68-70 Italian
19. Adams AJ, Kapash RJ, Barkan E. Visual performance and optical properties of Fresnel membrane prisms. Am J Optom Arch Am Acad Optom. 1971 Apr;48(4):289-97
20. Avetisov SE, Kaschenko TP, Rozenblium IuZ, Friedman SIa. [Use of prisms in ophthalmology. Prisms in treatment of strabismus and ocular muscle palsy. Special methods of using prisms]. Vestn Oftalmol. 1973 Sep-Oct;5:86-90 Russian
21. Petrov VV, Kriuchyn AA, Rykov SO, Serhiienko MM, Antonov YeYe, Mellina VB, Shanoilo SM, Shevkolenko MV: inventors; Institute for Information Recording of the NAS of Ukraine, assignee. [Combined microprysm lens]. Patent of Ukraine № 46750 A 61 В 3/08. 2010 Jan 11. Ukrainian
22. Butenko LV, Iegupova LI. [Development and use of advanced Fresnel microprisms for diagnosis and treatment of pediatric strabismus]. Reiestratsiia, zberigannia I obrobka danykh. 2010; 1:67-72 Ukrainian